The brace must be durable, used for a medical reason, not useful for someone who is not sick or injured, used in your home, and must have an expected lifetime of at least three years. If you have Original Medicare, you will pay 20% of the Medicare approved amount of the brace as long as the supplier is enrolled in Medicare and accepts assignment.
Full Answer
Will Medicare pay for a brace?
If you have Original Medicare, you will pay 20% of the Medicare approved amount of the brace as long as the supplier is enrolled in Medicare and accepts assignment. The Part B deductible still applies.
How does Medicare pay for supplies?
Medicare covers the amount of supplies your doctor says you need, based on your condition. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
How does Medicare pay for DME?
The amount you must pay for health care or prescriptions before Original Medicare, your Medicare Advantage Plan, your Medicare drug plan, or your other insurance begins to pay. applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment.
Does Medicare cover durable medical equipment?
A prescription from your doctor is generally adequate for coverage. However, in some situations, Medicare may require prior authorization before paying for Durable Medical Equipment. Every injection comes with a specific cost.
How often does Medicare pay for a rollator walker?
Medicare will pay for you to have a new walker with seat every five years.
Does Medicare pay for hernia belts?
A hernia support (whether in the form of a corset or truss) which meets the definition of a brace is covered under Part B under §1861(s)(9) of the Act.
Are arm slings covered by Medicare?
Number 4 — Not all equipment is covered by Medicare. For example, no matter what the diagnosis is, an arm sling is never covered, and neither is a post-op or surgical shoe. These are non-covered items.
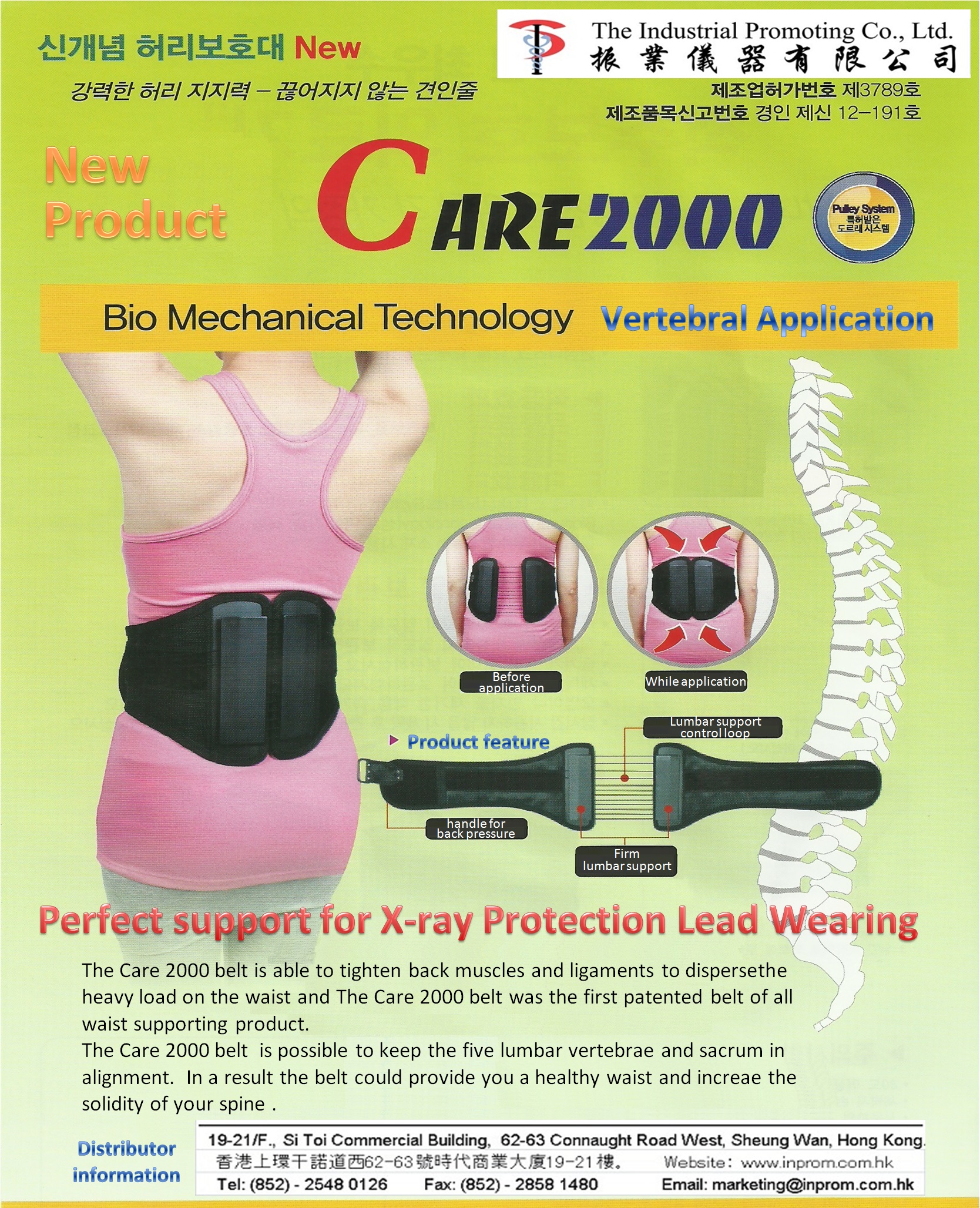
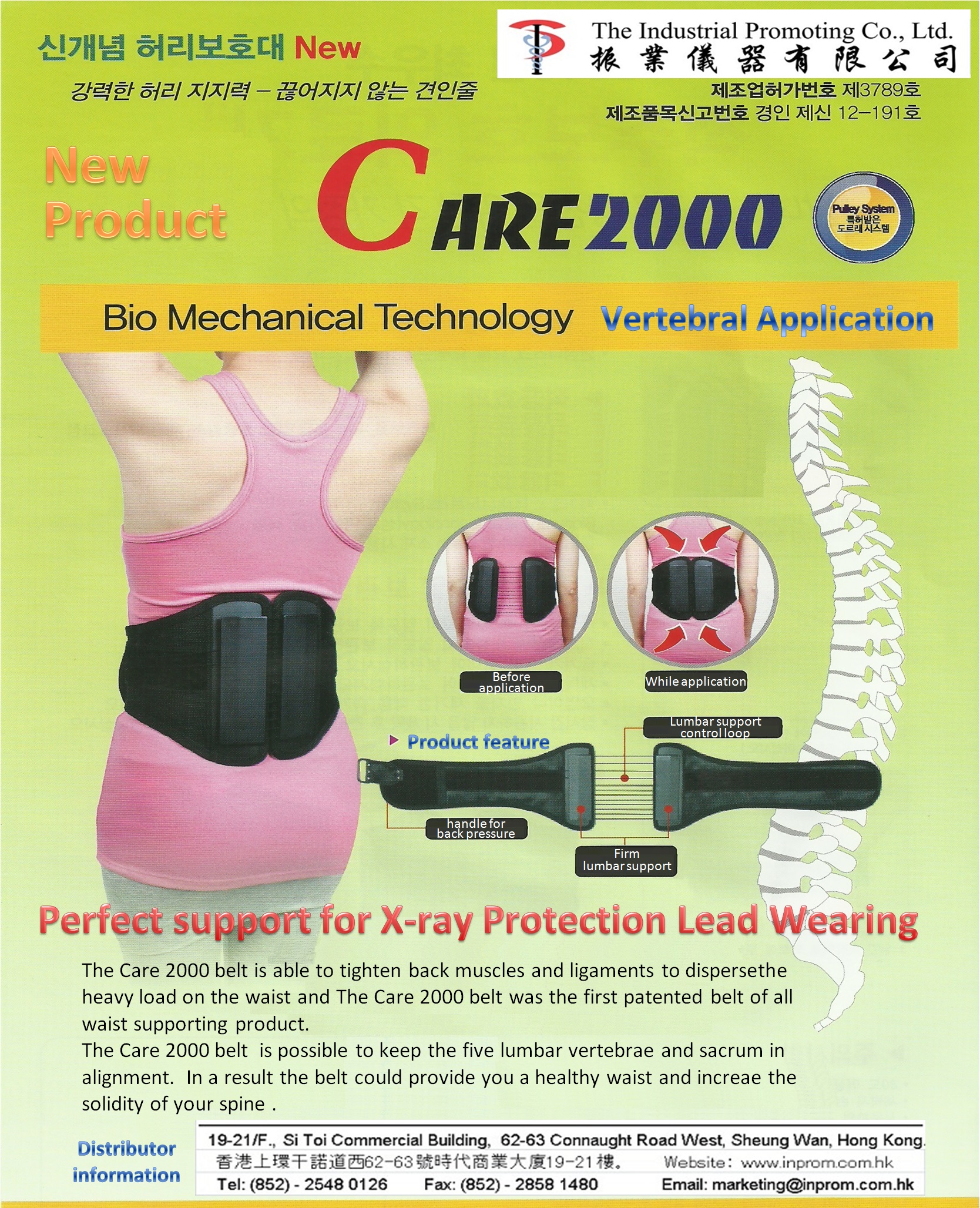
Is a back brace considered durable medical equipment?
Back braces are categorized as durable medical equipment, or DME. Durable medical equipment consists of products and items used for medical purposes, such as crutches, wheelchairs, braces and more. Items classified as DME are covered by Medicare Part B.
What is hernia belt?
A hernia truss or belt is a supportive undergarment for men designed to keep the protruding tissue in place and relieve discomfort. If you have an inguinal hernia, a hernia truss can help you feel more comfortable temporarily, but it doesn't treat the hernia. Talk to your doctor if you want to use a truss.
Does Medicare cover AFO?
Medicare will also cover AFO and KAFO prescriptions, although additional documentation and notes are necessary to receive full benefits. Documentation from the ordering physician, such as chart notes and medical records, is required for coverage.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Does Medicare pay for exercise equipment?
The short answer is, Yes, Medicare does pay for Durable Medical Equipment (DME)!
Is a sling considered durable medical equipment?
*Note: Certain non-durable items (e.g., arm slings, Ace bandages, splints, foam cervical collars, etc.) may be eligible for payment in some circumstances even though they are not durable and do not fit within the definition of DME.
Is a walker covered by Medicare?
Summary: Medicare generally covers walkers as part of “durable medical equipment.” To get full coverage, you may need a Medicare Supplement plan. A walker may be essential for you if you struggle to walk without support.
Is a walking boot considered durable medical equipment?
We offer a wide selection of durable medical equipment for orthopedic conditions, including: Crutches and walkers. Custom-fitted and prefabricated splints and walking boots. Air-pump walking boots.
Does Medicare pay for Dr Ho back brace?
Ho's Decompression Back Belt is now approved by Medicare, and will be launching in the United States in April 2012. This means that back pain sufferers with Medicare plans can now use their plans to receive their own Dr. Ho's belt.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Do Medicare contract suppliers have to accept assignment?
Contract suppliers are required to provide the item to you and accept assignment as a term of their contract with Medicare. Visit Medicare’s supplier directory to see if you live in or are visiting a competitive bidding area, or to find suppliers who accept assignment. Return to search results.
What is Medicare approved braces?
Medicare Approved Braces and Devices. Medicare approves braces and devices when medically necessary to treat or maintain a medical condition. Orthotic devices like braces are otherwise known as Durable Medical Equipment. Braces may be used to support the knee, neck, arm, or back. Combining the use of orthotic devices with other treatments may delay ...
What is wrist support brace?
Wrist support braces are another type of Durable Medical Equipment. Benefits include all wrist supports, braces, and stabilizers. Wrist supports may provide some pain relief due to medical conditions such as tendonitis, carpal tunnel syndrome, and other wrist strains or sprains.
What is durable knee brace?
The term durable means the device can handle repeat-usage over some time (3+ years). Medicare requires knee braces to provide therapeutic at-home benefits. As with other devices, your doctor must document an appropriate diagnosis that shows the need for the equipment.
What is durable medical equipment?
The Durable Medical Equipment must be a functional and rehabilitative device for coverage to apply . Knee orthotics must also aid a patient’s healing process of joint or neighboring tissue after an injury or surgery. Functional – A pre-injured knee may be the result of a fall, sporting injury, or trauma to the area.
Does Medicare pay for cervical collars?
Currently, Medicare doesn’t pay for these devices. Cervical collars may be either soft or hard. Soft collars are more comfortable; typically, these braces are made of foam, felt, or rubber. Hard neck supports may keep the head and neck completely still. After invasive surgery or severe neck injury, your doctor may prescribe hard neck support.
Does Medicare require a prescription for a medical device?
However, in some situations, Medicare may require prior authorization before paying for Durable Medical Equipment. Every injection comes with a specific cost. Talk to your plan directly to determine the allowable amount for a procedure or injection.
Does Medicare cover ankle braces?
Yes, Medicare will help cover the costs of ankle braces. Beneficiaries pay only 20% of the cost for ankle braces with Part B. Benefits may include ankle braces, straps, guards, stays, stabilizers, and even heel cushions. Acute and chronic ankle or foot pain is a common, everyday use for these devices.
What does Medicare Part B cover?
Supplies. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually doesn’t cover common medical supplies, like bandages and gauze, which you use at home.
What is Medicare Advantage Part C?
Some Medicare Advantage Plans (Part C) offer extra benefits that Original Medicare doesn’t cover - like vision, hearing, or dental. Contact the plan for more information. Return to search results.
What is an ostomy in Medicare?
The National Institutes of Health reports that an ostomy is a surgical procedure. This procedure creates an opening which is known as a stoma.
Do you have to pay Part B deductible for ostomy?
Beneficiaries must first pay the Part B deductible unless they have supplemental coverage. The need for ostomy supplies must be due to specific procedures. Including, ileostomy, urinary ostomy surgery, or a colostomy. Beneficiaries must use both providers and suppliers that accept and participate in a Medicare assignment to receive coverage.
Does Medicare cover ostomy supplies?
Medicare will cover up to a three- month supply of ostomy products at one time. You must have a prescription from your doctor to receive coverage under Medicare. The supplier must also be accredited and contracted with Medicare. Ostomy Supplies Covered by Medicare. Amount Allowed Per Month.
Does Medicare cover everything?
Medicare does not cover everything. Under Part A, you’re left with deductibles and other cost-sharing. Under Part B, you’re responsible for the remaining 20% of all your medical costs as well as deductibles. There are a few ways you can get supplemental coverage. One option is through a Medicare Advantage plan.
Is Medicare Supplement better than Medicare Supplement?
If your goal with supplemental insurance is to have less out-of-pocket costs, then a Medicare Supplement is the better option for you. Medicare Supplements will cover the coinsurance and deductibles left behind by Medicare. Some letter plans will leave you with zero out of pocket costs outside the monthly premium.
How much does Medicare pay for braces?
If you have Original Medicare, you will pay 20% of the Medicare approved amount of the brace as long as the supplier is enrolled in Medicare and accepts assignment. The Part B deductible still applies. If the supplier is enrolled in Medicare but is not “participating,” they can choose not to accept assignment.
What is a DME brace?
Medicare Part B (Medical Insurance) covers medically necessary back braces under the durable medical equipment (DME) prefabricated orthotics benefit. Your Medicare-approved physician must prescribe the back brace and it must meet specific DME criteria. The brace must be durable, used for a medical reason, not useful for someone who is not sick ...
Does Medicare Advantage have Part B?
If you are enrolled in a Medicare Advantage plan, such as an HMO or PPO, you will have at least the same Part B coverage as Original Medicare, but many MA plans offer additional coverage. Your costs will depend on which plan you choose.
Does Medicare cover back braces?
With guidance from your physician regarding time worn and specific exercises, wearing a back brace can have many positive benefits, including: High quality braces can be costly, but Medicare may help cover the cost of a back brace.
What is lumbar medial branch block?
Lumbar medial branch blocks refer to a diagnostic procedure where injection of an anesthetic “tests” the joint’s nerve endings. This is done to verify the pain relief response and receives coverage when medically necessary. When the patient feels relief, they’re a candidate for radiofrequency ablation.
What is supplemental insurance?
Supplement coverage is crucial for those with lower back pain management needs. When undergoing pain management treatments, supplemental insurance protects you financially. There are many different types of injections for treatment available to those with either chronic or acute conditions. We’ll acquaint you with some of ...
Does Medicare cover cortisone injections?
Per the standard Medicare guidelines, cortisone injections usually receive coverage without prior authorization. Also, different doses have different costs. Make sure to ask your doctor about the allowable amount for each procedure. Supplement coverage is crucial for those with lower back pain management needs.
Does Medicare cover pain management?
Usually, Medicare covers pain management injections when they’re determined to be medically necessary. Suppose you’re receiving an injection during an inpatient stay at a hospital. In that case, it will receive coverage from Part A. If your doctor administers the procedure in an outpatient setting, Part B covers the injection.
Does Medicare cover discectomy?
Sometimes, surgery, known as a discectomy, is performed to fix a herniated disc. But, Medicare doesn’t cover discectomies because patients can often get relief for a herniated disc through non-surgical approaches. These avenues for relief include exercise, physical therapy, massage, and pain medication.
Does Medicare cover lower back pain?
Medicare coverage for lower back pain management is available when necessary. Yet, some costs you may pay for entirely. By the time most people reach eligibility, they’ve had some lumbar pain. Those feeling lower back pain need to know about treatments and pain management therapies. The cause of the back pain determines a patient’s eligibility ...
Does Medicare cover lumbar spondylolisthesis?
Lumbar Spondylolisthesis. Medicare doesn’t cover lumbar artificial disc replacement (LADR) surgery. Alternative treatments are pain management medications and physical therapy. The latter have coverage when a doctor refers you to help get back on your feet.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES: For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
ICD-10-CM Codes that Support Medical Necessity
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the LCD section on “ Coverage Indications, Limitations, and/or Medical Necessity ” for other coverage criteria and payment information.
ICD-10-CM Codes that DO NOT Support Medical Necessity
For the specific HCPCS codes indicated above, all ICD-10 codes that are not specified in the preceding section. For all other HCPCS codes, diagnoses are not specified.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.