What do the Medicare star ratings mean?
“CMS’s annual ratings deliver meaningful information about the quality of each plan to help people with Medicare make informed health care decisions.” People with Medicare can compare quality through the Star Ratings, along with other information such as cost and coverage, on the online Medicare Plan Finder tool available on Medicare.gov.
What is a five-star Medicare Plan Rating?
Star ratings range from one to five, with one being the lowest rating and five being the highest. You may be able to switch to a top-rated plan once a year during the five-star enrollment period. The Centers for Medicare & Medicaid Services (CMS) updates ratings for Medicare plans every fall.
What percentage of Medicare Advantage plans have 4 or more stars?
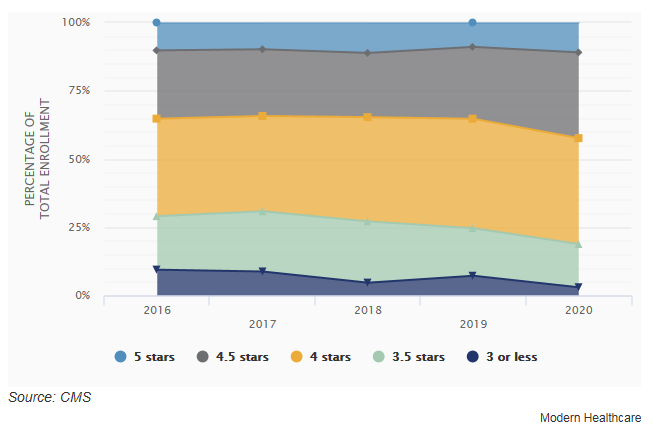
Approximately 90 percent of people currently in Medicare Advantage plans that offer prescription drug coverage are enrolled in a plan that earned four or more stars in 2022. The number of plans with a rating of 4 or more stars is higher for 2022 compared to last year.
Are StarStar ratings enough to compare nursing homes?
Star ratings can give you important information and help you compare nursing homes, but aren't a substitute for visiting the nursing home.

How do Medicare star ratings work?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
How do I increase my star rating for Medicare Advantage?
To improve the star ratings program, its measures must include fewer administrative measures, risk-adjusted mortality rates, and more equitable risk-adjustment formulas.
Are star ratings predictable?
It Is Possible To Accurately Predict Star Ratings.
Does Medicare need to be updated every year?
In general, once you're enrolled in Medicare, you don't need to take action to renew your coverage every year. This is true whether you are in Original Medicare, a Medicare Advantage plan, or a Medicare prescription drug plan.
How star ratings are calculated?
Summary star ratings are an average of a provider's question level star ratings. Patient star ratings are calculated by dividing the patient's aggregate mean score by 20. For clients using only one question in the patient star rating, the star rating would simply be the individual question score, divided by 20.
What is CMS star rating based on?
The Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health plan and health care system — the Star Rating Program. Health plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
How often are star ratings calculated?
each yearStar Ratings are calculated each year and may change from one year to the next.
Who sets the standards for Medicare star ratings?
The Centers for Medicare & Medicaid Services (CMS) publishes the Medicare Part C and D Star Ratings each year to measure the quality of health and drug services received by beneficiaries enrolled in Medicare Advantage (MA) and Prescription Drug Plans (PDPs or Part D plans).
Why are star ratings important to Medicare Advantage plans?
Medicare star ratings are important because they give you an idea about which plans in your area have the highest satisfaction ratings. Star ratings only pertain to Medicare Advantage and Part D plans. For both types of coverage, the ratings provide a way to compare your plan options beyond their cost.
What is Medicare annual enrollment period?
When you first become eligible for Medicare, you can join a plan. Open Enrollment Period. From October 15 – December 7 each year, you can join, switch, or drop a plan. Your coverage will begin on January 1 (as long as the plan gets your request by December 7).
Does Medicare automatically renew?
If you have Medicare Part A (hospital insurance) and/or Part B (medical insurance) and you are up to date on your Medicare premiums, your Medicare coverage will automatically carry over from one year to the next and there is nothing you need to do to renew your plan.
How often do you have to enroll in Medicare?
This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65....When your coverage starts.If you sign up:Coverage starts:The month you turn 65The next month1 month after you turn 652 months after you sign up2 more rows
When will Medicare star ratings come out?
Every year, during the fall season, CMS announces the Medicare Star Rating for the upcoming year. It means that in October 2021, the Star Ratings for 2022 will come out. These ratings are updated every year, so they may vary from each year.
How many times can you use SEP?
You are allowed to only use this SEP service once within the given time limit.
Is Medicare the same as all plans?
Many people often mistake that all Medicare plans are the same. But it is not the case. To find the top best-performing coverage option, you need to check their Medicare star rating.
Have any Medicare questions?
Do you have any Medicare-related questions? We are here to guide you through every matter so you can have a healthier life. Feel free to contact us.
How does Medicare's star rating system work?
You could choose from a wide range of Medicare Part C (now known as Medicare Advantage) plans as early as 1997. But you didn't have a good way to compare them until 2008. That's when the Centers for Medicare & Medicaid Services (CMS) first rolled out the star rating system.
What parts of a health insurance plan are rated?
The way that the CMS rates healthcare plans depends on what type of plan it is.
What is the standard rating for a Medicare plan?
Most Medicare plans have a good rating these days, but not all. According to the CMS, nearly 68% of Medicare plans with prescription drug coverage (MA-PDP) in 2022 have a four-star rating or higher. That’s up from 49% in 2021.
How to use the rating system to pick the best health insurance plan
In general, it's best to choose the highest-rated plan that you can afford. You can compare plans and their ratings on the Medicare Plan Finder website. On the Plan Finder tool, each plan has an overall star rating based on all the rated categories.
The bottom line
Choosing between different Medicare plans can be tough. But the star ratings can help you identify high-performing ones and those with higher scores in categories that may matter to you. The CMS rates each plan on up to 40 different factors to create a helpful picture of how well the plan treats its members and their healthcare needs.
Top 5-star Medicare Advantage plans
Medicare Advantage plans with five stars are top-tier plans that are considered "excellent" by the Medicare's administering agency, the Centers for Medicare & Medicaid Services (CMS).
5-star special enrollment period
If a 5-star plan is available in your location, you qualify for a 5-star special enrollment period (SEP) that allows you to switch to a 5-star plan at any time during the year.
How Medicare star ratings are calculated
Each Medicare plan's overall star rating is a weighted average of several different data points. This means it's a robust measurement that can help you understand which are the best-performing Medicare plans in your area.
Frequently asked questions
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calculations about the number of complaints, outcomes such as how often those with diabetes fill their prescriptions and more.
Methodology
Data and analysis is based on Centers for Medicare & Medicaid Services (CMS) public use files, fact sheets and technical notes. Medicare Advantage analysis only includes plans that include prescription drug coverage and excludes employer-sponsored plans, special needs plans, PACE plans, sanctioned plans and health care prepayment plans (HCPPs).
How many areas are in the Medicare Star Ratings?
The Medicare Star Ratings provide an in-depth analysis. The Overall Star Ratings above appear to be made up of five areas. In reality, each of those five areas is broken down even further.
What is the purpose of Medicare star rating?
The purpose of the Medicare Star Ratings is to help consumers make educated decisions when purchasing their health insurance plans. The Centers for Medicare & Medicaid Services (CMS) assigns a star rating of 1 to 5 based on ratings across designated performance areas. More stars mean better performance.
How are Star Ratings calculated?
Each Star Rating calculation is separate for the type of plan and coverage. For example, Star Ratings for health plans are different than those for hospitals.
Why is CMS rating important?
The CMS Star Ratings can be an invaluable tool when searching for insurance plans and providers. They shouldn’t, however, be your only resource when making decisions. When researching your choices, make sure you’re searching for the services and facilities you need, or may need in the future–seeing a provider’s rating in these specific areas may be more important to you than just the plan’s overall Star Rating.
When are CMS star ratings released?
CMS updates its Star Ratings at different times. Ratings for insurance plans are typically released each fall to line up with enrollment periods for Medicare, Medicare Advantage, Medicare Prescription Drug Plan (Part D), and standard health insurance. Changes are made based on feedback, provider recommendations and the data itself.
What is the age limit for CMS ratings?
CMS provides ratings in several vital areas for customers who are 65 and older, including:
Why do providers publish their star ratings?
By having their rating published publicly, providers must decide to improve low-performing areas or risk losing future customers. The Marketplace displays star ratings alongside vital details like each plans’ premiums and deductibles.