A person is eligible for an initial physical examination within the first 12 months of Medicare enrollment. After that time, they are eligible for an annual wellness visit once every 12 months. Medicare has different terms for physical exams and specific rules around them.
Why Medicare does not cover the annual physical exam?
Jun 25, 2019 · Yearly Wellness Visit. Your Medicare Part B coverage includes preventive services, including an annual wellness visit. Once you have had Medicare Part B for 12 months, you are eligible for this annual check-up. It does not cost anything if the health care provider doing your exam accepts Medicare assignment.
Does Medicare cover an annual physical?
Will Medicare pay for a yearly physical examination? En español | Medicare does not pay for the type of comprehensive exam that most people think of as a “physical.” But it does cover a one-time “Welcome to Medicare” checkup during your first year after enrolling in Part B and, later on, an annual wellness visit that is intended to keep track of your health.
Does Medicare cover annual physical exams?
Nov 23, 2020 · The one-time “Welcome to Medicare” preventive visit is not a prerequisite for the yearly wellness visit, but the annual cannot occur until you have passed the 12-month mark for Part B enrollment. Medicare physical exams. Original Medicare does …
Does Medicare pay for a yearly physical examination?
A person is eligible for one initial preventive physical examination (IPPE), also known as a Welcome to Medicare physical exam, within the first 12 months of enrolling in Medicare Part B.
How often does Medicare require a physical?
Does Medicare make you have a physical every year?
How often can you have a Medicare Annual Wellness visit?
How many preventive physical exams does Medicare cover?
What is the difference between a Medicare wellness exam and a physical?
What is the difference between an annual physical and a wellness exam?
An annual physical is focused on detecting any developing medical issues through a series of lab tests. On the other hand, a wellness exam guides you on how to make healthy lifestyle decisions and prevent common medical complications.Aug 21, 2020
How often does Medicare pay for routine blood work?
Is a yearly physical necessary?
Does Medicare wellness exam include blood work?
What is not covered in Medicare Annual Wellness visit?
Your doctor or other health care provider performs additional tests or services during the same visit. Medicare doesn't cover these additional tests or services under this preventive benefit.
Can I refuse the Medicare Annual Wellness visit?
Do Medicare wellness visits need to be 12 months apart?
Does Medicare cover physicals?
But make sure that you ask specifically for "Welcome to Medicare" or annual wellness visit by name. If you ask for a “physical,” Medicare will not cover it and you’ll be responsible for whatever the doctor charges.
How to get Medicare?
Initial visit: The “Welcome to Medicare” visit with your doctor aims to establish the state of your health when you enter the program and provide a plan of future care. The doctor will: 1 record your vital information (height, weight, blood pressure, body mass) 2 review your personal and family health history 3 check risk factors that could indicate future serious illnesses 4 recommend tests and screenings that could catch medical issues early and provide a checklist of preventive services (such as mammograms and vaccinations) to help you stay healthy 5 offer you the option of discussing end-of-life issues, including information on how to prepare an advance directive naming someone to make medical decisions on your behalf if you became too ill to make them yourself 6 provide counseling and referrals as appropriate
What does "assignment" mean in Medicare?
You’re enrolled in original Medicare (Part A and Part B) and you see a doctor who accepts “assignment” — meaning he or she accepts the Medicare-approved payment as full compensation. You’re enrolled in a Medicare Advantage (Part C) plan and see a doctor in the plan’s provider network.
What is an annual wellness visit?
Annual visit: During an annual wellness visit, the doctor measures your height, weight, body mass and blood pressure, and may listen to your heart through your clothes. The rest is a discussion of your own and your family’s medical history, any physical or mental impairments, and risk factors for diseases such as diabetes and depression.
Does Medicare cover physicals?
Routine physical examinations. Medicare does not cover a routine physical examination. Plans usually provide coverage for the following: Medicare will often consider anything other than these types of visits to be a routine physical examination, which they will not usually cover.
Does Medicare cover annual wellness visits?
Annual Wellness Visit (AWV) Medicare Part B covers yearly wellness visits, as it is the portion of Medicare that includes medical (usually nonhospital) services. The coverage of these wellness visits comes at no extra cost, as long as the medical provider accepts assignment.
Does Medicare cover preventive care?
While Medicare mainly covers the cost of diagnostic care and medical treatment, coverage sometimes also includes preventive services. Medicare mostly covers healthcare services to diagnose and treat medical conditions. However, there are times when Medicare does cover preventive services, such as annual wellness visits.
How often does Medicare cover AWV?
health educator, registered dietitian, or other health professionals whom a doctor directly supervises. Medicare will cover an AWV once every 12 months. The services that a doctor may perform include: setting up a personal prevention plan.
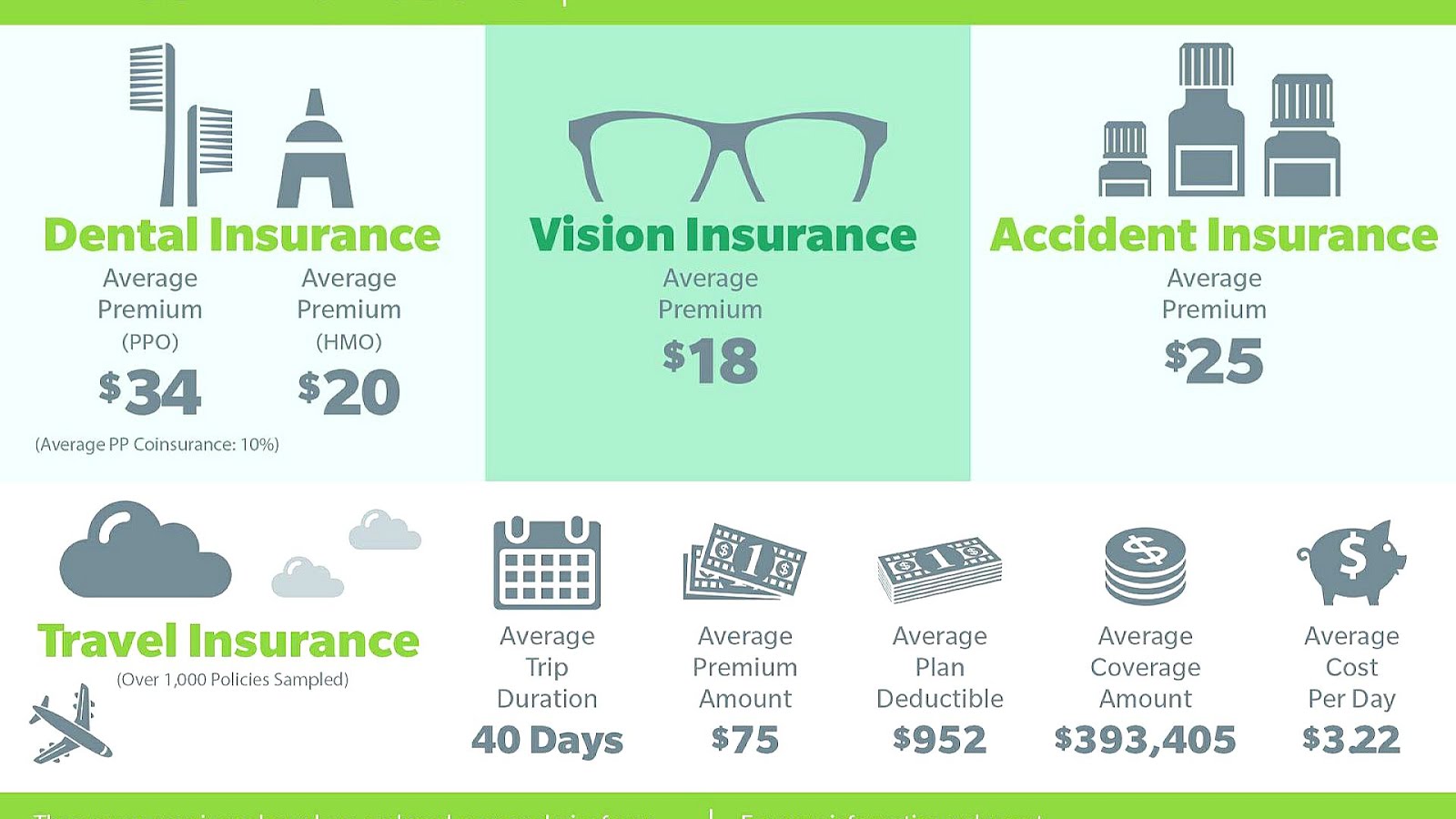
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
Does Medicare pay for physical therapy?
In the past, Medicare paid physical therapists based on the number of visits and the amount of time they spent with patients. To keep costs down and improve care, Medicare adopted a value-based approach to physical therapy.
How much does Medicare pay for speech therapy?
However, the threshold amount that Medicare pays for physical and speech therapy combined is $3,000 before reviewing a patient’s case to ensure medical necessity. Also, once a patient spends $2,080 on physical and speech therapy, providers add special billing codes to flag this amount.
Does physical therapy improve quality of life?
Whether you’re in an accident or you have a medical condition, therapy can improve the quality of life. If a doctor says that physical therapy will improve your quality of life, you can consider it necessary. In the context below, we’ll go into detail about when Medicare coverage applies, how often coverage applies, ...
What is the difference between Part A and Part B?
When physical therapy happens during or after hospitalization, Part A covers it. Part B pays for outpatient or at-home physical therapy. You may be responsible for part of the cost. You’ll obtain therapy in a hospital, skilled nursing facility, outpatient physical therapy center, or your home. Part A provides coverage for inpatient physical therapy.
What is Part B in a hospital?
Part B pays for outpatient or at-home physical therapy. You may be responsible for part of the cost. You’ll obtain therapy in a hospital, skilled nursing facility, outpatient physical therapy center, or your home. Part A provides coverage for inpatient physical therapy. If you’re in the hospital for at least three days, ...
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
How often do you get a wellness visit?
for longer than 12 months, you can get a yearly “Wellness” visit once every 12 months to develop or update a personalized prevention plan to help prevent disease and disability, based on your current health and risk factors.
What is a personalized prevention plan?
The personalized prevention plan is designed to help prevent disease and disability based on your current health and risk factors.
Does Medicare cover annual physicals?
Your doctor may also have performed head, neck, lung and abdominal exams as well as testing your reflexes and neurological responses. Medicare does not cover this kind of annual physical so your doctor will generally not cover these during your Annual Wellness Visit. If he does, then it may be billed as diagnostic.
Does Medicare require annual wellness visits?
The most common preventive care service is the Medicare Annual wellness visit. The Medicare Annual Wellness Visit is not mandatory. It is a medical visit that you can take advantage ...
Is a wellness visit mandatory for Medicare?
The Medicare Annual Wellness Visit is not mandatory. It is a medical visit that you can take advantage of voluntarily and free of charge. The wellness visit is intended to keep you in touch with your Medicare doctor and ensure that your doctor can help you with preventive care planning. Let’s take a look at what this particular appointment includes ...
What are the items covered by Medicare?
Here are some of the covered items that your Medicare doctor is likely to review with you during your first Medicare Annual Wellness Visit: Routine measurements. Height, weight and blood pressure check.
Does Medicare Advantage cover wellness visits?
Do Medicare Advantage plans cover the wellness visit? All Medicare Advantage plans must cover the same medical services as Original Medicare Parts A and B, so yes they will offer an annual wellness visit at no cost to you. Some Medicare Advantage plans also offer more comprehensive physical exams.
How often do you get a wellness visit?
You’ll be eligible for a wellness visit every year. After your first one, the subsequent wellness appointments will cover things that your doctor established as a baseline during your initial appointment. If you’ve had Part B for more than 12 months, you can get a wellness visit each year.
Who can perform a wellness visit?
Any doctor or practitioner recognized by Medicare can perform the wellness visit. This would include nurse practitioners, physician assistants, clinical nurse specialists, and other health professionals who are working under the supervision of a Medicare physician.
What are the requirements for a mental health exam?
You may also receive exams of certain aspects of your physical and mental health, such as: 1 Counseling about certain screenings or shots you may require 2 Height, weight, blood pressure, and body mass index measurements 3 A basic vision test 4 A review of your risk for depression 5 A written plan detailing what steps for preventive care you should take
What is Medicare Supplement?
A Medicare Supplement (Medigap) plan can help pay for your out-of-pocket Medicare costs for outpatient care ordered by your doctor or health care professional during a physical. Medicare Part B covers your Welcome to Medicare visit and yearly wellness visits.
How much is Medicare Part B deductible?
In 2019, the standard Medicare Part B deductible is $185 per year. Your Medicare Part B deductible must be paid before Medicare will begin paying its share of Medicare-approved services. Once your Part B deductible is met, Medicare pays 20 percent of the Medicare-approved amount for a service.
Who is Christian Worstell?
Or call 1-800-995-4219 to speak with a licensed insurance agent. Christian Worstell is a health care and policy writer for MedicareSupplement.com. He has written hundreds of articles helping people better understand their Medicare coverage options.
Does Medicare cover annual physicals?
While Medicare does not cover annual physical exams, it does cover a single "initial preventive physical examination," followed by exams called "annual wellness visits.
Is a routine physical exam covered by Medicare?
The Centers for Medicare & Medicaid Services (CMS) notes that a "routine physical examination" is not covered by Medicare.
How long does a physical exam last?
In defining the term, Dignity Health states, "A thorough physical examination covers head to toe and usually lasts about 30 minutes. It measures important vital signs — temperature, blood pressure, and heart rate — and evaluates your body using ...
What is an AWV visit?
Now onto the annual wellness visit, sometimes referred to as an AWV, which was established by the Affordable Care Act. As Medicare.gov notes, beneficiaries with Medicare Part B for longer than a year are eligible for the service once every 12 months. During these visits, a provider develops or updates a personalized prevention plan to help reduce the likelihood of disease and disability. The visit can include a wide range of services, such as medical and family history review, developing/updating current providers and prescriptions, gathering of routine measurements, treatment options for risk factors, and development of a screening schedule. Providers also ask patients to complete a health risk assessment (HRA) and may perform a cognitive impairment assessment to look for signs of Alzheimer's disease or dementia. Medicare patients pay nothing for the annual wellness visit.
Does a wellness visit include a physical?
The annual wellness visit generally doesn't include a physical exam, except to check routine measurements such as height, weight and blood pressure.".
What is an IPPE?
Finally, let's review the components of an initial preventive physical examination, also referred to as an IPPE or "Welcome to Medicare" preventive visit. This is a service provided to newly enrolled Medicare beneficiaries once within the first 12 months they are covered by Medicare Part B. As Medicare.gov notes, the visit includes a review of a patient's medical and social history concerning health and education and counseling about preventive services. Also included with this review: services such as health risk screenings, flu shots, and referrals for other care; routine measurements; body mass index calculation; vision test; evaluation of potential risk for depression; and a written plan outlining services needed. This visit is covered only once and only if it's performed within the 12 months of Part B enrollment.