You may be eligible for up to 2 screenings each year. Part B covers these screenings if you have any of these risk factors: High blood pressure (hypertension) History of abnormal cholesterol and triglyceride levels (dyslipidemia) Obesity History of high blood sugar (glucose)
Full Answer
How much does CPT code 83036 cost with Medicare?
Medicare reimbursement for CPT codes 83036 and 83036QW is $13.42 in all states except: Idaho: $9.66 Maryland: $12.66 Oklahoma: $11.95 Rhode Island: $12.09 South Dakota: $12.86 Wyoming: $10.49 Diagnosis (ICD-9) Codes
When did CMS set the payment for code 83037?
• For calendar year 2007, CMS set the payment for code 83037 by crosswalking it to code 82985 (Glycated protein). • For tests furnished on or after April 1, 2008, the payment for 83037 or 83037QW will be the same as the payment on the clinical laboratory fee schedule for 83036.
What is the cost of 83036 QW hemoglobin?
83036QW Hemoglobin; glycated (A1c) using CLIA waived method Medicare reimbursement for CPT codes 83036 and 83036QW is $13.42 in all states except: Idaho: $9.66 Maryland: $12.66 Oklahoma: $11.95 Rhode Island: $12.09 South Dakota: $12.86 Wyoming: $10.49
What is the CPT code for glycosylated protein 83037?
CPT code 83036, glycosylated (A1c), already existed and was priced at $13.56 on the clinical laboratory fee schedule. • For calendar year 2006, CMS determined that code 83037 should be paid via carrier gap filling. • For calendar year 2007, CMS set the payment for code 83037 by crosswalking it to code 82985 (Glycated protein).
How often does Medicare allow an A1c test?
You may be eligible for up to 2 screenings each year.
How often can you bill an A1c?
For beneficiaries with stable glycemic control (defined as 2 consecutive HbA1c results meeting the treatment goals) performing the HbA1c test at least 2 times a year may be considered reasonable and necessary.
Does Medicare cover 83036?
(2) the service must be medically necessary or indicated. Once these two criteria are met, Medicare pays for most clinical laboratory tests based on the Laboratory Fee Schedule.
What diagnosis covers A1c for Medicare?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
What are the new guidelines for A1C?
ADA now recommends A1C below 7% or TIR above 70%, and time below range lower than 4% for most adults. In previous years, the Standards of Care included an “A1C Testing” subsection that recommended people with diabetes test their A1C two to four times a year with an A1C target below 7%.
What diagnosis will cover 83036?
Diabetes Hemoglobin A1c Testing Claims including procedure code 83036 or 83037 should include a line item with the resulting CPT procedure code below and be billed with a zero charge.
Does 83036 require a modifier?
CPT 83036 requieres a CLIA certificate and the QW modifier can be used.
What is included in CPT code 83036?
Group 1CodeDescription83036HEMOGLOBIN; GLYCOSYLATED (A1C)
How many diabetic test strips will Medicare pay for?
If you don't use insulin, you may be able to get 100 test strips and 100 lancets every 3 months. If your doctor says it's medically necessary, and if other qualifications and documentation requirements are met, Medicare will allow you to get additional test strips and lancets.
Does Medicare cover A1c for pre diabetes?
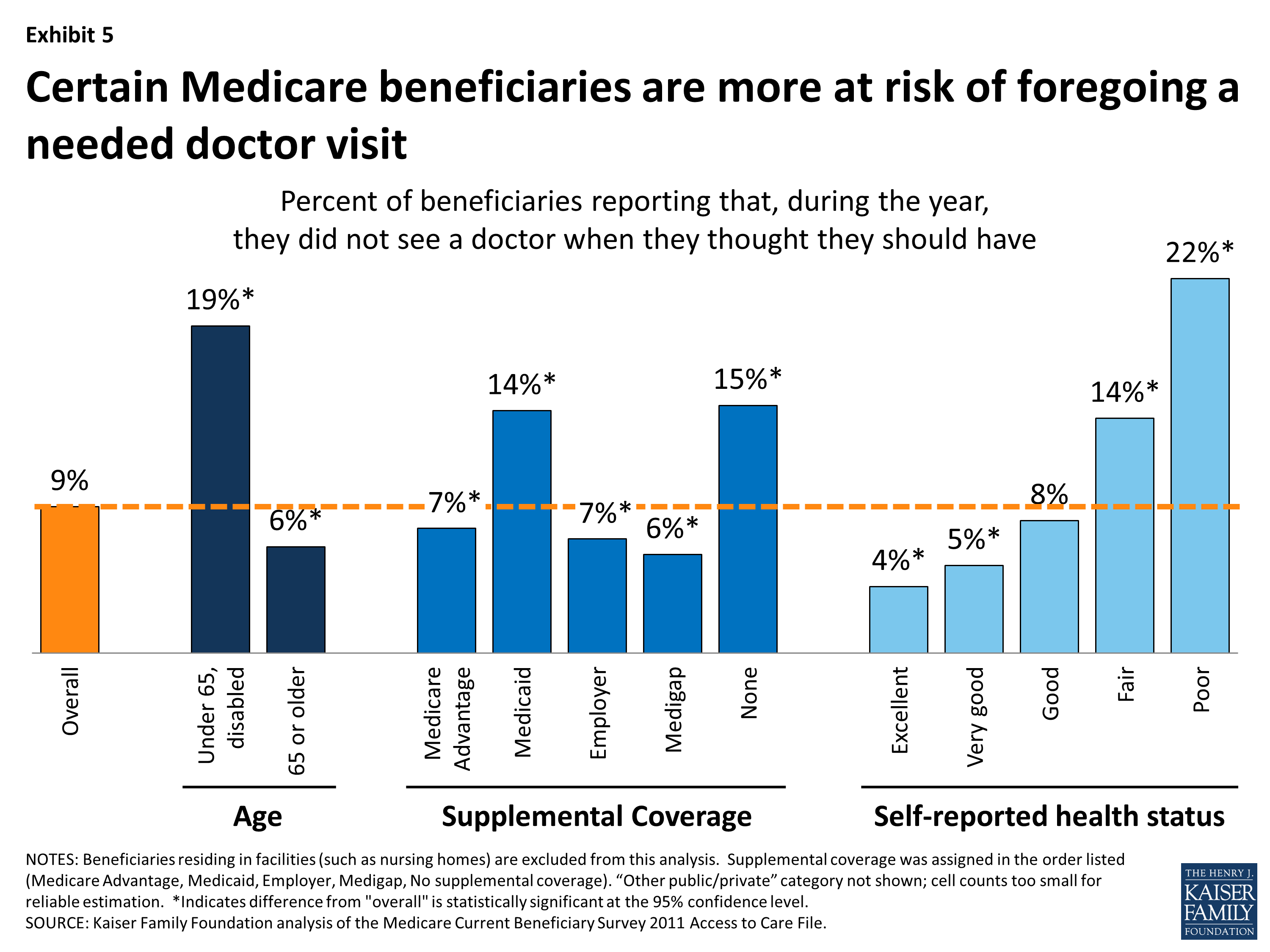
(Note that the Hemoglobin A1c is not currently covered by Medicare for pre-diabetes screening).
What ICD-10 code covers hemoglobin A1c screening?
1.
Does Medicare pay for diabetic medication?
You can also visit Medicare.gov/what-medicare-covers to view the information in the chart. Part D covers anti-diabetic drugs for maintaining blood sugar (glucose). Part B covers these screenings if your doctor determines you're at risk for diabetes. You may be eligible for up to 2 diabetes screenings each year.
What are the requirements for Medicare to pay for a diagnostic test?
Before Medicare pays for any test or diagnostic service, two basic criteria must be met: (1) the service must be covered by Medicare (e.g. , certain procedures such as routine screening tests are not covered) and. (2) the service must be medically necessary or indicated.
Can ICD-9 codes be assigned?
Definitive ICD-9 codes should only be assigned and recorded in the medical record after a diagnosis is clearly determined. Terms such as “rule out”, “probable”, and “suspected” should NOT be used since they can not be coded as such and may be interpreted as a firm diagnosis by a third party payer.
Does Medicare pay for labs?
Medicare payment for clinical laboratory tests is always the lesser of the fee schedule amount or the actual amount billed. The provider must accept the Medicare reimbursement as payment in full for a laboratory test. Medicare patients may NOT be billed for any additional amounts.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1862 (a) (1) (A) allows coverage and payment for only those services are considered to be reasonable and necessary for the diagnosis or treatment of illness or to improve the functioning of a malformed body member. CMS Internet-Only Manual, Pub.
Coverage Guidance
Hemoglobin A1c (HbA1c) refers to the major component of hemoglobin A1. Performance of the HbA1c test at least 2 times a year in patients who are meeting treatment goals and who have stable glycemic control is supported by the American Diabetes Association Standards of Medical Care in Diabetes - 2016 (ADA Standards).
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
When will Medicare start paying for insulin?
Insulin savings through the Part D Senior Savings Model. Starting January 1, 2021, you may be able to get Medicare drug coverage that offers broad access to many types of insulin for no more than $35 for a month's supply.
Does Medicare cover blood sugar screening?
A history of high blood sugar (glucose) Medicare also covers these screenings if 2 or more of these apply to you: You’re age 65 or older. You’re overweight. You have a family history of diabetes (parents or siblings).
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
Coding Analyses for Labs (CALs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with CALs, from the Coding Analyses for Labs database.