
The Medicare Part B drug payment system is used by Medicare to reimburse health care providers for the average costs of the drugs they administer when providing outpatient services to Medicare beneficiaries. Reimbursement to individual providers is based on a formula computed from national sales data, not on the price paid by a specific provider.
What is the maximum premium for Medicare Part B?
The standard monthly premium for Part B, which covers outpatient care and durable equipment ... or offers a different copay and an out-of-pocket maximum (a Medicare Advantage Plan). The Aduhelm situation highlights the ripple effect that expensive drugs ...
What are the rules for Medicare Part B?
Fact sheet FACT SHEET: Most Favored Nation Model for Medicare Part B Drugs and Biologicals Interim Final Rule with Comment Period
- Background. High drug prices are impacting the wallets of Medicare beneficiaries through increased premiums and out-of-pocket costs.
- Model Design
- Participants. ...
How much does Part B insurance cost?
Part B costs: What you pay 2021: Premium $170.10 each month (or higher depending on your income). The amount can change each year. You’ll pay the premium each month, even if you don’t get any Part B-covered services.
How high will the Medicare Part B deductible get?
The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
What is Medicare Part B reimbursement?
What is ASP in Medicare?
What are the direct impacts of the Medicare Modernization Act?
What is separately payable drug?
Does Medicare have power to pay for drug prices?
Does Medicare Part B have future prices?
Do insurers reimburse for drugs?
See more
About this website
How do I get reimbursed for Medicare Part B?
You may be reimbursed the full premium amount, or it may only be a partial amount. In most cases, you must complete a Part B reimbursement program application and include a copy of your Medicare card or Part B premium information.
How do doctors get reimbursed from Medicare?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
How Does Medicare pay providers in Part B?
If the provider accepts assignment (agrees to accept Medicare's approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ).
How does the Part B reimbursement work?
The Medicare Part B Reimbursement program reimburses the cost of eligible retirees' Medicare Part B premiums using funds from the retiree's Sick Leave Bank. The Medicare Part B reimbursement payments are not taxable to the retiree.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What is the Medicare reimbursement rate?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How much does Medicare Part B pay for physician fees quizlet?
Part B of Medicare pays 80% of physician's fees (based upon Medicare's physician fee schedule) for surgery, consultation, office visits and institutional visits after the enrollee meets a $185 deductible/yr. (2019). Then the patient pays 20% coinsurance of the Medicare approved amount for services.
Does Medicare pay for providers?
Physicians and other health professionals: Medicare reimburses physicians and other health professionals (e.g., nurse practitioners) based on a fee-schedule for over 7,000 services.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
2022 ASP Drug Pricing Files | CMS
Notice of Pricing Changes for the April 2022 Medicare Part B Quarterly Average Sales Price Pricing File This announcement serves as notification of the process that we used to substitute the WAMP for the ASP for Aduhelm in the April 2022 ASP pricing files, consistent with our regulations at 42 CFR 414.904(d), based on the findings of the OIG that the ASP used to set the Medicare Part B payment ...
2021 ASP Drug Pricing Files | CMS
The Medicare Part B Drug and Biological Average Sales Price Quarterly Payment files for calendar year 2021 are located in the "Downloads" section below.
Billing and Coding Guidelines for Drugs and Biologics (Non-chemotherapy ...
Billing and Coding Guidelines for Drugs and Biologics (Non-chemotherapy) L 34741 . Medicare Excerpts: CMS 100-02, Medicare Benefit Policy Manual, Chapter 15- Section 50 - Drugs and Biologicals: 50.2 - Determining Self-Administration of Drug or Biological
Billing and Coding Guidelines for Drugs and Biologics (Non-chemotherapy ...
remainder is discarded. (except those provided under the Competitive Acquisition Program (CAP) for Part B drugs and biologicals). Providers must document the discarded drugs or biologicals in the patient's medical record.
What is Medicare Part B reimbursement?
One of the keys to understanding Medicare Part B reimbursement is “ assignment ,” which can be confusing for those not familiar with medical insurance terminology. Medicare’s definition of an assignment is “an agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for ...
What percentage of Medicare Part B is paid?
The approved amount is also sometimes referred to as the Medicare Fee Schedule. Medicare Part B pays 80 percent of its approved amount. The remaining 20 percent that can be billed to the patient is known as the Medicare coinsurance.
What is Medicare coinsurance?
Medicare coinsurance is your responsibility. Finding providers who accept assignment will save you money and the potential issues of filing your own claim. Medicare claims are processed by contracted insurance providers known as MACs. You have the right to appeal any decision by Medicare.
How much is Medicare Part B deductible?
Medicare Part B has an annual deductible that is currently set at $198 per year. Medicare will not pay anything under Part B until that amount is paid by the patient.
What is billed fee?
The billed amount, or professional fee, is simply the amount for a service or item that appears on a provider’s bill. If no insurance was involved, that is the amount a patient would be charged. The Medicare-approved amount is what Medicare would pay for any covered service or item.
What is an appeal in Medicare?
An appeal is an action you can take if you disagree with the way your claim was processed. If you believe a service or item was denied in error, or you disagree with the amount of payment, you have the right to appeal. You may also appeal if Medicare stops paying for an item or service that you are currently receiving and believe you still need.
Who handles Medicare Part B claims?
All Medicare Part B claims are processed by contracted insurance providers divided by region of the country. The current term for these providers is “Medicare administrative contractors” (MACS).
How much does Medicare cost?
Medicare Part premiums are currently set at $99.90 for most seniors with Medicare. That’s not expensive for what it covers, but it adds up to nearly $1,200 per year. Considering the medical coverage they’re getting, most people don’t mind shelling out that $1,200. But there are some lucky people who don’t have to.
Can you get full reimbursement for Part B?
If you pay more than the standard Part B premium, you may be eligible for full reimbursement. Some pension plans may offer reimbursement only up to the standard premium amount.
Do Medicare Part B patients get reimbursed?
Correction. They do pay their Medicare Part B premiums—but then they get reimbursed for what they paid .
What is Medicare Part B reimbursement?
Medicare Part B Reimbursement of Drugs prior to the Medicare Modernization Act. The Medicare Part B drug payment system is used by Medicare to reimburse health care providers for the average costs of the drugs they administer when providing outpatient services to Medicare beneficiaries.
What is ASP in Medicare?
By law, a drug's ASP is defined as the volume-weighted average manufacturer sales price net of all rebates, discounts, and other price concessions to U.S. purchasers, excluding sales that are exempt from Medicaid "best price" calculations and sales to other federal purchasers. 11 Manufacturers are required to provide CMS with the quarterly sales price and volume of sales for each covered drug by National Drug Code (NDC) within 30 days of the end of the quarter. Because multiple manufacturers may produce the same drug, CMS crosswalks NDCs for the same drug using the Healthcare Common Procedure Coding System (HCPCS). CMS then calculates a volume-weighted ASP for each HCPCS code, which becomes the basis for the reimbursement rate for the following quarter. Given the time needed to submit and process sales data, the current reimbursement rate always reflects a drug's ASP from two quarters prior. Figure 1 shows the timeline for establishing Medicare Part B reimbursement rates.
What are the direct impacts of the Medicare Modernization Act?
Following the MMA changes to the Medicare Part B drug payment system, MedPAC issued two Congressionally-mandated reports, which found that health care providers could still purchase most covered drugs at prices below the Medicare Part B reimbursement rate. 15, 16.
What is separately payable drug?
10 42 C.F.R. § 419 as amended. Separately payable drugs are those that are not packaged within an ambulatory payment classification group because their average cost per day of treatment exceeds $80. The Medicare Hospital Outpatient Prospective Payment System (OPPS) has typically reimbursed these drugs at ASP plus a 4 to 6 percent margin.
Does Medicare have power to pay for drug prices?
Under this acquisition process, Medicare has no price-setting power reimbursement rates lag rather than lead market prices. Empirical analysis of quarterly ASPs and reimbursement rates for covered drugs shows that market prices vary considerably over time and occasionally experience sharp spikes. In general, however, previous studies have found that most providers could still purchase most covered drugs at or below the reimbursement rate.
Does Medicare Part B have future prices?
Medicare Part B reimbursement rates do not establish future prices - they are based on prices previously obtained in the market. Thus, shortages (or surpluses) of a given drug will lead to price increases (or decreases), just as had been the case before the MMA.
Do insurers reimburse for drugs?
Unlike the many other medical supplies that providers routinely buy in the private market, insurers often separately reimburse providers for the cost of these drugs, rather than expecting providers to cover these costs as part of their global reimbursement. The prices of the drugs themselves, however, are not subject to price regulation ...
What would happen if manufacturers wanted to respond to the Medicare reimbursement reductions under the proposed policy?
As a result, if manufacturers wanted to respond to the Medicare reimbursement reductions under the proposed policy by cutting prices of drugs going to Medicare beneficiaries but not those with employer-based coverage, substantial changes in the distribution system would be required.
How would biosimilars affect Medicare?
Medicare would pay the same reimbursement based on the weighted average sales of all innovator and biosimilar products in the code. This would change the physician incentive substantially, while also lowering beneficiary co-insurance. It is not surprising that in the U.S. many approved biosimilars have not yet been marketed—physicians have no incentive to use the biosimilars if they earn more by administering the innovator medicine. (A separate factor that might partially explain why biosimilars in the US lag those in Europe might involve the prevalence of aggressive patent challenges in the US).
What does "best price" mean in Medicare?
And Medicaid “best price” rules would mean that a manufacturer’s price reduction to help physicians to avoid losses when administering drugs to Medicare payments would also reduce the amounts that can be charged to Medicaid agencies.
How would the proposed policy affect Medicare?
The proposed policy would likely radically disrupt economic incentives for physicians. It and make what Medicare pays for some medicines systematically less than physicians’ acquisition and administrative cost, which would cause them to lose money when administering those drugs. Large financial losses would limit access for Medicare patients to medically needed medicines, as projected by the Medicare Actuary.
How many Medicare beneficiaries would lose access to drugs?
Indeed, the Medicare Actuary (Table 11) estimates that 1 in 5 Medicare beneficiaries—such as cancer patients—would lose access to drugs subject to this regulation, with another 1 in 10 Medicare patients forced to shift where they get their care to access these drugs. In addition, implementation on such short notice would lead to administrative ...
What are the changes to the buy and bill system?
Changes in “Buy and Bill.” Other reforms propose more substantial changes in the buy and bill system for physicians, such as not having physicians take ownership of drugs—they would be paid an amount for storage and administering the drug. Their patients would then benefit from the physician using the lower-priced drugs and the physician earnings would not be impacted by which alternative they administer. Or vendors could be created to act on behalf of physicians to negotiate prices with manufacturers, seeking discounts in return for steering volume to the drug being discounted. Vendors, which could include large medical practices, would have to influence affiliated physicians to shift utilization toward the lower cost drugs. This would be analogous to the role that PBMs play with pharmacy-dispensed drugs.
Is there regulation for Part B?
Regulation. Nevertheless, with an important share of Part B drug spending for medicines without the prospect for effective competition, engaging market forces and competition cannot address a large part of the problem; regulation would be required. Given the distribution system for physician-administered drugs and concerns about maintaining patient access, regulation would need to apply to manufacturer prices rather than what Medicare pays. Extending regulated prices beyond Medicare Part B would reduce health spending on medicines (but concomitantly lower manufacturer revenues). When private insurers pay too much for drugs, that drives up premiums, burdening employers and employees that purchase coverage and government, which subsidize both employer-based coverage (through the tax system) and subsidizes individual coverage directly. However, fewer drugs might be developed if potential returns are reduced.
What is Medicare reimbursement?
A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay.
How many psychiatrists have opted out of Medicare?
Of the tiny fraction of doctors who have opted out of Medicare entirely, 42 percent are psychiatrists. And although the number of doctors opting out increased sharply from 2012 to 2016, it dropped in 2017, with 3,732 doctors opting out.
What is Medicare participating provider?
Physicians who agree to fully accept the rates set by Medicare are referred to as participating providers. They accept Medicare’s reimbursements for all Medicare-covered services, for all Medicare patients, and bill Medicare directly for covered services. Most eligible providers are in this category. A Kaiser Family Foundation analysis found that ...
Does Medicare pay for the entire bill?
If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill; Medicare will not reimburse the doctor or the patient for any portion of the bill, and the provider can set whatever fees they choose.
Can a doctor opt out of Medicare?
A small number of doctors (less than 1 percent of eligible physicians) opt out of Medicare entirely, meaning that they do not accept Medicare reimbursement as payment-in-full for any services, for any Medicare patients. If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill;
Can a physician accept Medicare reimbursement?
Because the reimbursement rates are generally lower than physicians receive from private insurance carriers, some physicians opt to be non-participating providers. This means that they haven’t signed a contract agreeing to accept Medicare reimbursement as payment-in-full for all services, but they can agree to accept Medicare reimbursement ...
What happens if you don't pay Medicare Part B?
If you don't pay your monthly Medicare Part B premiums through Social Security, the giveback benefit would be credited to your monthly statement. Instead of paying the full $148.50, you'd only pay the amount with the giveback benefit deducted.
How to find Part B buy down?
If you enroll in a plan that offers a giveback benefit, you'll find a section in the plan's summary of benefits or evidence of coverage (EOC) that outlines the Part B premium buy-down. Here, you'll see how much of a reduction you'll get. You can also call us toll-free at 1-855-537-2378 and one of our knowledgeable, licensed agents will answer your questions and explain your options.
What is the Medicare premium for 2021?
In 2021, the standard Medicare Part B monthly premium is $148.50. Beneficiaries also have a $203 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What does it mean to be dually eligible for Medicare?
If you're dually eligible, it means you have both Medicare and Medicaid.
Can you enroll in Medicare Advantage if you have Medicaid?
This means anyone with Medicaid or other forms of assistance that pay the Part B premium cannot enroll in one of these Medicare Advantage plans.
Does Medicare give back Medicare?
The Medicare giveback benefit, or Part B premium reduction plan, is becoming more available and popular among beneficiaries. Medicaid also offers programs that pay your Part B premium if you meet certain qualifications, and some retiree health plans may offer reimbursement benefits.
Do retirees get Medicare Part B?
However, for most plans you must be a retired employee or already enrolled in the health plan and be enrolled in Medicare Part B.
Why would Medicare allow additional Part B payments?
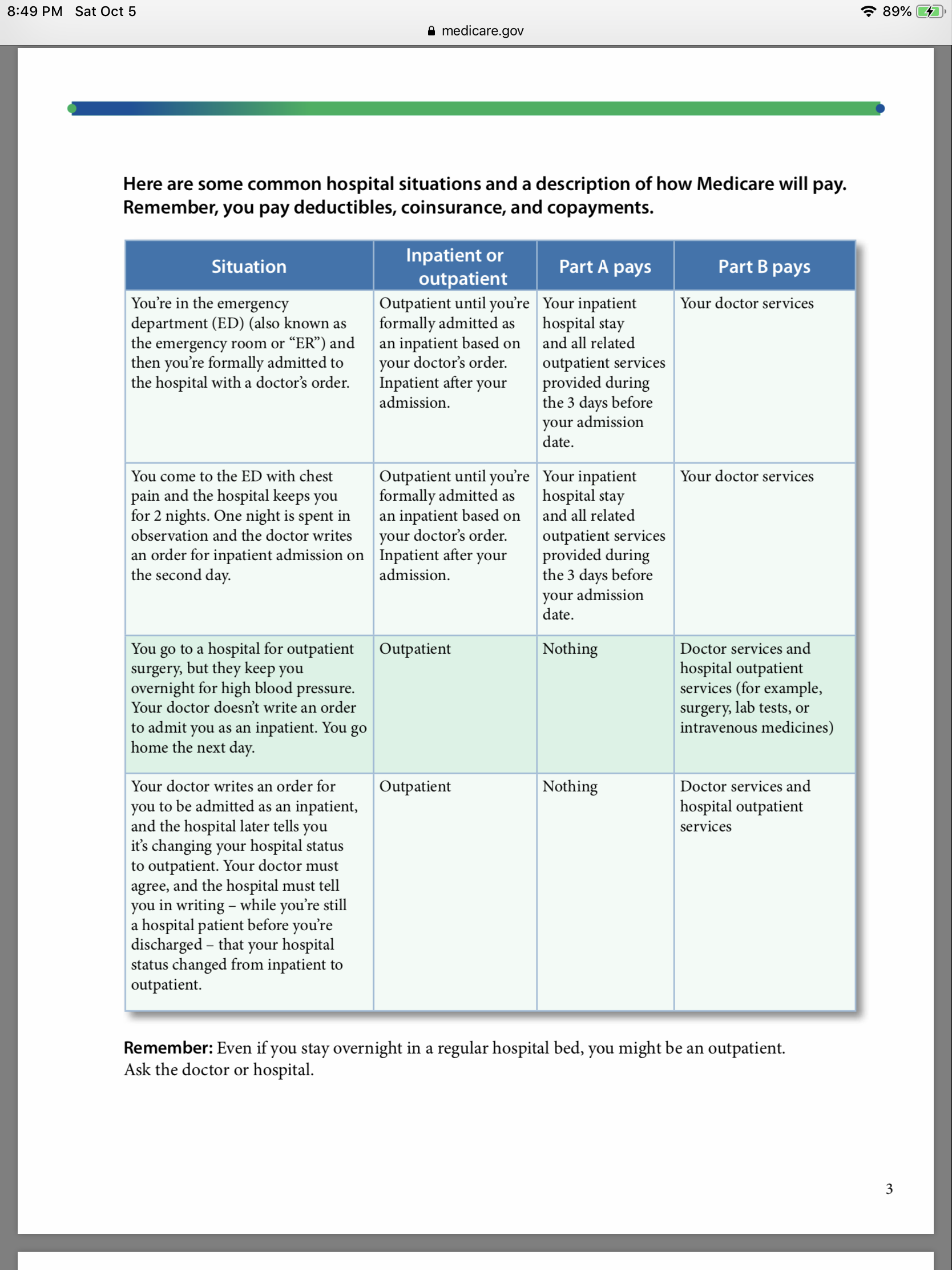
Specifically, the proposed rule would allow additional Part B payment when a Medicare Part A claim is denied because the beneficiary should have been treated as an outpatient, rather than being admitted to the hospital as an inpatient. The proposed rule, Medicare Program; Part B Inpatient Billing in Hospitals, proposes that if ...
When Part A payment cannot be made for a hospital inpatient claim?
When Part A payment cannot be made for a hospital inpatient claim because the beneficiary has exhausted his or her Part A benefits or is not entitled to Part A, Medicare’s current policy pays for the limited set of ancillary inpatient services under Part B, subject to the timely filing restriction. The proposed rule would not change this policy.
What is the reasonable and necessary standard for Medicare?
The “reasonable and necessary” standard is a prerequisite for Medicare coverage in the Social Security Act. The statutory timely filing deadline, under which claims must be filed within 12 months of the date of service, would continue to apply to the Part B inpatient claims. Also on March 13, CMS Acting Administrator Marilyn Tavenner issued an ...
When Medicare denies a claim, does it accept a new claim?
When the Medicare review contractor denies a Part A claim because a hospital inpatient admission is not reasonable and necessary, Medicare would accept new, timely filed Part B inpatient claims and provide payment for all reasonable and necessary Part B inpatient services, except those that by statute, Medicare definition, or coding definition specifically require an outpatient status (such as observation services).
How long after the date of service can you file a Part B claim?
These claims would be denied for payment if filed more than 12 months after the date of service.
How long after the date of service can a hospital bill?
Also under current policy, the hospital may only bill for the limited list of Part B inpatient ancillary services and those services must be billed no later than 12 months after the date of service.
Does Medicare pay for inpatient services?
Under longstanding Medicare policy, Medicare only pays for a limited number of ancillary medical and other health services as inpatient services under Part B when a Part A claim submitted by a hospital for payment of an inpatient admission is denied as not reasonable and necessary. Hospitals have expressed concern about Medicare’s policy, arguing that all Part B hospital services provided should be billable to Medicare because they would have been reasonable and necessary if the beneficiary had been treated as an outpatient and not as an inpatient.
When will Medicare change to MPFS?
On December 27, the Consolidated Appropriations Act, 2021 modified the Calendar Year (CY) 2021 Medicare Physician Fee Schedule (MPFS):
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When will CMS issue a correction notice for 2021?
On January 19, 2021, CMS issued a correction notice to the Calendar Year 2021 PFS Final Rule published on December 28, 2020, and a subsequent correcting amendment on February 16, 2021. On March 18, 2021, CMS issued an additional correction notice to the Calendar Year 2021 PFS Final Rule. These notices can be viewed at the following link:
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
When will CMS accept comments on the proposed rule?
CMS will accept comments on the proposed rule until September 13, 2021, and will respond to comments in a final rule. The proposed rule can be downloaded from the Federal Register at: ...
Does CMS process claims?
CMS is ready to process claims correctly and on time. You don’t need to wait to submit your claims.
How is Medicare Part B reimbursement conducted?
Reimbursement for Medicare Part B is conducted through a series of codes that number in the thousands and are updated quarterly. It is, then, important for long term care facility owners and administrators to understand how Medicare Part B works and what can be billed through it. For an overview of the process by which Medicare Part B is used in nursing homes, watch this interview between Jason Long, CEO of Experience Care, and Sue Friesth, Experience Care’s financial product manager:
What is Medicare Part B?
Medicare Part B, like the other three branches of Medicare, is billed through a system of thousands of codes in the Healthcare Common Procedure Coding System (HCPCS), more specifically HCPCS Level II. These are medical codes used for claims related to items and services like devices, supplies, medications, and transportation.
How much is Medicare Part B 2021?
The people receiving care will first have to elect Medicare Part B coverage, which requires them to pay a premium. For 2021, this amount is $148.50 for those making $88,000 or less. There is also a deductible, which is $203 for 2021, that must be paid, either by the patient/resident or a co-insurer. The deductible can be paid to any provider of Medicare Part B services. In other words, prior to entering a facility, a senior may have already met his or her deductible elsewhere and will, thus, not have to pay it at the facility. Once that deductible is met, one will be covered by Medicare.
How much does Medicare charge for therapy?
In other words, the entire fee schedule amount, the gross price, for therapy services must be documented. For instance, your facility may charge $75 for therapy evaluation, regardless of whether it is charged to Medicare or a private payer. Medicare Part B, meanwhile, might have $69 as its fee schedule amount for that service, meaning, you cannot charge more than that. What you should not do is charge 80% of the $69, or, $55.20, because that will result in only receiving 80% of what you charge, or, $44.16. Instead, you bill the entire $69 or $75 and then end up receiving $55.20 in reimbursement.
How to apply for Medicare if you are not enrolled in Medicare?
Those who are not enrolled in Medicare Part A must first do so. They can apply online here. Those unsure whether or not they have Part A can look on their red, white, and blue Medicare card, which will show “Hospital (Part A)” on the lower-left corner. Alternatively, they can call their local Social Security office or call Social Security at 1-800-772-1213.
What are the services required for a resident?
Required inpatient services – A resident must need or a doctor must order care related to the skills of professional personnel like registered nurses, licensed practical nurses, physical therapists, occupational therapists, speech-language pathologists, and audiologists.
Does Medicare reimburse for 80% of coinsurance?
It is important that long term care providers do not write off the coinsurance amount, as this will lead to Medicare treating the amount reported as the total amount, meaning, Medicare will only reimburse the facility for 80% of the 80% being reported. Medicare will then expect another payer to account for the remaining 20%, when, in reality, that 20% has not been reported.
What is Medicare Part B reimbursement?
Medicare Part B Reimbursement of Drugs prior to the Medicare Modernization Act. The Medicare Part B drug payment system is used by Medicare to reimburse health care providers for the average costs of the drugs they administer when providing outpatient services to Medicare beneficiaries.
What is ASP in Medicare?
By law, a drug's ASP is defined as the volume-weighted average manufacturer sales price net of all rebates, discounts, and other price concessions to U.S. purchasers, excluding sales that are exempt from Medicaid "best price" calculations and sales to other federal purchasers. 11 Manufacturers are required to provide CMS with the quarterly sales price and volume of sales for each covered drug by National Drug Code (NDC) within 30 days of the end of the quarter. Because multiple manufacturers may produce the same drug, CMS crosswalks NDCs for the same drug using the Healthcare Common Procedure Coding System (HCPCS). CMS then calculates a volume-weighted ASP for each HCPCS code, which becomes the basis for the reimbursement rate for the following quarter. Given the time needed to submit and process sales data, the current reimbursement rate always reflects a drug's ASP from two quarters prior. Figure 1 shows the timeline for establishing Medicare Part B reimbursement rates.
What are the direct impacts of the Medicare Modernization Act?
Following the MMA changes to the Medicare Part B drug payment system, MedPAC issued two Congressionally-mandated reports, which found that health care providers could still purchase most covered drugs at prices below the Medicare Part B reimbursement rate. 15, 16.
What is separately payable drug?
10 42 C.F.R. § 419 as amended. Separately payable drugs are those that are not packaged within an ambulatory payment classification group because their average cost per day of treatment exceeds $80. The Medicare Hospital Outpatient Prospective Payment System (OPPS) has typically reimbursed these drugs at ASP plus a 4 to 6 percent margin.
Does Medicare have power to pay for drug prices?
Under this acquisition process, Medicare has no price-setting power reimbursement rates lag rather than lead market prices. Empirical analysis of quarterly ASPs and reimbursement rates for covered drugs shows that market prices vary considerably over time and occasionally experience sharp spikes. In general, however, previous studies have found that most providers could still purchase most covered drugs at or below the reimbursement rate.
Does Medicare Part B have future prices?
Medicare Part B reimbursement rates do not establish future prices - they are based on prices previously obtained in the market. Thus, shortages (or surpluses) of a given drug will lead to price increases (or decreases), just as had been the case before the MMA.
Do insurers reimburse for drugs?
Unlike the many other medical supplies that providers routinely buy in the private market, insurers often separately reimburse providers for the cost of these drugs, rather than expecting providers to cover these costs as part of their global reimbursement. The prices of the drugs themselves, however, are not subject to price regulation ...

Important Terminology
Billed Amount vs. Approved Amount
Assignment
- One of the keys to understanding Medicare Part B reimbursement is “assignment,” which can be confusing for those not familiar with medical insurance terminology. Medicare’s definition of an assignment is “an agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any mor…
What If The Doctor Or Supplier Does Not Accept assignment?
- This does not mean you cannot seek treatment from them. It also doesn’t mean the service or item will be denied by Medicare. These are both common misconceptions. However, there are some distinct disadvantages to using non-participating providers: 1. You may have to pay the entire charge for the service or item at the time of service. 2. You will usually end up paying mor…
How Are Medicare Part B Claims paid?
- All Medicare Part B claims are processed by contracted insurance providers divided by region of the country. The current term for these providers is “Medicare administrative contractors” (MACS). Providers file your Part B claim to one of the MACS and it is from them that you will receive a notice of how the claim was processed. The statement you wi...
Medicare Supplemental Insurance
- While not strictly a part of Medicare, “Medigap” plans are worth a brief mention. They are sold by private insurers in every state, and their main function is to pick up the 20 percent Medicare coinsurance. More extensive information on them is available on the Medicare website at this tab.
Filing An Appeal
- An appeal is an action you can take if you disagree with the way your claim was processed. If you believe a service or item was denied in error, or you disagree with the amount of payment, you have the right to appeal. You may also appeal if Medicare stops paying for an item or service that you are currently receiving and believe you still need. If you decide toappeal Medicare’s decision…