When Medicare approves your home health services, you may pay nothing for home health care services, though you may be responsible for 20 percent of the Medicare-approved amount for durable medical equipment (DME), which may include physical therapy supplies, wound care supplies, and assistive devices.
How much does Medicare pay for home health care?
Jun 20, 2019 · If you qualify for home health care under Medicare, you generally don’t have to pay any coinsurance or copayment. If you need durable medical equipment, you’ll typically pay 20% of the Medicare-approved amount as coinsurance. Read more about Medicare and durable medical equipment. When does Medicare not cover in-home health care?
Does Medicaid pay for in-home care?
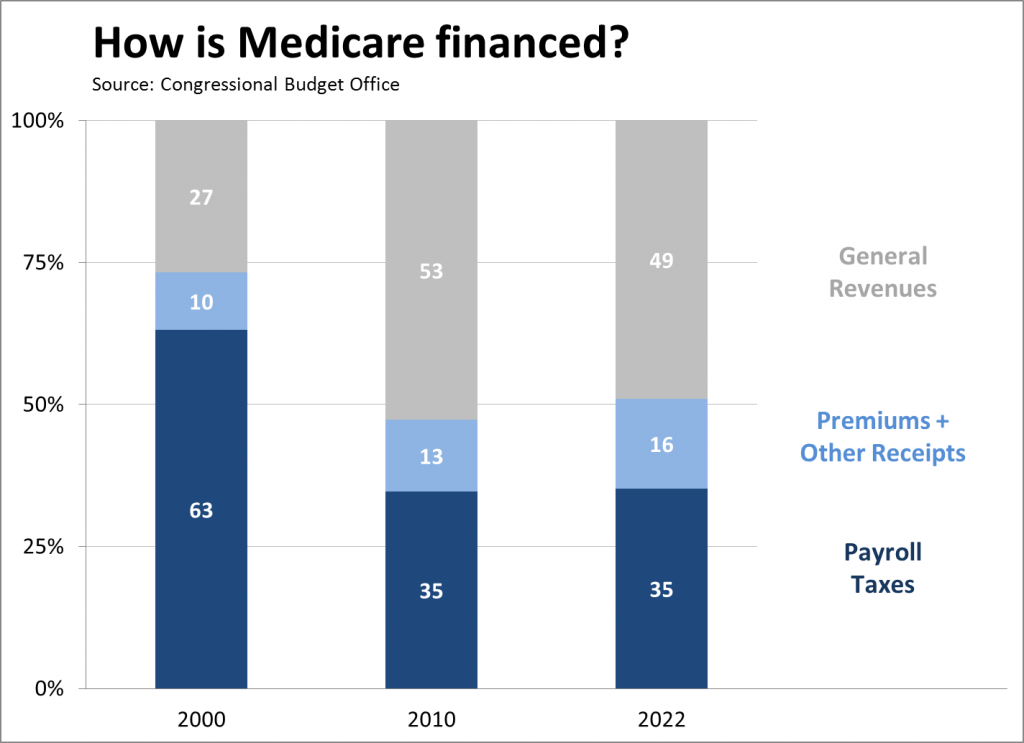
If you don’t qualify for a premium-free Part A, you might be able to buy it. In 2022, the premium is either $274 or $499 each month, depending on how long you or your spouse worked and paid Medicare taxes. You also have to sign up for Part B to buy Part A.
How much does in-home care cost per month?
Jan 06, 2022 · The services themselves will cost you zero dollars out of pocket (aside from whatever deductibles and copayments you pay for your Medicare plan). The only extra cost you’ll have for home health services is 20 percent of whatever durable medical equipment is …
Does Medicare Part B cover home health care?
Feb 14, 2020 · If you have Original Medicare, you are fully covered for a stay up to 20 days. After the 20th day, you will be responsible for a co-insurance payment for each day at a rate of $176 per day. Once you have reached 100 days, the cost of care for each day after is your responsibility and Medicare provides no coverage.
Does Medicare pay for help around the house?
How do I get my $144 back from Medicare?
How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
Which of the three types of care in the nursing home will Medicare pay for?
Is there really a $16728 Social Security bonus?
Will Social Security get a $200 raise in 2021?
Who qualifies as a caregiver under Medicare rules?
- You must be under the care of a doctor, and you must be getting services under a plan of care created and reviewed regularly by a doctor.
- You must need, and a doctor must certify that you need, one or more of these: ...
- You must be homebound, and a doctor must certify that you're.
What does Medicare Part B cover in a nursing home?
Part A covers inpatient hospital care, skilled nursing facility care, and hospice stays. Part B provides coverage for outpatient services, such as visits to a doctor's office, durable medical equipment, therapeutic services, and some limited prescription medication.
Which type of care is not covered by Medicare?
What is the average cost of a nursing home by state?
When Medicare runs out what happens?
How much does a nursing home cost?
What Is Home Health Care?
Home health care can involve a wide range of services you may need when you’re ill or recovering from an illness or surgery. In some cases it can i...
In-Home Care: Medical and Non-Medical
Depending on what is available in your community, home care can include: 1. Health care – skilled nursing care; physical, speech, occupational and...
Does Medicare Cover Home Health Care?
Medicare Part A and/or Part B may help pay for your home health care if these conditions apply to you: 1. You’re under the care of a doctor who acc...
Home Health Care and Medicare Supplement Insurance
You might have to pay a coinsurance amount in some cases; for example, under Medicare Part B, you usually pay 20% of durable medical equipment cost...
Not All Home Health Care Agencies Are Created Equal
Home health agencies vary in the services they offer, and not every agency is certified by Medicare. You may want to match your needs with the serv...
Does Medicare cover in-home care?
When might Medicare cover in-home health care? In general, Medicare doesn’t cover long- term home health care. Here’s how Medicare coverage of in-home health care typically works. In most cases, even when Medicare covers in-home health care, it’s for part-time care, and for a limited time.
Do you have to pay Medicare Part B premium?
Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending. You’ll need to keep paying your Medicare Part B premium (along with any premium the plan may charge) when you have a Medicare Advantage plan.
Does Medicare Advantage have a deductible?
Medicare Advantage plans may have annual deductibles, and may charge coinsurance or copayments for these services. Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending.
What is home health aide?
Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom. Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
What is round the clock care?
In-home meals (delivered to your home) Round-the-clock care (24 hours a day) Homemaker services , like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How much does nursing home care cost?
Nursing home care can cost tens of thousands of dollars per year for basic care, but some nursing homes that provide intensive care can easily cost over $100,000 per year or more. How Much Does Medicare Pay for Nursing Home Care?
Does Medicare cover nursing home care?
While Medicare benefits do help recipients with the cost of routine doctor visits, hospital bills and prescription drugs, the program is limited in its coverage of nursing home care. This is because nursing home care varies greatly in terms of scope and amenities.
How long does Medicare cover you?
If you have Original Medicare, you are fully covered for a stay up to 20 days. After the 20th day, you will be responsible for a co-insurance payment for each day at a rate of $176 per day. Once you have reached 100 days, the cost of care for each day after is your responsibility and Medicare provides no coverage.
Is Medicare good or bad for seniors?
For seniors and qualifying individuals with Medicare benefits, there’s some good news and some bad news. While Medicare benefits do help recipients with the cost of routine doctor visits, hospital bills and prescription drugs, the program is limited in its coverage of nursing home care.
How much does home health care cost?
In 2018, it was estimated that the average cost for non-medical home care was somewhere around $21.00 per hour and could go as high as $27.50 per hour – making it difficult for most seniors to afford. Thus, you may want to try Medicare to help cover costs.
Does Medicare cover homemaker services?
Medicare can pay for a range of home health care services, including equipment, physical therapy, supplies, and nursing and doctor’s care. That said, occupational therapy, homemaker services, and personal care get no coverage. If you’re caring for a senior parent or loved one and you’re looking into Medicare for the first time, ...
Does Medicare cover skilled therapy?
Occupational therapy, speech therapy, and physical therapy by a licensed therapist all count as skilled therapy services. More than likely, Medicare will cover the costs under your insurance plan so a senior can get the therapy they need.
Does Medicare cover dental care?
Medicare does not cover things like long term care, routine foot care, dental care and dentures, eye exams for prescribing glasses, or hearing aides, even if they are necessary for someone who is receiving home health care.
What is Medicare Part A?
With some exceptions, Medicare Part A is hospital insurance and it covers services such as: Hospice care. Home health care. Non-custodial, non-long term care in a skilled nursing facility. Inpatient hospital care. Medicare Part A usually lacks a monthly premium for most people who are age 65:
Does Medicare Part A have a monthly premium?
Non-custodial, non-long term care in a skilled nursing facility. Inpatient hospital care. Medicare Part A usually lacks a monthly premium for most people who are age 65: Those who get it premium-free are people who get Social Security retirement benefits or retirement benefits from the Railroad Benefit Board.
What is a DME?
Durable Medical Equipment (DME) Durable medical equipment (DME) is defined by Medicare as: durable. used for a medical reason. will be used in your home. is not something that is usually used by someone who is not injured or sick. has a general lifetime of at least three years.
Does Medicare cover nursing home care?
Medicare generally doesn't cover Long-term care stays in a nursing home. Even if Medicare doesn’t cover your nursing home care, you’ll still need Medicare for hospital care, doctor services, and medical supplies while you’re in the nursing home.
Do nursing homes accept Medicaid?
Most, but not all, nursing homes accept Medicaid payment. Even if you pay out-of-pocket or with long-term care insurance, you may eventually "spend down" your assets while you’re at the nursing home, so it’s good to know if the nursing home you chose will accept Medicaid. Medicaid programs vary from state to state.
Does long term care insurance cover nursing home care?
Long-term care insurance can vary widely. Some policies may cover only nursing home care, while others may include coverage for a range of services, like adult day care, assisted living, medical equipment, and informal home care. If you have long-term care insurance, check your policy or call the insurance company to find out if ...
How to find out if you have long term care insurance?
If you have long-term care insurance, check your policy or call the insurance company to find out if the care you need is covered. If you're shopping for long-term care insurance, find out which types of long-term care services and facilities the different policies cover.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Does Medicaid pay for nursing home care?
Yes, Medicaid will pay for in-home care, and does so in one form or another, in all 50 states. Traditionally, Medicaid has, and still continues to, pay for nursing home care for persons who demonstrate a functional and financial need. However, in-home care provides an alternative for seniors who require assistance to remain living at home, ...
What is HCBS waiver?
HCBS Medicaid Waivers. Home and Community Based Services Medicaid wa ivers, also known as Section 1915 (c) waivers, are another way in which Medicaid offers in-home services and supports to promote independent living of elderly persons.
What is a CFC in healthcare?
One such alternative, made possible by the Affordable Care Act, is the Community First Choice (CFC) option. CFC allows states to offer in-home personal attendant services to assist with one’s activities of daily living (ADLs) ...
What is a 1915 C waiver?
Home and Community Based Services Medicaid waivers, also known as Section 1915 (c) waivers, are another way in which Medicaid offers in-home services and supports to promote independent living of elderly persons.
What are some examples of planning strategies?
There are also planning strategies, such as Miller Trusts, Medicaid asset protection trusts, irrevocable funeral trusts and annuities, that can be implemented in order for one to meet the financial eligibility criteria.
What is functional need?
A functional need threshold, also referred to as medical need, must also be met in order for one to be eligible for in-home care . For the state Medicaid plan (regular Medicaid), persons often must demonstrate the need for assistance with activities of daily living and / or instrumental activities of daily living.
What is home care?
Home care services, also called personal care, attendant care, companion care or non-medical care, is limited to helping with the activities of daily living. Some care services provided by non-medical home care attendants include housekeeping, transportation for errands and medical appointments, meal planning and preparation, toileting and grooming.
Do you have to live within the service area of Medicare Advantage?
To qualify for Medicare Advantage, applicants must be eligible for traditional Medicare, and they must live within the service area of the plan they choose. In most cases, with the exception being seniors with very low income, enrollees pay the Medicare Part B monthly premium.
What is home care for seniors?
For some seniors, living at home requires a helping hand with some activities of daily living. In these cases, home care provides a balance between preserving privacy and independence and having needs met efficiently. Home care can range between highly specialized care, such as visits from a neurologist, to generalized care and companionship. It can be broken down into three categories, including home health care, non-medical home care and in-home services.
What is home health aide?
Home health care, which may also be referred to as home health aide services, addresses the needs of seniors who require regular health monitoring. Home health aides, also called geriatric aides, certified nursing assistants or nurse aides, are certified or licensed to provide specialized care such as checking patients’ respiration, pulse and temperature. They may also provide assistance with medical equipment like braces or ventilators, provide wound care, change catheters and administer medications. Along with skilled nursing services, home health aides may provide personal care services like help with bathing, dressing and toileting.
Does Medicare cover personal care?
Under traditional Medicare, there is no coverage for non-medical care, and any personal care services are paid for in full by the one receiving them. However, under the recently expanded Medicare Advantage program, seniors may be eligible to have some services covered.
What is Medicare Advantage?
In October 2018, the Centers for Medicare and Medicaid Services approved new Medicare Advantage guidelines that allowed a greater degree of flexibility for enhanced quality of life, including expanded coverage for home care. The purpose of this is to allow seniors to continue living at home as long as possible. Previously, coverage for home health care services was limited to skilled nursing care. Now, some Medicare Advantage plans cover services like housekeeping and laundry, meal delivery, ride-share for medical appointments and aides to help with the activities of daily living.
Why is aging in place important?
For many seniors and families, aging in place isn’t just about enjoying the ability to embrace the security and familiarity of home, but it’s also a financially economical option. According to the U.S. Department of Housing and Urban Development, aging in place saves money, particularly for seniors who own their homes outright and are no longer paying on a mortgage. Older adults who own their homes spend less on living expenses and are able to access their home’s equity to pay for in-home mobility devices and personal care services.