Is a colonoscopy covered under Medicare?
Medicare covers screening colonoscopies once every 24 months if you’re at high risk for colorectal cancer. If you aren’t at high risk, Medicare covers the test once every 120 months, or 48 months after a previous flexible sigmoidoscopy. There’s no minimum age requirement.
Should we pay doctors less for colonoscopy?
May 20, 2021 · How often Medicare pays for a colonoscopy depends on your risk level. If you’re at a higher risk for colorectal cancer due to a family history or other factors, Medicare pays for you to have a screening colonoscopy every 24 months .
Why did Medicare charge me for a colonoscopy?
Nov 29, 2021 · Medicare sets limits on how often it will pay for colorectal cancer screenings, based on the type of procedure. Barium enema : Every four years for people at average risk of colorectal cancers; every two years for individuals at high risk.
What is the recommended age for a colonoscopy?
Jul 01, 2021 · How often Medicare pays for screening depends on your risk. For people considered high risk, a screening colonoscopy can be performed every 24 months. To be clear, this is not based on the calendar year but on actual months. If your last colonoscopy was 23 months ago, Medicare will not cover it as a free screening test.
Will Medicare pay for more than one colonoscopy a year?
Medicare covers screening colonoscopies once every 24 months if you're at high risk for colorectal cancer. If you aren't at high risk, Medicare covers the test once every 120 months, or 48 months after a previous flexible sigmoidoscopy.
How often do you need a colonoscopy after age 70?
Most people should get a colonoscopy at least once every 10 years after they turn 50. You may need to get one every 5 years after you turn 60 if your risk of cancer increases. Once you turn 75 (or 80, in some cases), a doctor may recommend that you no longer get colonoscopies.Jan 3, 2020
Does Medicare pay for colonoscopy after age 70?
Screening guidelines from the U.S. Preventive Services Task Force recommend screening for colon cancer with any method, including colonoscopy, from age 50 to 75. Medicare reimburses colonoscopy, regardless of age.Sep 26, 2016
How Much Does Medicare pay towards a colonoscopy?
Original Medicare pays the full cost of a colonoscopy if a medical provider who accepts Medicare rates does the procedure. However, if a polyp is found and removed during the colonoscopy, the procedure is considered diagnostic rather than preventive and you likely will owe 20 percent of the Medicare-approved fee.
At what age can a woman stop getting mammograms?
For women with no history of cancer, U.S. screening guidelines recommend that all women start receiving mammograms when they turn 40 or 50 and to continue getting one every 1 or 2 years. This routine continues until they turn about 75 years of age or if, for whatever reason, they have limited life expectancy.Feb 19, 2021
Why are colonoscopies not recommended after age 75?
“There are risks involved with colonoscopy, such as bleeding and perforation of the colon, and also risks involved with the preparation, especially in older people,” Dr. Umar said.Jun 15, 2021
Does Medicare cover anesthesia for colonoscopy?
Colonoscopy is a preventive service covered by Part B. Medicare pays all costs, including the cost of anesthesia, if the doctor or other provider who does the procedure accepts Medicare assignment. You don't have a copay or coinsurance, and the Part B doesn't apply.
What does Medicare consider high risk for colonoscopy?
Medicare covers a screening colonoscopy once every 24 months for people considered high risk,9 defined as having a history or a close relative with a history of colorectal polyps or cancer, a history of polyps, or inflammatory bowel disease like Crohn's disease or ulcerative colitis.
Is colonoscopy covered by Medicare Australia?
Items 32223, 32224, 32225 and 32226 have time intervals for repeat colonoscopy which are consistent with guidelines. These services are payable under Medicare only when provided in accordance with the approved intervals.Nov 1, 2019
Does Medicare pay for cologuard and colonoscopy?
Yes, Medicare will cover the cost of a Cologuard test every three years for those who qualify. Cologuard is the only stool-DNA test approved by the Food and Drug Administration for detecting colorectal cancer. Medicare Part B will cover a Cologuard test every three years if you: Are between the ages of 50 and 85.
Does Medicare cover colon polyp removal?
During a diagnostic colonoscopy, a doctor removes polyps or takes tissue biopsies. A person with Medicare will need to cover 20% of the Medicare-approved amount of the doctor's services, as well as a copayment if the doctor performs the procedure in a hospital setting.Mar 3, 2020
Is cologuard covered by Medicare?
Medicare Part B covers the Cologuard™ test once every 3 years for people with Medicare who meet all of these conditions: Between 50 and 85 years old.Oct 9, 2014
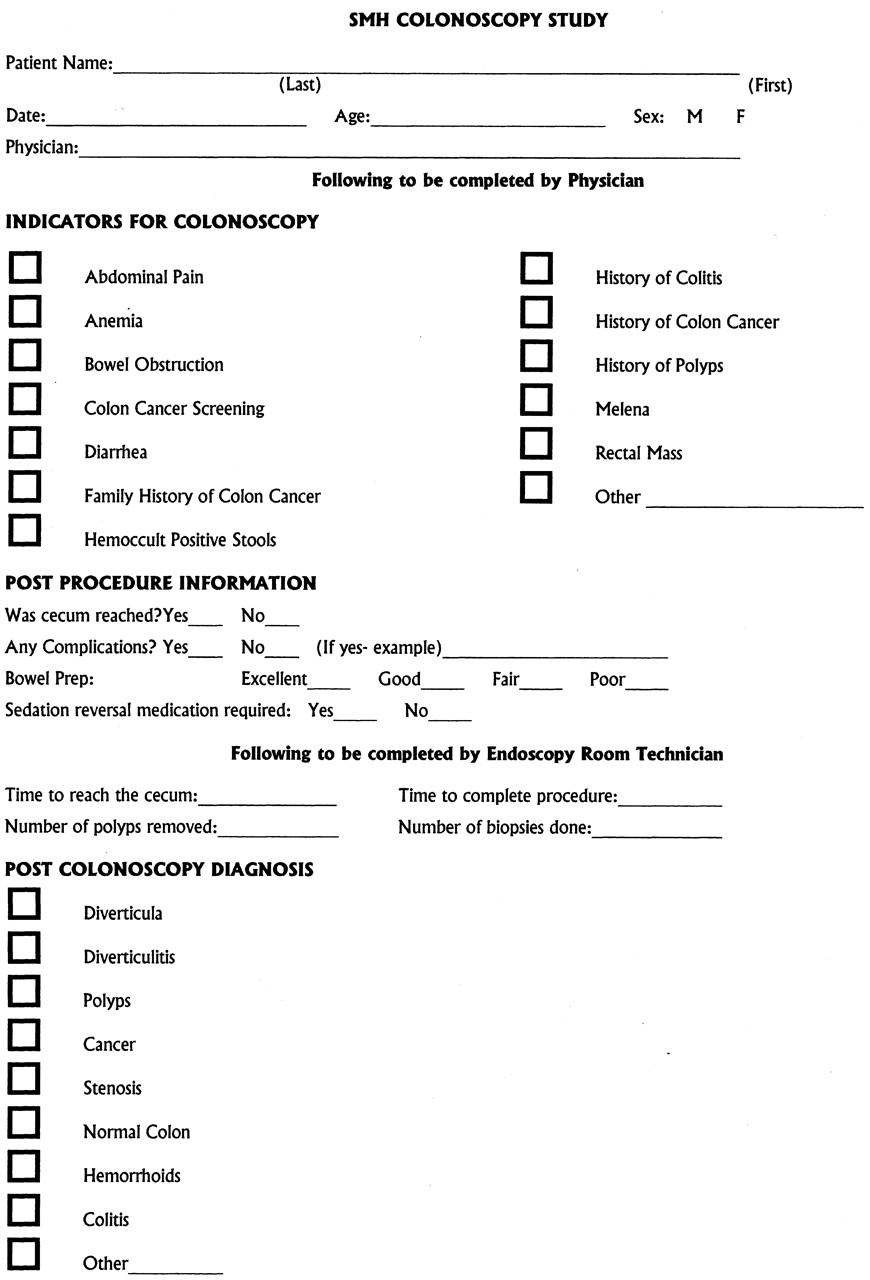
The Difference Between Screening and Diagnostic Colonoscopy
Tanya Feke, MD, is a board-certified family physician, patient advocate and best-selling author of "Medicare Essentials: A Physician Insider Explains the Fine Print."
Screening Colonoscopy
The goal of preventive medicine is to stop disease from happening whenever possible. It promotes healthy lifestyles and well-being for individuals and their communities.
Diagnostic Colonoscopy
Unlike screening tests, diagnostic colonoscopies are performed when someone has signs and symptoms. This includes, but is not limited to, blood in the stool, a change in bowel habits, decreasing blood counts (with or without anemia), or unintentional weight loss.
Screening Colonoscopy Turned Diagnostic
Imagine you are scheduled for a screening colonoscopy. During the procedure, your doctor finds a polyp. They have one of two choices: biopsy or remove the polyp, or complete the colonoscopy without an intervention.
Frequency of Colonoscopy Screening
How often Medicare pays for screening depends on your risk. For people considered high risk, a screening colonoscopy can be performed every 24 months. To be clear, this is not based on the calendar year but on actual months. If your last colonoscopy was 23 months ago, Medicare will not cover it as a free screening test.
A Word From Verywell
As a screening tool for colorectal cancer, colonoscopies set the standard. They allow your doctor to visualize the colon and to take action if they see any abnormalities.
Colorectal cancer: risk factors
Medicare pays for more frequent colonoscopies for people at high risk of developing colorectal cancer.
AARP In Your State
Visit the AARP state page for information about events, news and resources near you.
Medicare and Medicaid Overview
Medicare and Medicaid are government run medical programs that offer people who qualify health insurance and assistance with paying medical bills.
Medicare Colonoscopy Coverage
The Centers for Disease Control and Prevention and the US Preventive Services Task Force (USPSTF) support health authorities in their goal to screen at least 80% of people ages 50-75 for colorectal cancer by 2024.
Medicaid Colonoscopy Coverage
Medicaid is essentially a medical funding program that is run by the state and the determination of whether your colonoscopy is covered is dependent upon if your state approves. States are able to cover these screenings, but there is no assurance that you can get a free colonoscopy for a cancer screening.
Other Government Programs
Colorectal cancer is the second leading cause of deaths due to cancer in the United States. Screening for colorectal cancer is the best way to detect colorectal cancer at its earliest and most treatable stage. In 2018, 21.7 million people aged 50 to 75 in the United States have never been screened for colorectal cancer.
How Much Does Medicare Pay for a Colonoscopy?
Colonoscopy is a preventive service covered by Part B. Medicare pays all costs, including the cost of anesthesia, if the doctor or other provider who does the procedure accepts Medicare assignment. You don’t have a copay or coinsurance, and the Part B doesn’t apply.
Do I Have to Have a Colonoscopy?
Colon cancer is very treatable when found early, and colonoscopy is the gold standard screening test. There are other screening tests for colon cancer that you may want to discuss with your doctor. The important thing is to get screened.
Medicare Made Clear
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Get the Latest
Boost your Medicare know-how with reliable, up-to-date news and information delivered to your inbox every month.
Colonoscopy screening
Medicare covers screening colonoscopy costs as long as the doctor who performs the test accepts assignment.
Colonoscopy diagnostics
During a diagnostic colonoscopy, a doctor removes polyps or takes tissue biopsies.
Medicare Coverage for Diagnostic Colonoscopy
Diagnostic colonoscopies differ from preventive screenings. Therefore, diagnostics and preventives may have different costs; every plan may have its value set in place.
Does Medicare Cover Screenings for a Colonoscopy?
Part B pays all costs for preventive services, including the anesthesia used during the procedure. However, coverage is only when your doctor accepts the assignment.
Medicare and the Gastroenterologist
Be sure to talk to your plan directly or ask the doctor if they accept your insurance. However, not having a Gastroenterologist (GI) in your network is terrifying.
How Much Does a Colonoscopy Cost Out of Pocket?
The bill following a colonoscopy for an uninsured person can range from as low as $600 to more than $5,000. Out of pocket costs are different depending on location, CPT codes, and how long it takes. Self-pay patients should consider all the fees and compare rates before shelling out hundreds or thousands of dollars.
How Much Does Medicare pay for a Colonoscopy?
Part A or B pays for a colonoscopy in full when the procedure is preventive. The test becomes a diagnostic service when tissues or polyps are detected and removed.
How Often Does Medicare pay for a Colonoscopy?
Some patients are more likely than others for a colon cancer diagnosis. These patients are known as high-risk beneficiaries by CMS. After reaching one of Medicare’s requirements, at-risk patients are covered for one colonoscopy every two years, with zero out-of-pocket costs.
Will Medicare Pay for Colonoscopy after age 70?
Medicare starts paying for screenings at the age of 50 until 85 years or older. Stool DNA tests are otherwise known as Cologuard. Those showing no colorectal cancer symptoms or increased risks may get one Cologuard check every three years.