What does the CPT code e0185 mean?
Oct 01, 2015 · For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements. ... Codes E0185 ...
Does Medicare cover echocardiograms?
Oct 01, 2015 · For the items addressed in this LCD, the “reasonable and necessary” criteria, based on Social Security Act § 1862 (a) (1) (A) provisions, are defined by the following coverage indications, limitations and/or medical necessity. A Group 1 mattress overlay or mattress ( E0181, E0182, E0184, E0185, E0186, E0187, E0188, E0189, E0196, E0197 ...
When does Medicare cover an EKG?
Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live. Your Medicare coverage choices. Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan ...
Does Medicare cover transesophageal echocardiogram (TEE)?
Sep 04, 2021 · Does Medicare cover mammograms after age 65? Medicare does cover mammograms for women aged 65-69. Annual screening mammograms have 100% coverage. Medicare pays 80% of the cost of diagnostic mammograms. Mammograms remain an important cancer detection tool as you age. Twenty-five percent of breast cancer diagnoses involve …

How often can you get a walker from Medicare?
Does Medicare cover low air loss mattress?
Does Medicare cover mattress for bed sores?
What type of mattress does Medicare cover?
Does Medicare help with mattress?
Does Medicare pay for gel mattress?
How often will Medicare replace a mattress?
Will Medicare pay for a Craftmatic bed?
Does Medicare cover mattress toppers?
Is memory foam mattress good for elderly?
What is a pressure relief mattress?
Why is it called a low air loss mattress?
What is a POD in Medicare?
Proof of delivery (POD) is a Supplier Standard and DMEPOS suppliers are required to maintain POD documentation in their files. Proof of delivery documentation must be made available to the Medicare contractor upon request. All services that do not have appropriate proof of delivery from the supplier shall be denied as not reasonable and necessary.
What is a support surface that does not meet the characteristics specified in the Coding Guidelines section of the Policy Article?
A support surface which does not meet the characteristics specified in the Coding Guidelines section of the Policy Article will be denied as not reasonable and necessary.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is Section 1833 E?
Section 1833 (e) of the Social Security Act precludes payment to any provider of services unless "there has been furnished such information as may be necessary in order to determine the amounts due such provider". It is expected that the beneficiary’s medical records will reflect the need for the care provided. The beneficiary’s medical records include the treating practitioner’s office records, hospital records, nursing home records, home health agency records, records from other healthcare professionals and test reports. This documentation must be available upon request.
Do DMEPOS require a WOPD?
For DMEPOS base items that require a WOPD, and also require separately billed associated options, accessories, and/or supplies, the supplier must have received a WOPD which lists the base item and which may list all the associated options, accessories, and/or supplies that are separately billed prior to the delivery of the items. In this scenario, if the supplier separately bills for associated options, accessories, and/or supplies without first receiving a completed and signed WOPD of the base item prior to delivery, the claim (s) shall be denied as not reasonable and necessary.
Do you need a written order for DMEPOS?
For Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) base items that require a Written Order Prior to Delivery (WOPD), the supplier must have received a signed SWO before the DMEPOS item is delivered to a beneficiary. If a supplier delivers a DMEPOS item without first receiving a WOPD, the claim shall be denied as not reasonable and necessary. Refer to the LCD-related Policy Article, located at the bottom of this policy under the Related Local Coverage Documents section.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
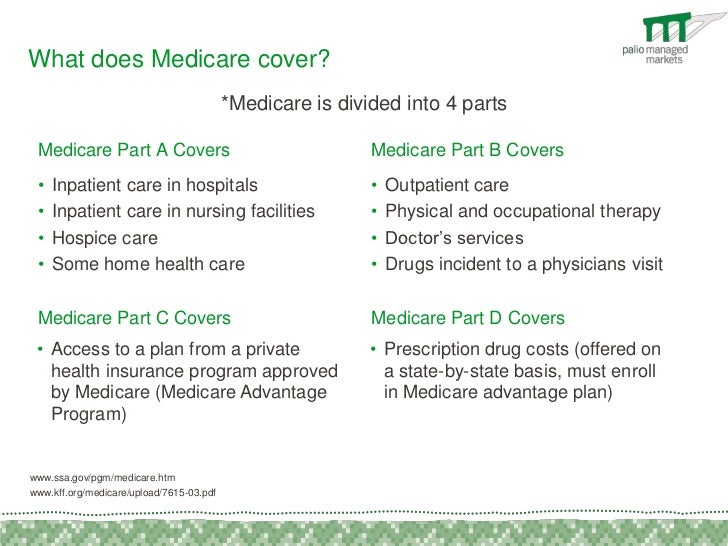
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
When does Medicare pay for mammograms?
Medicare pays for a routine screening mammogram every year, starting at age 40.
Does Medicare pay for breast ultrasound?
Part B covers breast ultrasound as a diagnostic procedure if it’s necessary. Medicare will pay 80% of the cost, and you’ll be responsible for the other 20%.
Is a 3D mammogram more expensive than a 2D mammogram?
Medicare covers 3D mammograms in the same way as 2D mammograms. But, a 3D image is more expensive than a standard 2D mammogram.
Does Medicare cover mammograms in the late 70s?
Part B continues to cover screening and diagnostic mammograms for women in their late 70s. Medicare pays the full cost of testing annually, and 80% of the cost of diagnostic mammograms. About 14% of breast cancer diagnoses occur in women aged 75-84. The American Cancer Society recommends women in their late 70s have breast cancer screenings.
What is Medicare's Welcome to Medicare?
The main purpose of the “Welcome to Medicare” visit is for your health care provider to create a personalized prevention plan for your health care needs. Yearly Wellness Visit. Your Medicare Part B coverage includes preventive services, including an annual wellness visit.
What is a wellness check up?
At your wellness check-up, your physician will check your height, weight, blood pressure, and any other necessary measurements, and evaluate you for cognitive impairment. Your physician will give you health advice based on your results, let you know what your risk factors are, and offer treatment options if you require them.
Does Medicare cover annual health visits?
Medicare offers an initial health exam when you are first enrolled in Medicare coverage and annual health care visits. If you are enrolled in Medicare Part B coverage, you will be eligible for an initial “Welcome to Medicare” visit. After that, your Medicare coverage includes yearly “wellness” visits. Here are the details about what to expect ...
Does Medicare Advantage have the same benefits as Original Medicare?
If you are enrolled in a Medicare Advantage plan, you will have at least the same Pat A and Part B benefits as Original Medicare, so you will have access to the Welcome to Medicare visit and yearly wellness visits.
How long does Medicare cover hospitalization?
Part A has a larger deductible, but once you’ve met it, Medicare covers all your hospitalization costs for the first 60 days you’re in the hospital.
How to find a Medigap plan?
MedicareFAQ can help you find the Medigap plan that’s right for you. Just call us or fill out our form and we’ll get started on a free quote.
How much does an EKG cost?
An EKG costs about $50, according to the American Academy of Family Physicians. The Medicare reimbursement rate may be less. Medicare will pay 80 percent of its current reimbursement rate for the procedure. You can expect to pay the other 20 percent if you don’t have Medigap.
Do you pay less for EKG with Medicare Advantage?
Advantage plans also have doctor networks. So, you’ll pay less if you use an in-network doctor. If you have Medicare Advantage, EKG coverage follows the same rules as in Medicare. But your costs may be different. To avoid unexpected bills, make sure the doctors administering your EKG are in your plan’s network.
Is an EKG the same as an echocardiogram?
Although the names are similar, an electrocardiogram (EKG) is not the same as an echocardiogram. An echocardiogram, or echo, uses sound waves to produce moving pictures of your heart. Also known as a heart ultrasound, it shows your heart’s size and shape and how well the heart and valves are working. Medicare covers echocardiograms ...
Does Medicare cover EKG?
Medicare covers echocardiograms if they’re medically necessary. Your doctor may order an electrocardi ogram, or EKG, to measure your heart’s health. Medicare will also pay for one routine screening EKG during your first year on Medicare.
Does Medicare cover nuclear stress tests?
Nuclear stress tests and echocardiographic stress tests include imaging as part of the procedure. No matter what type of stress test you have, Medicare will cover the test if it’s necessary. Coverage falls under Part A if you’re an in-patient, and Part B if you’re not.
