When does Medicare cover bi-level or BiPAP?
When does Medicare cover bi-level or BiPAP? Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive sleep apnea if the patient meets the criteria for PAP therapy (outlined above) and:
How many times a year does Medicare pay for CPAP?
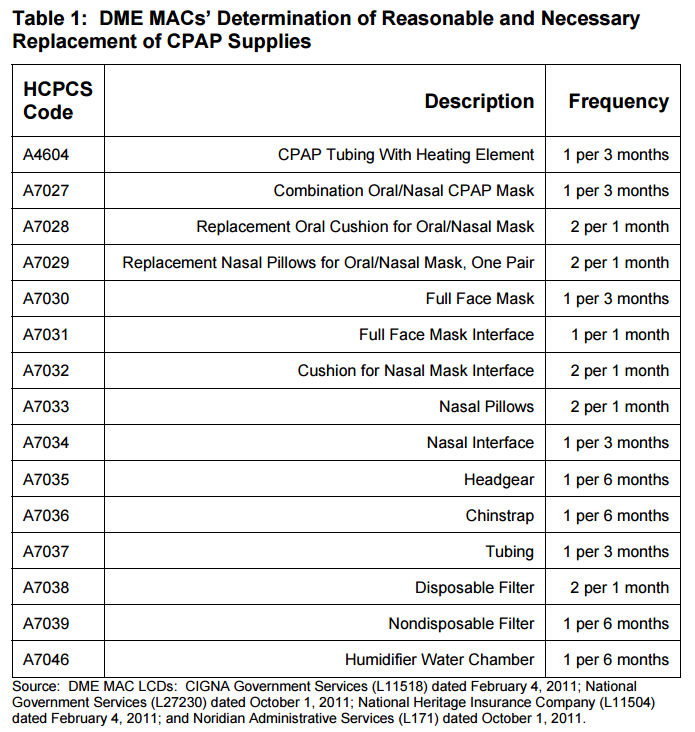
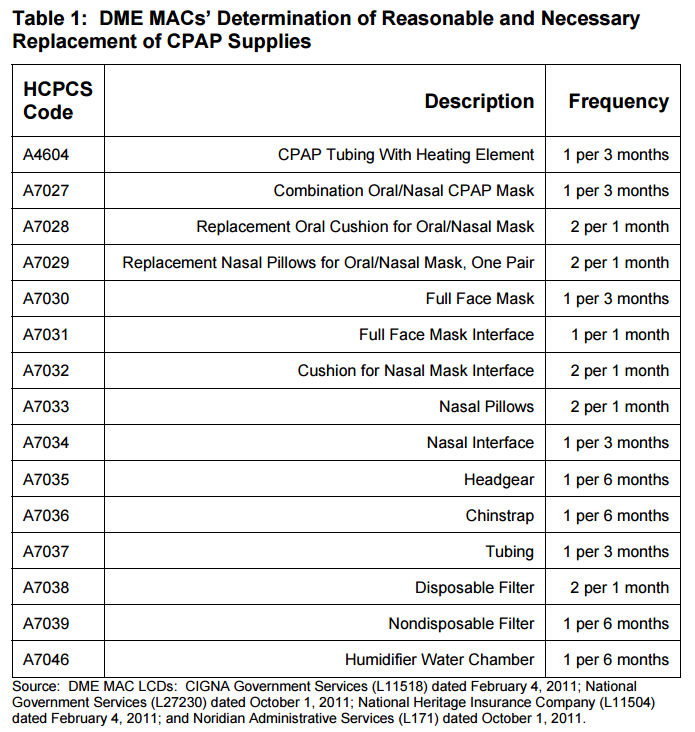
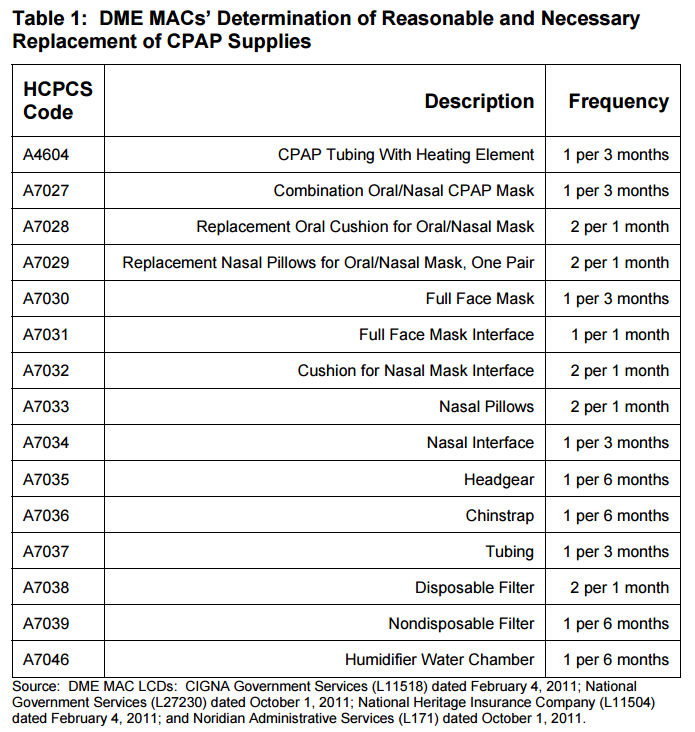
Below is a list of how many times per year Medicare will pay for a portion of certain CPAP supplies, according to the Department of Health and Human Services: humidifier water chamber: 2 times per year nondisposable filters: 2 times per year chinstrap: 2 times per year
How long will my CPAP or BiPAP equipment last?
Once you receive your CPAP or BiPAP equipment you will have it for a 3-month trial or 90 day compliance period. To meet compliance you will need to demonstrate daily usage of your CPAP for at least 70 to 85% of the period. This breaks down to about 4 hours per night.
Does Medicare Part B cover CPAP therapy?
We reviewed Medicare coverage for sleep studies here. In this post, learn about Medicare Part B coverage for CPAP and other PAP therapy (Part B covers certain doctor’s services, out patient care, medical supplies and preventative services).
Is Bipap covered by Medicare?
Yes, Medicare may cover rental or a replacement CPAP machine and/or CPAP supplies if you meet certain requirements.
How often can you get a new CPAP machine through Medicare?
every 5 yearsMedicare will usually cover a new CPAP machine every 5 years! This is also how long most manufacturers estimate that a CPAP machine will last, so even if your machine seems to be working, it's a good idea to replace it before it breaks down.
How often does Medicare pay for CPAP mask?
every 3 months11 For example, DME MACs will reimburse a supplier for a CPAP mask (A7034) every 3 months and a nondisposable filter (A7039) every 6 months.
How Long Will Medicare pay for CPAP supplies?
13 monthsfor the machine rental and purchase of related supplies (like masks and tubing). Medicare pays the supplier to rent a CPAP machine for 13 months if you've been using it without interruption. After Medicare makes rental payments for 13 continuous months, you'll own the machine.
How long does a Bipap machine last?
In general, CPAP machines are used for roughly three to five years. CPAP masks, however, should be replaced several times per year.
How often do you need a new CPAP machine?
approximately 5 yearsYour CPAP machine should be replaced after approximately 5 years of use. The good news is, Medicare and most other insurers typically provide coverage for a new CPAP machine around the same time frame.
Does Medicare pay for a replacement CPAP machine?
Medicare will only pay for a replacement CPAP device if it is lost, stolen, or irreparable damaged due to a specific incident; or if the equipment is older than 5 years old and is no longer functioning properly.
Does ResMed accept Medicare?
Do you accept either Medicare or Medicaid? Medicare and Medicaid will pay for medical equipment and supplies only if a supplier has a Medicare or Medicaid supplier number. Expedite, LLC, the operator of the ResMed Shop, does not have a Medicare or Medicaid supplier number.
How often does CPAP cover insurance?
Certain supplies need be replaced anywhere from every two weeks to every six months. Generally, insurance companies will authorize replacement of CPAP masks, tubing and filters every 90 days. Many insurance plans follow the guidelines from Medicare for regular replacement of supplies.
How many hours does Medicare require for CPAP?
Medicare Coverage of CPAP at Home Adherence to CPAP is defined as usage greater or equal to 4 hours per night on 70% of nights during a consecutive 30 days anytime during the first 3 months of initial usage.
How many hours per night should I use my CPAP machine?
If you're wondering, “how many hours per night should CPAP be used?” the answer is, for the entire night while you sleep, ideally 7+ hours. CPAP compliance measures how many hours and nights you use your therapy and if you use it often enough for effective treatment.
Do I own my CPAP machine?
After the rental period is over, you own the device. However, these insurance companies are often requiring proof that you are using the equipment and meeting their usage requirements (at least 4 hours per night for 70% of nights) in order to continue payment.
Does Medicare Cover CPAP and Other Pap Therapy For Sleep Apnea?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn...
How Does Medicare Define CPAP Compliance Or Adherence?
Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period...
What Is The Rental Term For Pap Therapy?
If the 3-month trial is successful (see above) Medicare will continue to cover the PAP device on a rental basis for up to 13 months in total up to...
Will Medicare Cover CPAP If I had A Machine Before I Got Medicare?
Yes, Medicare may cover rental or a replacement CPAP machine and/or CPAP supplies if you meet certain requirements.
When Does Medicare Cover Bi-Level Or Bipap?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive...
What Is Required in The Initial Face-To-Face Clinical Evaluation?
Written entries of the evaluation may include:History 1. Signs and symptoms of sleep disordered breathing including snoring, daytime sleepiness, ob...
What Information Does Medicare Require on The Prescription For CPAP and Supplies?
1. Beneficiary/patient’s name 2. Treating physician’s name 3. Date of order 4. Detailed description of items (type of device and supplies, pressure...
How Often Does Medicare Cover Replacement Pap Supplies?
Here’s an outline of the Medicare supply replacement schedule. For more detail (including how to tell when your equipment needs to be replaced, che...
How Much Will Medicare Pay For A CPAP Or Other Pap Machine?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insuranc...
How much does Medicare pay for a PAP?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insurance terms here ). If you have a secondary insurance, they may pick up the remaining 20% (read our post about how much sleep studies cost here ).
How long does it take to use CPAP for Medicare?
How does Medicare define CPAP compliance or adherence? Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period any time in the first three months of initial usage.
How long does a bi level CPAP trial last?
If the patient switches to a bi-level device within the 3-month trial, the length of the trial is not changed as long as there are at least 30 days remaining. If less than 30 days remain of the trial period, re-evaluation must occur before the 120th day (following the same criteria as CPAP adherence).
When does Medicare continue to cover PAP?
If you are successful with the 3-month trial of PAP, Medicare may continue coverage if the following criteria are met: Clinical re-evaluation between the 31st and 91st day after starting therapy, to include: Treating physician documents that the patient is benefiting from therapy; and.
Does Medicare cover bi level respiratory assist?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive sleep apnea if the patient meets the criteria for PAP therapy (outlined above) and:
Does Medicare require proof of usage?
Many other insurance companies are now following Medicare’s lead and requiring proof of usage before continuing to pay for the machine. Learn more about that here. If adherence to therapy is not documented within the first three months, the patient fails the trial period.
Who is Julia from Advanced Sleep Medicine?
in 2011 with a background in sales, marketing and customer service. She is currently the vice president of marketing and operations and enjoys the opportunity to educate and interact with those looking to improve their health through better sleep.
Medicare Coverage for CPAP Machines
Caitlin McCormack Wrights has over a decade of experience writing hundreds of articles on all things finance. She specializes in insurance, mortgages, and investing and relishes making dull subject matter gripping and everyday topics amazing. Caitlin has a bachelor's from Duke and a master's from Princeton.
When Will Medicare Cover CPAP Machines?
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study.
How To Get Medicare To Cover a CPAP Machine
Medicare will cover a CPAP machine if you meet two conditions. You must first be diagnosed with obstructive sleep apnea, and you must submit your primary doctor’s order or prescription to the right supplier to receive coverage. Here are the steps you’ll need to take to make that happen.
How Much Does a CPAP Machine Cost With Medicare?
Medicare typically covers the most basic level of equipment, and it may not pay for upgrades. In the case where Medicare doesn’t cover upgrades or extra features, you’ll need to sign an Advance Beneficiary Notice (ABN) before you get the equipment.
The Bottom Line
The rules of how DMEs are covered, including CPAP machines, are generally the same whether you have Original Medicare or a Medicare Advantage Plan. However, the amount you pay with Original Medicare and a Medicare Advantage Plan may often differ. Compare Medicare and Medicare Advantage to learn more.
How often can I get a new CPAP machine while on Medicare?
Once you’ve continuously used your CPAP machine for the approved 13-month rental, you will own it. However, CPAP supplies may lose effectiveness with use, and Medicare covers their replacement. Guidelines suggest replacing a CPAP mask every three months and a non-disposable filter every six months. 4
How do I get CPAP supplies covered by Medicare?
Medicare will only help cover CPAP supplies and accessories if you get them from a Medicare-approved contract supplier after completing the necessary medical steps.
How much is Medicare Part B deductible?
Part B deductible. The Medicare Part B deductible is $185 per year in 2019. You must meet your deductible before your Part B coverage will kick in. Part B coinsurance or copayment. You are typically responsible for 20 percent of the Medicare-approved amount for the CPAP machine cost, including filters, hoses and other parts.
What is Medicare Advantage?
Medicare Advantage plans cover everything that Part A and Part B cover, and some plans include extra benefits not covered by Original Medicare. These additional benefits may include coverage for services like: Prescription drugs. Dental care.
Does Medicare have an out of pocket spending limit?
Medicare Advantage plans also include an annual out-of-pocket spending limit, which Original Medicare (Part A and Part B) doesn’t include. This spending limit can potentially save you money in Medicare costs for your CPAP machine.
Does Medicare cover CPAP machines?
Medicare typically covers CPAP machines if your doctor says it’s medically necessary. Medicare Advantage plans may also cover CPAP machines, and some plans offer additional benefits such as prescription drug coverage. Medicare typically does cover CPAP machines that are deemed medically necessary by a doctor.
How often does Medicare pay for CPAP?
nondisposable filters: 2 times per year. chinstrap: 2 times per year.
How long can you rent a CPAP machine?
CPAP rental for 13 months if you’ve been using it consistently (after 13 months , you’ll own the CPAP machine) masks or nose pieces you wear when using the machine. tubing to connect the mask or nose piece to the machine. This Medicare coverage applies only if your doctor and supplier participate in the Medicare program.
What is Medicare Part B?
Medicare Part B is the section that pays for durable medical equipment (DME), such as CPAP machines. To have your CPAP machine covered, you need to make sure that your clinician and device supplier participate in the Medicare program.
How long does a CPAP machine last?
Your CPAP machine is paid for after 13 months and you’ll own it, but it should last several years . You may have it replaced with your medical benefit after this time.
Does Medicare cover CPAP machines?
Medicare will cover a part of the cost of a CPAP machine if you’ve been diagnosed with obstructive sleep apnea. Coverage for CPAP machines falls under the Medicare Part B coverage of durable medical equipment. You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs.
Do you pay for a CPAP machine?
You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs. A continuous positive airway pressure (CPAP) machine is a medical device that gives you extra oxygen with a bit of force.
Why do you need to replace CPAP supplies?
Because your CPAP supplies must be replaced on a regular basis to keep your CPAP working like new. Plus, this is crucial to keeping your equipment free of viruses, germs, or other harmful pathogens and prevents air leaks.
When do you have to meet with your doctor for CPAP?
You are required to meet with your doctor between the 31st and 90th day during the compliance period (and no later than the 90th day) for your doctor document that CPAP therapy is helping you and to ensure compliance. CPAP compliance is generally tracked by your machine via Bluetooth or by using an SD card.
How old do you have to be to get Medicare?
To enroll you must be age 65 or older and you must be a U.S. citizen or a permanent resident for five consecutive years. You may automatically enroll in Medicare part A if you already receive benefits from Social Security or the Railroad Retirement Board (RRB).
Can you get CPAP supplies covered by Medicare?
If you’re avoiding replacing your CPAP equipment because it might be too expensive or a time-consuming hassle, then we have good news. Once you turn 65 you can get CPAP supplies covered through Medicare.
Is a PCP a Medicare?
Make sure your primary care physician (PCP) is enrolled in Medicare, otherwise you’ll be responsible for the payment . Your PCP must also physically document office notes and medical records that explain that a PAP (positive airway pressure) device is necessary and beneficial for your health.
Does Medicare cover CPAP?
Wait, does Medicare cover CPAP supplies? Really?! Yes, and they may cover a new CPAP machine too, if yours is older than five years old. You just have to be diagnosed with sleep apnea and follow Medicare’s guidelines.
Get A Second Clinical Evaluation
If Medicare covers your CPAP machine for the three-month trial period, you must undergo a second clinical evaluation to establish medical necessity for continued coverage. During the face-to-face evaluation, your doctor must document that your symptoms of sleep apnea have improved and that youve adhered to consistent CPAP therapy.
Does Medicare Pay For Cpap Machines And Supplies
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here’s how we make money.
How Do You Treat Sleep Apnea
Mild cases of sleep apnea are often managed through simple lifestyle changes such as quitting smoking, losing weight or treating nasal allergies. For individuals who have a moderate or severe case of sleep apnea, treatment may be more complex, and can include supplemental oxygen, oral appliances or airway-pressure devices, including CPAP machines.
What Are Medicare Guidelines For Cpap
You have a three-month trial period covered by Medicare. After three months, your doctor will check how the treatment is working for you. Medicare may cover CPAP therapy long-term if your doctor verifies in your medical record that:
Option : Use Medicares Website
If you have a Medicarehealthcare plan, you can also find in-network durable medical equipment providers by using Medicares Supplier Directory. After you click the link, enter your zipcode and select the corresponding product category. For CPAP machines and related supplies, select .
When Should I Contact My Private Insurance
Once you think you have sleep apnea, check with your insurance company to find out what type of coverage you get for CPAP.
Insurance And Cpap Machines
The terms of your CPAP machine, insurance coverage depends on your provider. Some providers reimburse you for the cost of purchasing the machine outright, while others require a rent-to-own plan under which you must use the machine for a set amount of time before it becomes your property.
What Does Medicare Cover
Federally managed Medicare has four parts, which include Part A and Part B , together known as original Medicare. The two other parts of Medicare are Part C, also known as Medicare Advantage, and Part D .
Does Medicare Cover Sleep Apnea Treatment With A Cpap Machine
In most cases, Medicare generally covers 80% of the allowable charges related to a sleep apnea machine.
Option : Use Medicares Website
If you have a Medicarehealthcare plan, you can also find in-network durable medical equipment providers by using Medicares Supplier Directory. After you click the link, enter your zipcode and select the corresponding product category. For CPAP machines and related supplies, select .
Will Medicare Supplement Plans Pay For My Cpap Machine
Between five and 20 percent of the adult population has sleep apnea, though the National Sleep Foundation suggests that the numbers may be underreported. People of all ages can develop sleep apnea, and as you get older, you might need a CPAP machine. But will Medicare Supplement plans pay for your durable medical equipment?
Will Medicare Cover A Cpap Machine
Medicare covers CPAP machines used to treat sleep apnea under the durable medical equipment benefit. To qualify for CPAP coverage, you must meet the following requirements:
Sleep Apnea And Medicare
Navigating coverage for sleep apnea can be tricky, but luckily, Medicare often picks up a majority of the cost. If youre diagnosed with obstructive sleep apnea, you may qualify for CPAP therapy, including routine accessories for your CPAP machine.
How Much Do Positive Airway Pressure Machines Cost
The cost of a positive airway pressure machine depends on the unit’s quality and features, and prices for standard CPAP machines typically range between $250 and $1,000.