Does Medicare cover sleep studies and CPAP machines?
Both your sleep study and CPAP machine will be covered by Medicare Part B, as long as your doctor and supplier participate in Medicare. Expect to pay a share of the costs under your Medicare Part B or Medicare Advantage plan.
How many times a year does Medicare pay for CPAP?
Below is a list of how many times per year Medicare will pay for a portion of certain CPAP supplies, according to the Department of Health and Human Services: humidifier water chamber: 2 times per year nondisposable filters: 2 times per year chinstrap: 2 times per year
Can a patient resume CPAP therapy after a sleep study?
If the patient wants to resume therapy, s/he must start the process over with a new face-to-face evaluation and in-center sleep study (home sleep testing is not sufficient). How does Medicare define CPAP compliance or adherence?
Do I need a new CPAP machine?
We’re asked this question on a daily basis. 1. You’re a CPAP user and would like a new machine. If your CPAP machine is more than a few years old, you may be interested in a new machine. Most insurances will cover a new CPAP every 3 to 5 years (learn more here ).
How many times will Medicare pay for a sleep study?
All four levels of sleep studies (Type I, Type II, Type III and Type IV) are covered by Medicare.
How often can I get a new CPAP machine on Medicare?
every 5 yearsMedicare will usually cover a new CPAP machine every 5 years! This is also how long most manufacturers estimate that a CPAP machine will last, so even if your machine seems to be working, it's a good idea to replace it before it breaks down.
How Long Does Medicare pay for CPAP machine?
13 monthsfor the machine rental and purchase of related supplies (like masks and tubing). Medicare pays the supplier to rent a CPAP machine for 13 months if you've been using it without interruption. After Medicare makes rental payments for 13 continuous months, you'll own the machine.
How often do you need to repeat a sleep study?
While there is no set time to repeat a sleep apnea test, many doctors recommend an updated test every 5 years. Returning sleep apnea symptoms, changes in lifestyle, or changes in CPAP therapy are good indicators that a new sleep study test is required.
How long is a CPAP prescription good for?
How Long Is My Prescription Valid? If your CPAP prescription mentions a “Life time Need” or says “99 months”, it's valid for as long as you need therapy. If your prescription shows an expiration date, it is valid until the date shown.
What is the Medicare approved amount for a CPAP machine?
How much does a CPAP machine cost with Medicare? If the average CPAP machine costs $850, and Medicare covers 80 percent of it, then you'll have to pay $170; however, you'll also have to account for the Medicare Part B deductible, which is $203 in 2021, meaning your total cost may be up to $373.
Does Medicare Part B pay for CPAP machine?
Original Medicare is made up of parts A (hospital insurance) and B (medical insurance). Medicare Part B is the section that pays for durable medical equipment (DME), such as CPAP machines.
Does ResMed accept Medicare?
Do you accept either Medicare or Medicaid? Medicare and Medicaid will pay for medical equipment and supplies only if a supplier has a Medicare or Medicaid supplier number. Expedite, LLC, the operator of the ResMed Shop, does not have a Medicare or Medicaid supplier number.
How do you qualify for a CPAP machine?
All patients with an apnea-hypopnea index (AHI) greater than 15 are considered eligible for CPAP, regardless of symptomatology. For patients with an AHI of 5-14.9, CPAP is indicated only if the patient has one of the following: excessive daytime sleepiness (EDS), hypertension, or cardiovascular disease.
How long are sleep study results valid?
For many patients, it will depend on your doctor's preferences as to when you should retest. Some physicians may require an annual test, and others may prefer a test every five years. One of the signs that you may need to retest is the return of your sleep apnea symptoms.
Why would I need a second sleep study?
For those more high-risk patients, a split-night study can help diagnosis and start treating sleep apnea immediately. Because the two-part process essentially enables clinicians to perform two studies in the same night, the average turnaround time from referral to treatment is shorter.
How do you know when you no longer need a CPAP?
Some of the tell-tale signs of a successful CPAP treatment are below:Your breathing when you sleep is continuous (uninterrupted)You don't find yourself waking up and gasping for air.You don't get headaches in the morning.You feel more rested throughout the day.You can focus on tasks more clearly.More items...•
Does Medicare Cover CPAP and Other Pap Therapy For Sleep Apnea?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn...
How Does Medicare Define CPAP Compliance Or Adherence?
Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period...
What Is The Rental Term For Pap Therapy?
If the 3-month trial is successful (see above) Medicare will continue to cover the PAP device on a rental basis for up to 13 months in total up to...
Will Medicare Cover CPAP If I had A Machine Before I Got Medicare?
Yes, Medicare may cover rental or a replacement CPAP machine and/or CPAP supplies if you meet certain requirements.
When Does Medicare Cover Bi-Level Or Bipap?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive...
What Is Required in The Initial Face-To-Face Clinical Evaluation?
Written entries of the evaluation may include:History 1. Signs and symptoms of sleep disordered breathing including snoring, daytime sleepiness, ob...
What Information Does Medicare Require on The Prescription For CPAP and Supplies?
1. Beneficiary/patient’s name 2. Treating physician’s name 3. Date of order 4. Detailed description of items (type of device and supplies, pressure...
How Often Does Medicare Cover Replacement Pap Supplies?
Here’s an outline of the Medicare supply replacement schedule. For more detail (including how to tell when your equipment needs to be replaced, che...
How Much Will Medicare Pay For A CPAP Or Other Pap Machine?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insuranc...
How long do you have to rent a medical machine?
to rent the machine for the 13 months if you’ve been using it without interruption. After you’ve rented the machine for 13 months , you own it.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is a Part B deductible?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. Medicare pays the. supplier.
Does Medicare cover CPAP machine rental?
If you had a CPAP machine before you got Medicare, Medicare may cover CPAP machine cost for replacement CPAP machine rental and/or CPAP accessories if you meet certain requirements.
How often do insurance companies cover CPAP?
Most insurances will cover a new CPAP every 3 to 5 years (learn more here ). In recent years, machines have become smaller, quieter and most now have wireless compliance monitoring so you can keep track of your progress (and no longer have to mail in your smart card if you need a compliance report ). In this case, your insurance company may require ...
Who is Julia from Advanced Sleep Medicine?
in 2011 with a background in sales, marketing and customer service. She is currently the vice president of marketing and operations and enjoys the opportunity to educate and interact with those looking to improve their health through better sleep.
Can you use HST and CPAP at the same time?
If, like many CPAP users, you dread the though of a night without your CPAP (you can’t use HST equipment and CPAP at the same time), you may prefer to go to the sleep center for a 50/50 or split night study (learn more about different sleep study types here ). 2.
Can you use bilevel CPAP at high pressure?
You want to try bilevel PAP therapy. If you are using CPAP at a high pressure or suspect that you may benefit from bilevel therapy, most insurance companies will require that you demonstrate CPAP intolerance during an overnight sleep study.
note
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like:
note
Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs.
Medicare Coverage for CPAP Machines
Caitlin McCormack Wrights has over a decade of experience writing hundreds of articles on all things finance. She specializes in insurance, mortgages, and investing and relishes making dull subject matter gripping and everyday topics amazing. Caitlin has a bachelor's from Duke and a master's from Princeton.
When Will Medicare Cover CPAP Machines?
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study.
How To Get Medicare To Cover a CPAP Machine
Medicare will cover a CPAP machine if you meet two conditions. You must first be diagnosed with obstructive sleep apnea, and you must submit your primary doctor’s order or prescription to the right supplier to receive coverage. Here are the steps you’ll need to take to make that happen.
How Much Does a CPAP Machine Cost With Medicare?
Medicare typically covers the most basic level of equipment, and it may not pay for upgrades. In the case where Medicare doesn’t cover upgrades or extra features, you’ll need to sign an Advance Beneficiary Notice (ABN) before you get the equipment.
The Bottom Line
The rules of how DMEs are covered, including CPAP machines, are generally the same whether you have Original Medicare or a Medicare Advantage Plan. However, the amount you pay with Original Medicare and a Medicare Advantage Plan may often differ. Compare Medicare and Medicare Advantage to learn more.
How often can I get a new CPAP machine while on Medicare?
Once you’ve continuously used your CPAP machine for the approved 13-month rental, you will own it. However, CPAP supplies may lose effectiveness with use, and Medicare covers their replacement. Guidelines suggest replacing a CPAP mask every three months and a non-disposable filter every six months. 4
How do I get CPAP supplies covered by Medicare?
Medicare will only help cover CPAP supplies and accessories if you get them from a Medicare-approved contract supplier after completing the necessary medical steps.
How much does Medicare cover for a CPAP machine?
After you pay the $185 yearly Part B deductible (for 2019), Medicare will cover 80% of the Medicare-approved rental costs of the CPAP machine for 3 months, ...
How long is a CPAP trial?
If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy. If the therapy is successful, your doctor can extend the treatment and Medicare will cover it.
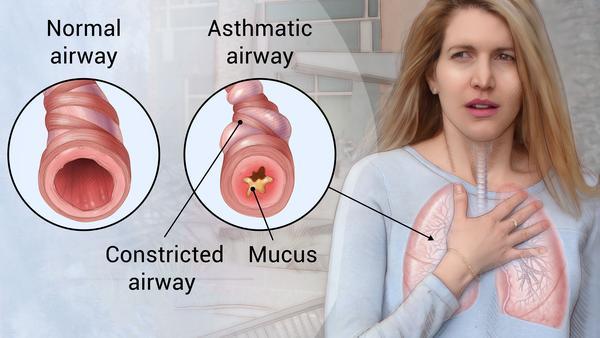
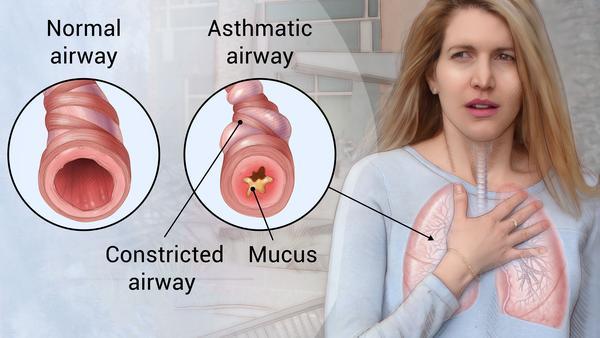
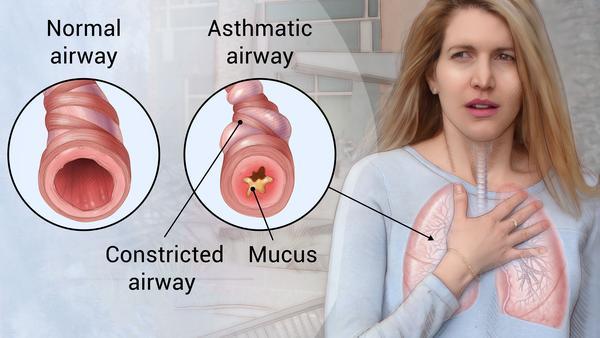
What is the best treatment for sleep apnea?
A continuous positive airway pressure (CPAP) machine is the most common treatment for moderate to severe sleep apnea. The machine is equipped with a mask that blows air into your throat while you are sleeping to keep your airway ...
How long does breathing pause last?
Breathing pauses from sleep apnea can last from several seconds to minutes and can occur over 30 times per hour. Sleep apnea is a chronic condition that disrupts your sleep and can lead to daytime sleepiness and more serious health conditions.
Does Medicare Supplement have a 20% deductible?
Depending on the Medicare Supplement insurance plan you choose, you could get full coverage for both the Part B deductible and the 20% Part B coinsurance cost. You can use the comparison chart below to see the benefits that are offered by each type of standardized Medigap plan sold in most states.
Can you take a prescription for a CPAP machine?
After you are approved for therapy, your doctor will give you a medical prescription for the CPAP machine. You can take this to any medical equipment supplier that accepts Medicare payments. If they accept Medicare, the supplier will bill Medicare directly for your Medicare-covered CPAP supplies.
Does Medicare cover CPAP?
Medicare does cover CPAP machine therapy if you are diagnosed with sleep apnea. You may be eligible for sleep apnea treatment options if you are enrolled in Medicare Part B and have been diagnosed with obstructive sleep apnea. If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy.
Medicare CPAP Compliance
Medicare can and will cover CPAP therapy for a three-month trial or longer, provided your doctor provides proper documentation that the treatment is helping you and that you meet specific requirements.
Does Medicare cover sleep studies?
Medicare Part B—the medical insurance portion—does cover Type I, II, III, and IV sleep tests and devices. Note that, like many other covered services, you’ll pay 20% of the Medicare-approved amount after you meet your Part B deductible. Doctors may require an at-home sleep apnea test.
How often will Medicare pay for a new CPAP machine?
Medicare will generally pay for CPAP machine replacement every five years. Medicare can also pay 80% of the cost for replacement supplies. The Part B deductible will still apply. Replacement supplies for CPAP machines include:
Are CPAP machines considered Durable Medical Equipment?
CPAP machines are considered Durable Medical Equipment (DME), which means that they’re covered by Medicare. DME must be durable, used for a medical reason and used in your home. DME should not be useful to someone who is well.
Are CPAP cleaners covered by Medicare?
Unlike CPAP machines themselves or their tubing, masks or replacement parts, CPAP cleaners aren’t covered by Medicare. Because CPAP cleaners and sanitizers aren’t considered DME, they’re not eligible for coverage. They can, however, be purchased with HSA/FSA funds.
Review your Medicare Coverage with SelectQuote
If your doctor has ordered a sleep test and/or CPAP therapy for sleep apnea, you’ll want to be sure that your Medicare coverage can help pay for your treatment and medical care. If you have questions about Medicare or would like a licensed insurance agent to help review your current coverage, SelectQuote can help.
How often does Medicare pay for CPAP?
nondisposable filters: 2 times per year. chinstrap: 2 times per year.
How long can you rent a CPAP machine?
CPAP rental for 13 months if you’ve been using it consistently (after 13 months , you’ll own the CPAP machine) masks or nose pieces you wear when using the machine. tubing to connect the mask or nose piece to the machine. This Medicare coverage applies only if your doctor and supplier participate in the Medicare program.
What is Medicare Part B?
Medicare Part B is the section that pays for durable medical equipment (DME), such as CPAP machines. To have your CPAP machine covered, you need to make sure that your clinician and device supplier participate in the Medicare program.
How long does a CPAP machine last?
Your CPAP machine is paid for after 13 months and you’ll own it, but it should last several years . You may have it replaced with your medical benefit after this time.
Does Medicare cover CPAP machines?
Medicare will cover a part of the cost of a CPAP machine if you’ve been diagnosed with obstructive sleep apnea. Coverage for CPAP machines falls under the Medicare Part B coverage of durable medical equipment. You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs.
Do you pay for a CPAP machine?
You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs. A continuous positive airway pressure (CPAP) machine is a medical device that gives you extra oxygen with a bit of force.