Is Cologuard covered by United health care?
Apr 14, 2019 · Medicare includes coverage for colorectal cancer screening, including a Cologuard kit under specific circumstances. A stool DNA test (Cologuard) will be covered by Medicare every 3 years for people 50 to 85 years of age who do not have symptoms of colorectal cancer and who do not have an increased risk of colorectal cancer.
Is the ColoGuard test covered by Medicare?
Sep 20, 2021 · How Often Does Medicare Pay for the Cologuard Test? Part B will cover the Cologuard test once every three years if you meet the following criteria. At average risk Age 50-85 Asymptomatic You should have a good understanding of what will affect your screening for colorectal cancer.
Does United Healthcare cover Cologuard?
Jan 19, 2022 · Typically, Medicare Part B does pay for Cologuard tests every three years if you meet all of the following conditions: You show no signs or symptoms of colorectal disease. You are 50-85 years old. You have no personal history of colorectal cancer, inflammatory bowel disease or adenomatous polyps. You have no family history of hereditary nonpolyposis …
Is Cologuard covered by insurance?
Jan 06, 2022 · A screening colonoscopy is covered by Original Medicare as often as every 24 months for those at very at high risk, or once every 10 years if you are not at high risk. There is no minimum age requirement if medically-indicated by risk. Cologuard is the brand name of a test that you might have seen on television. It is less invasive than colonoscopy, and is an …
How often will Medicare pay for cologuard test?
once every 3 yearsMedicare Part B covers the Cologuard™ test once every 3 years for people with Medicare who meet all of these conditions: Between 50 and 85 years old.Oct 9, 2014
Can you do cologuard every year?
A Cologuard test should be done every three years rather than annually due to the higher cost and false-positive rates compared to an annual FIT. More research is needed to determine how often the Cologuard test should be done.Feb 6, 2022
How often should cologuard be repeated?
How often do you need to repeat the test – Cologuard must be repeated every three years if you've never had a positive result. Once you have had a positive result, you will need to have diagnostic colonoscopies for further screening exams.Oct 4, 2019
Will Medicare pay for a colonoscopy after a positive cologuard?
Yes, Medicare will cover the cost of a Cologuard test every three years for those who qualify. Cologuard is the only stool-DNA test approved by the Food and Drug Administration for detecting colorectal cancer. Medicare Part B will cover a Cologuard test every three years if you: Are between the ages of 50 and 85.
Which is better colonoscopy or cologuard?
Cologuard vs Colonoscopy According to GI Alliance, Cologuard can miss up to 8% of colon cancer and more than 50% of pre-cancerous polyps. Stool DNA (Cologuard) testing is designed to detect and not prevent cancer. A colonoscopy is the only test that both detects and prevents colon cancer.Jan 15, 2022
Is cologuard cheaper than a colonoscopy?
As for cost-effectiveness, at $599 — of which Medicare is expected to pay $502 — Cologuard is more expensive than FIT, but less than colonoscopy.Dec 3, 2014
At what age do you stop having mammograms?
The age to stop screening with mammography should be based on each woman's health status rather than an age-based determination. In average-risk women aged 75 years or older or in women with a life expectancy of 10 years or less, clinicians should discontinue screening for breast cancer.Sep 22, 2020
How often are colonoscopies recommended?
Because colonoscopy testing is highly accurate and colorectal cancer tends to grow slowly, most experts recommend that people at average risk should have a baseline colonoscopy at age 50, then repeat the exam every 10 years.Feb 1, 2020
Why do I need a repeat colonoscopy in 3 years?
Patients in the high-risk group have three or more adenomas or polyps 1 cm or larger, or high-grade dysplasia, and should have a repeat colonoscopy in three years.Apr 1, 2008
Does Medicare cover colonoscopy after age 70?
The US Preventive Services Task Force recommends screening guidelines to include all colon cancer tests, any method from ages 50 to 75. However, Medicare pays or reimburses the costs of a colonoscopy – no matter the age.Sep 28, 2021
Why are colonoscopies not recommended after age 75?
“There are risks involved with colonoscopy, such as bleeding and perforation of the colon, and also risks involved with the preparation, especially in older people,” Dr. Umar said.Jun 15, 2021
How often do you need a colonoscopy after age 70?
For those opting to undergo colonoscopies (other screening options include a fecal occult blood test and flexible sigmoidoscopy), the procedure should be done every 10 years, and is not needed after age 75.Mar 12, 2013
How often does Part B cover Cologuard?
Part B will cover the Cologuard test once every three years if you meet the following criteria: At average risk. Age 50-85. Asymptomatic. You should have a good understanding of what will affect your screening for colorectal cancer. The Affordable Care Act requires insurance companies to abide by the USPSTF recommendations for coverage.
What to do if you don't see your state on Cologuard?
If you don’t see your state, don’t worry because Cologuard is adding new states and plans all the time. Check back often, and if you’re considering canceling your test, call their Customer Care Center first. You can request more information about the financial assistance program that Exact Sciences offers.
How much does a blood test cost?
The price of the test can range from $400-$600. Although, talking with your insurance provider can help; you can request fees for the test and laboratory be covered. You don’t know unless you ask. More than 92% of all patients have a $0 out-of-pocket cost for testing.
Does Medicare cover colorectal screening?
Medicare is exempt from this requirement; beneficiaries might be responsible for paying coinsurance or co-payments. Look over your plan, make sure you have a good understanding of what type of insurance you have, and what service options your plan covers for colorectal screening, including Cologuard.
Can you get co-insurance with Medicare?
Most people with Medicare won’t be responsible for co-insurance if they get a Cologuard kit. Reaching the next stage of life presents new screenings that you should talk to your doctor about. One of several options is Cologuard; however, your doctor or healthcare provider must give you a prescription.
Do you have to come out of pocket with Medicare?
Beneficiaries with Medicare Advantage plans or other insurance plans besides Medicare may need to come out-of-pocket for some expenses. Any Medicare member and those with other insurance types whether private or public should contact their insurance plan provider about coverage.
Does Exact Sciences have a contract with Medicare?
They’re not on contract with Medicare in every state; for instance, in New York, Cologuard is a preventative service for Medicaid members. Then, some states will allow Exact Sciences to contact directly Medicaid plans in the states they’re not participating.
How often does Medicare pay for Cologuard?
Typically, Medicare Part B does pay for Cologuard tests every three years if you meet all of the following conditions: You have no personal history of colorectal cancer, inflammatory bowel disease or adenomatous polyps. You have no family history of hereditary nonpolyposis colorectal cancer, familial adenomatous polyposis, ...
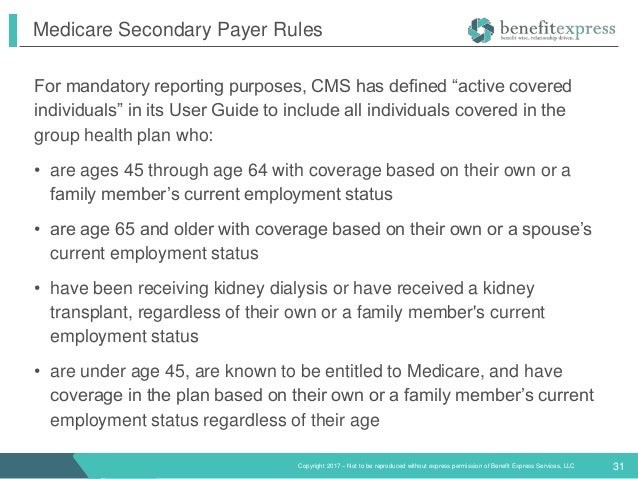
How often is a barium enema covered by Medicare?
Barium enema. This test is covered by Medicare every 48 months if you are age 50 or older and every 24 months if you are at a high risk for colorectal cancer. Colonoscopy. This test is covered every 24 months if you are at a high risk for colorectal cancer. Fecal occult blood test.
How many Medigap plans are there?
In most states, there are 10 standardized Medigap plans to choose from, with a range of available basic benefits.
Can you get Cologuard if you have a family history?
You have no family history of hereditary nonpolyposis colorectal cancer, familial adenomatous polyposis, colorectal cancers or adenomatous polyps. Typically, you pay nothing for Cologuard (if it is prescribed by a doctor who accepts Medicare assignment).
Types Of Colorectal Cancer Screening
Because colon cancer begins as growths called polyps, finding and removingpolyps is the best way to prevent colon cancer. There are three types of CRC screening:
Colorectal Cancer Screening In Patients With Cystic Fibrosis
An UpToDate review on Cystic fibrosis: Overview of gastrointestinal disease states that The Cystic Fibrosis Foundation has developed Guidelines for Colorectal Cancer Screening for adults with CF. The guideline recommends colonoscopy for screening, beginning at age 40 years, or at 30 years for those who have had an organ transplant.
What Colonoscopy Costs Does Medicare Cover
Medicare covers all costs associated with a colonoscopy screening for colorectal cancer so long as the doctor who does it accepts Medicare.
The Affordable Care Act
Regardless of the insurance you are having, the Affordable Care Act mandates the insurance providers to follow the guidelines of the U.S. Preventive Services Task Force for coverage. If the screening test has received an A or B rating by this agency, private insurance companies would cover the cost of the test without charging a co-pay.
What Are The Screening Guidelines For Cologuard Under Medicare
The U.S. Preventative Services Task Force guidelines for screening for colorectal cancer do NOT include the testing of stool DNA. On the other hand, several agencies and societies do review these tests.
Medicaid Coverage For Colorectal Cancer Screening
States are authorized to cover colorectal screening under their Medicaid programs. But unlike Medicare, theres no federal assurance that all state Medicaid programs must cover colorectal cancer screening in people without symptoms. Medicaid coverage for colorectal cancer screening varies by state.
Who Needs A Colonoscopy
The U.S. Preventive Services Task Force recommends that people at average risk of colorectal cancer should have regular colonoscopies starting at age 50. The American Cancer Society recommends people start screening at 45.
What is a Cologuard test?
Cologuard is a diagnostic tool manufactured by Exact Sciences used for the assessment of colon cancer. If your physician has recommended this test, it would be advisable to check whether it is covered by Medicare or any other insurance policy.
Does Medicare cover screening tests?
If the screening test has received an A or B rating by this agency , private insurance companies would cover the cost of the test without charging a co-pay. But, Medicare is exempted from this mandate and you may need to pay co-pays and co-insurance.
Can Cologuard detect colorectal cancer?
Currently, the US Multi-Society Task Force on Colorec tal Cancer, the Joint Guideline from the American Cancer Society, and the American College of Radiology have recommended DNA tests of stools using Cologuard kit to detect colorectal cancer. But, the U.S. Preventive Services Task Force guidelines for the screening of colorectal cancer have not ...
Is Cologuard covered by Medicare?
Earlier Cologuard was not covered by Medicare and most other insurance policies. However, a few years back, the Centers for Medicare & Medicaid Services (CMS) made an announcement that Cologuard would be covered by Medicare based on the CMS National Coverage Decision.
Is Cologuard a good test?
While there are several other screening options to test the presence of blood in the stools, the Cologuard test is considered superior for the accurate results it provides.
Does Medicare require stool DNA testing?
But, the U.S. Preventive Services Task Force guidelines for the screening of colorectal cancer have not been modified to include stool DNA testing. However, Medicare is not bound by the professional guidelines recommended by these agencies.
