Full Answer
Does Medicare cover every test?
Medicare coverage for many tests, items and services depends on where you live. This list only includes tests, items and services that are covered no matter where you live. If your test, item or service isn’t listed, talk to your doctor or other health care provider.
How often are serum CEA determinations indicated for metastatic solid tumors?
Serum CEA determinations are generally not indicated more frequently than once per chemotherapy treatment cycle for patients with metastatic solid tumors which express CEA or every two months post-surgical treatment for patients who have had colorectal carcinoma.
How often should CEA testing be performed in colorectal carcinoma patients?
In following patients who have had treatment for colorectal carcinoma, ASCO guideline suggests that if resection of liver metastasis would be indicated, it is recommended that post-operative CEA testing be performed every two to three months in patients with initial stage II or stage III disease for at least two years after diagnosis.
Does Medicare cover stress tests and electrocardiograms?
Nuclear stress tests and echocardiographic stress tests include imaging as part of the procedure. No matter what type of stress test you have, Medicare will cover the test if it’s necessary. Coverage falls under Part A if you’re an in-patient, and Part B if you’re not. Medicare Guidelines for a Diagnostic Electrocardiogram
Is CEA blood test covered by Medicare?
To summarize, NCD 190.26 provides, under the heading “Indications,” that a CEA test “may be medically necessary,” and thus covered by Medicare, for two broad groups of patients: (1) patients with colorectal cancer; and (2) patients with other types of cancer when the cancer tumor does not express a “more specific ...
What ICD 10 code will cover CEA?
0 for Elevated carcinoembryonic antigen [CEA] is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
Does Medicare cover a CA 125 blood test?
Medicare currently covers the use CA-125 for monitoring of response to therapy related to ovarian cancer. Based on this strong association between these two conditions, we believe that CA-125 testing is reasonable and necessary for monitoring response to therapy for PPC.
How long does a CEA take?
A CEA blood test usually takes less than five minutes. CEA tests of other body fluids usually take 30 minutes or less. You can return home the same day.
What diagnosis will cover CEA?
CEA is a protein polysaccharide found in some carcinomas. It is effective as a biochemical marker for monitoring the response of certain malignancies to therapy. CEA may be medically necessary for follow-up of patients with colorectal carcinoma.
What is the CPT code for CEA?
002139: Carcinoembryonic Antigen (CEA) | Labcorp. For hours, walk-ins and appointments.
What pathology tests are not covered by Medicare?
Medicare does not cover the costs of some tests done for cosmetic surgery, insurance testing, and several genetic tests. There are also limits on the number of times you can receive a Medicare rebate for some tests. Your private health insurance may pay for diagnostic tests done while you are a patient in hospital.
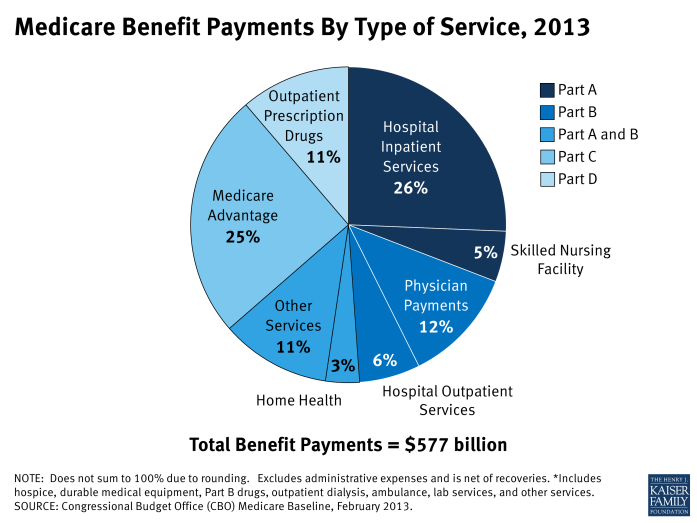
What tests are covered by Medicare?
Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines. Examples would be screening blood tests to diagnose or manage a condition. Medicare Advantage, or Part C, plans also cover blood tests.
Does Medicare Part B cover lab tests?
Medicare Part B covers clinical diagnostic lab tests such as blood tests, tissue specimen tests, screening tests and urinalysis when your doctor says they're medically necessary to diagnose or treat a health condition.
How often should CEA test be done?
The National Comprehensive Cancer Network, for example, recommends that people who are treated for stage II or III colon or rectal cancer have CEA testing every 3 to 6 months for 2 years and then every 6 months for 3 additional years, plus CT scans every 6 to 12 months for 5 years.
What is the cost of CEA test?
The CEA Blood Test cost is quite variable and differ from one city to another. Nevertheless, the average CEA Blood Test cost hovers in the 500 to 1500 INR range.
Does CEA detect all cancers?
High CEA levels may also be a sign of some noncancerous conditions, such as cirrhosis, noncancerous breast disease, and emphysema. A CEA test can't tell you what kind of cancer you have, or even whether you have cancer. So the test is not used for cancer screening or diagnosis.
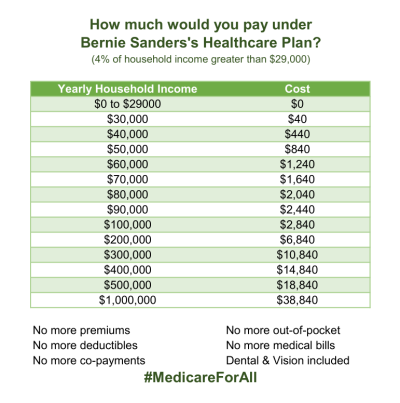
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
How long do you have to rent a medical machine?
to rent the machine for the 13 months if you’ve been using it without interruption. After you’ve rented the machine for 13 months , you own it.
Does Medicare cover CPAP machine rental?
If you had a CPAP machine before you got Medicare, Medicare may cover CPAP machine cost for replacement CPAP machine rental and/or CPAP accessories if you meet certain requirements.
What Parts of Medicare Cover Cortisone Injections?
Original Medicare (Medicare Parts A and B) and Medicare Advantage plans (Medicare Part C) provide limited coverage for cortisone injections.
How Much Does a Cortisone Shot Usually Cost?
The Medicare cost of a single cortisone shot can range from $25 to $300 or even more. Several factors influence the price of the injection, including:
How Often Will Medicare Pay for Cortisone Injections?
Although cortisone injections are incredibly beneficial, and the effects may last for several months, repeated injections can lead to further loss of cartilage. Doctors typically recommend a maximum of three injections annually.
Does Medicare Cover PRP Knee Injections?
Platelet-rich plasma (PRP) injections are another treatment option for post-surgery pain and chronic conditions like osteoporosis.
Does Private Insurance Cover Cortisone Injections?
Private insurance companies may offer more generous coverage for cortisone shots than Medicare with many policies covering medically necessary injections in hospitals and clinics. Insured patients may have out-of-pocket expenses as low as $10.
Medicare May Help With Pain-Relieving Injections
If a doctor suggests that cortisone injections could improve your wellbeing by relieving pain and inflammation, Medicare may cover some of the cost.
How much does an EKG cost?
An EKG costs about $50, according to the American Academy of Family Physicians. The Medicare reimbursement rate may be less. Medicare will pay 80 percent of its current reimbursement rate for the procedure. You can expect to pay the other 20 percent if you don’t have Medigap.
Does Medicare cover echocardiograms?
Medicare covers echocardiograms if they’re necessary. Coverage works the same way as for electrocardiograms: if you’re an outpatient, Part B covers the procedure. If you’re an inpatient, your Part A coverage applies.
Does Medicare cover EKG?
Medicare covers echocardiograms if they’re medically necessary. Your doctor may order an electrocardi ogram, or EKG, to measure your heart’s health. Medicare will also pay for one routine screening EKG during your first year on Medicare.
Does Medicare cover nuclear stress tests?
Nuclear stress tests and echocardiographic stress tests include imaging as part of the procedure. No matter what type of stress test you have, Medicare will cover the test if it’s necessary. Coverage falls under Part A if you’re an in-patient, and Part B if you’re not.
Do you pay less for EKG with Medicare Advantage?
Advantage plans also have doctor networks. So, you’ll pay less if you use an in-network doctor. If you have Medicare Advantage, EKG coverage follows the same rules as in Medicare. But your costs may be different. To avoid unexpected bills, make sure the doctors administering your EKG are in your plan’s network.
What percentage of Medicare payment does a supplier pay for assignment?
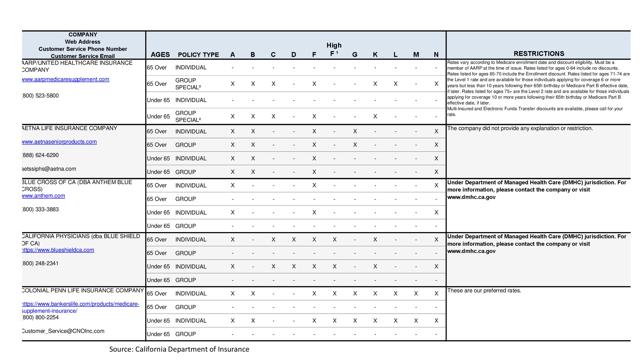
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What happens if you don't enroll in Medicare?
If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them. Make sure your doctors and DME suppliers are enrolled in Medicare. It’s important to ask your suppliers if they participate in Medicare before you get DME.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
Does Medicare cover wheelchairs?
Medicare Part B (Medical Insurance) covers power-operated vehicles (scooters) and manual wheelchairs as durable medical equipment (DME) that your doctor prescribes for use in your home. You must have a face-to-face examination and a written prescription from a doctor or other treating provider before Medicare helps pay for a power wheelchair.
Do you have to get prior authorization for a wheelchair?
Starting September 1, 2018, you may have to get prior approval (known as “prior authorization”) for certain types of power wheelchairs. Under this program, 40 types of power wheelchairs require “prior authorization” before Medicare will cover the wheelchair cost.
Can a DME provider provide a prior authorization for a wheelchair?
If your physician prescribes one of these wheelchairs to you, your DME supplier will, in most cases, submit a prior authorization request and all documentation to Medicare on your behalf . Medicare will review the information to make sure that you’re eligible and meet all requirements for power wheelchair coverage.
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
Coding Analyses for Labs (CALs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with CALs, from the Coding Analyses for Labs database.