You’ll get a bill: Part B only. Every 3 months. Part A (Hospital Insurance) Every month. Part D income-related monthly adjustment amount (Part D IRMAA) Part D IRMAA. An extra amount you pay in addition to your Part D plan premium, if your income is above a certain amount. Every month.
Full Answer
When can I enroll in Medicare Part B?
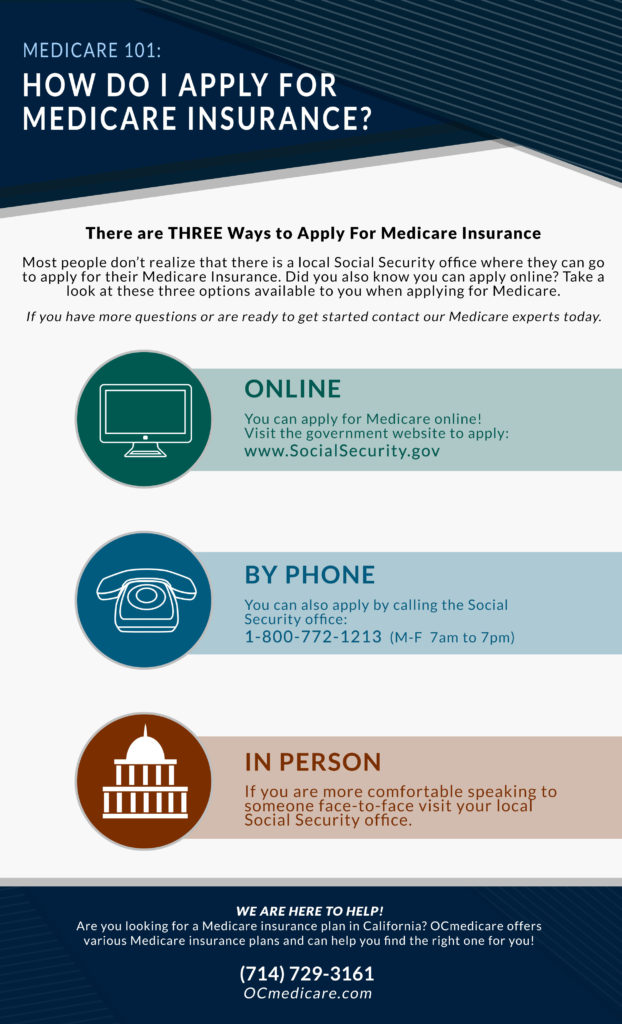
· Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). Send the completed form to your local Social Security office by fax or mail. Call 1-800-772-1213. TTY users can call 1-800-325-0778. Contact your local Social Security office. If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
How can I get help with Medicare Part A and Part B?
· During Medicare's General Enrollment Period (January 1–March 31), you can enroll in Part B and your coverage will start July 1. Deciding to enroll in Part B is an important decision. It depends on the type of coverage you have now. It’s also important to think about the Part B late enrollment penalty—this lifetime penalty gets added to your monthly Part B premium, and it …
How much does Medicare pay for Medicare Part B?
· Views: 80286. States must help pay some of the Medicare costs for beneficiaries who have limited income and resources. Under these programs, states help pay for Medicare Part A and Part B premiums, deductibles and copayments. Some of these programs also pay additional Medicare expenses for elderly and disabled people.
How much does Medicare Part B cost in 2020?
· You are first eligible to apply for Medicare three months before you turn 65. This marks the beginning of the Initial Enrollment Period, which lasts for seven months. You are required to apply for Medicare during this period to avoid getting extra fees charged to you. The only way to avoid getting an extra fee is to apply for an extension.
Do you have to enroll in Medicare Part B every year?
For Original Medicare (Parts A and B), there are no renewal requirements once enrolled. Medigap plans ― also known as Medicare Supplement plans ― auto renew annually unless you make a change.
How often are Medicare Part B premiums adjusted?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security.
Do you have to renew Medicare supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.
Is Medicare Part B billed monthly or quarterly?
Medicare will issue Part A bills monthly and Part B bills every 3 months. There are several ways to pay the premiums, including: through the Medicare account. online through a bank's bill payment service.
What is the Medicare Part B premium for 2021?
$148.50Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Is Medicare Part B premium automatically deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
Does my Medicare supplemental plan automatically renew?
Once you find the best plan, you will likely want to be able to keep it. Fortunately, you will be able to stay with your plan as long as you like in most cases. This is called “guarantee renewable.” Medicare Supplement insurance plans renew automatically when you make your premium payment.
Do Medicare supplement plan benefits automatically update?
As long as you pay your premium, your Medigap policy is guaranteed renewable. This means it is automatically renewed each year. Your coverage will continue year after year as long as you pay your premium.
Can I change my Medicare supplement anytime?
FAQs. When can I change my Medicare Supplement plan? You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
Are Medicare Part B premiums deducted a month in advance?
These bills are paid in advance of coverage. For example, if you applied for Medicare to start in August, you'll receive a bill in July for your August, September, and October Part B premiums.
Will Medicare send me a bill for Part B?
If you have Medicare Part B but you are not receiving Social Security or Railroad Retirement Board benefits yet, you will get a bill called a “Notice of Medicare Premium Payment Due” (CMS-500). You will need to make arrangements to pay this bill every month.
Does Medicare Part B pay for prescriptions?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a limited number of outpatient prescription drugs under certain conditions.
When do you get Medicare Part B?
Most people get Medicare Part B (Medical Insurance) when they turn 65. If you didn't sign up for Part B then, now's the time to decide if you want to enroll. During Medicare's General Enrollment Period (January 1–March 31), you can enroll in Part B and your coverage will start July 1.
How to apply for Part B?
Signing up for Part B is easy—apply by March 31. Fill out a short form, and send it to your local Social Security office. Call Social Security at 1-800-772-1213. TTY users can call 1-800-325-0778. Contact your local Social Security office. If you get benefits from the Railroad Retirement Board, contact your local RRB office to sign up for Part B. ...
Is it important to enroll in Part B?
Deciding to enroll in Part B is an important decision. It depends on the type of coverage you have now. It’s also important to think about the Part B late enrollment penalty—this lifetime penalty gets added to your monthly Part B premium, and it goes up the longer you wait to sign up.
What age does Medicare cover outpatient?
Medicare coverage becomes available to individuals once they reach the age of 65 or under the age of 65 when they qualify due ...
How long does Medicare coverage last?
This marks the beginning of the Initial Enrollment Period, which lasts for seven months.
How long does a Part B extension last?
This period begins the month that you retire or that your healthcare benefits end and lasts for a total of eight months.
How much is the 2020 Medicare premium?
The base premium payment for 2020 is $144.60 for everyone with an annual income of less than $87,000 or joint filers with an income less than $174,000. If you are above this income threshold, your premium payment may increase to up to $376 per month if you file as an individual and up to $491.60 if you file jointly.
How many employees do you need to have to sign up for Medicare?
If you are receiving healthcare insurance from an employer, it is also important to consider how large the company is. If the employer has fewer than 20 employees, they have the option of requiring you to sign up for Medicare Part B during your Initial Enrollment Period, causing Medicare to serve as your primary insurance ...
Does Medicare coinsurance apply to a physician?
This coinsurance cost only applies at providers that accept Medicare assignment and partner with them to provide care. If you visit a physician or facility that does not accept assignment, you will be forced to pay the entire amount out of pocket as opposed to just 20 percent.
What is Medicare Part B?
Some people automatically get. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , and some people need to sign up for Part B. Learn how and when you can sign up for Part B. If you don't sign up for Part B when you're first eligible, ...
What is the standard Part B premium for 2021?
The standard Part B premium amount in 2021 is $148.50. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
What happens if you don't sign up for Part B?
If you don't sign up for Part B when you're first eligible, you may have to pay a late enrollment penalty.
How much do you pay for Medicare after you meet your deductible?
After you meet your deductible for the year, you typically pay 20% of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How much is Part B deductible in 2021?
Part B deductible & coinsurance. In 2021, you pay $203 for your Part B. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. . After you meet your deductible for the year, you typically pay 20% of the.
Do you pay Medicare premiums if your income is above a certain amount?
If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
How many forms do you need to submit to get SEP?
Beneficiaries must submit two forms to get approval for the SEP.
How to use SEP form?
To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS 40B) and the request for employment information form (CMS L564). You’ll complete the Medicare enrollment application and give the request for employment information form to the employer to fill out. You want to request additional copies of form L564 from Social Security if you’ve been covered through more than one job-based plan since you qualified for Medicare.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
Can disabled people get SEP?
People 65 and older only qualify for this SEP if they have coverage through their own or their spouse’s job, but disabled individuals can also qualify because they’re covered by a non-spouse family member’s plan.
When will Part B coverage start?
You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B. (Even though you weren't covered a total of 27 months, this included only 2 full 12-month periods.)
When does Part B start?
You waited to sign up for Part B until March 2019 during the General Enrollment Period. Your coverage starts July 1, 2019. Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B.
What percentage of FPL can I get for Medicare Part B?
Not have an income that is more than 200% of the FPL (You may only get partial aid if your income is between 150% to 200% of the FPL.) Part B Only: Both the Specified Low-Income Medicare Beneficiary (SLMB) and Qualifying Individual (QI) programs will help pay for Medicare Part B premiums.
What is the difference between Medicare Part A and Part B?
All programs require eligibility for Medicare Part A, but the main difference between each is the federal poverty level (FPL) range that those seeking help must be within.
How much is Part B insurance?
The standard Part B premium as of 2019 is $135.50, but most people with Social Security benefits will pay less ($130 on ).
Is QMB coverage 100%?
But if you’re approved as a QMB, you are not responsible for paying any cost-sharing, according to the Center for Medicare Advocacy. This means that your Medicare costs, including your premiums, are 100% covered. To qualify for the QMB program, your income must not exceed 100% of the FPL.
Does Medicare Part B pay for premiums?
Part B Only: Both the Specified Low-Income Medicare Beneficiary (SLMB) and Qualifying Individual (QI) programs will help pay for Medica re Part B premiums. 4
Can you get Medicare out of pocket?
Each state manages MSP funds and decides who qualifies. Programs can pay for all, or just some, of your Medicare out-of-pocket expenses, which includes premiums.
How much is Medicare Part D 2022?
Medicare Part D plans are also provided through private insurance companies. The national average Part D premium is $33 for 2022. 3 But depending on where you live and the type of plan you have, Medicare Part D costs will vary.
When does Medicare take effect?
January–March. April–June. July–September. If you make a change, it will take effect on the first day of the following month. You’ll have to wait for the next period to make another change. You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October ...
How often can you change your medicaid?
If you have Medicaid or receive Extra Help, you may be able to make changes to your coverage one time during each of these periods: If you make a change, it will begin the first day of the following month. You’ll have to wait for the next period to make another change.