If surgery is medically necessary, you’ll have coverage. Many surgeries are elective, while some require prior authorization. Medicare Part A and Part B pay for 80% of the bill. To avoid paying the 20%, you can buy a Medicare Supplement plan.
Is surgery covered by Medicare?
Surgery is one of several treatments covered under Medicare. A procedure must be considered medically necessary to qualify for coverage. This means the surgery diagnoses or treats an illness, injury, condition, disease or its symptoms. To keep your costs low, make sure the doctor performing your surgery accepts Medicare assignment.
How much of your surgery will health insurance cover?
The good news is that most health insurance plans cover a significant portion of surgical costs for procedures that are deemed medically necessary, such as surgery to save your life, improve your health, or prevent illness. This can range from an appendectomy to a heart bypass, but it can also include procedures like rhinoplasty (nose surgery ...
What surgeries does Medicare cover?
Traditional or Original Medicare covers medically necessary surgeries, including any operations that will save your life. Your Original Medicare coverage also pays for surgeries that improve your health and quality of life. Medicare covers emergency surgeries. For example, if you need immediate surgery for a life-threatening condition.
How to pay for surgery costs without insurance?
These may include:
- Bleeding and clotting studies
- Cardiac evaluation
- CBC (complete blood count) / SMA-7 (a blood metabolic panel)
- Schirmer’s test (dry eye test)
Does Medicare cover hospital operations?
Generally, Medicare covers services (like lab tests, surgeries, and doctor visits) and supplies (like wheelchairs and walkers) that Medicare considers “medically necessary” to treat a disease or condition.
Does Medicare have to approve surgery?
Your doctor must consider the surgical procedure “medically necessary.” The doctor(s) performing the surgery must accept Medicare assignment (that is, the doctor agrees to accept the Medicare-approved amount for the service, and not bill you besides a copayment or coinsurance amount).
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
How does Medicare decide how much to pay?
The Centers for Medicare and Medicaid Services (CMS) determines the final relative value unit (RVU) for each code, which is then multiplied by the annual conversion factor (a dollar amount) to yield the national average fee. Rates are adjusted according to geographic indices based on provider locality.
What is the maximum out-of-pocket expense with Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
How long does it take Medicare to approve a surgery?
Medicare takes approximately 30 days to process each claim.
How many days will Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
Does Medicare pay for everything?
Original Medicare (Parts A & B) covers many medical and hospital services. But it doesn't cover everything.
What procedures are not covered by Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
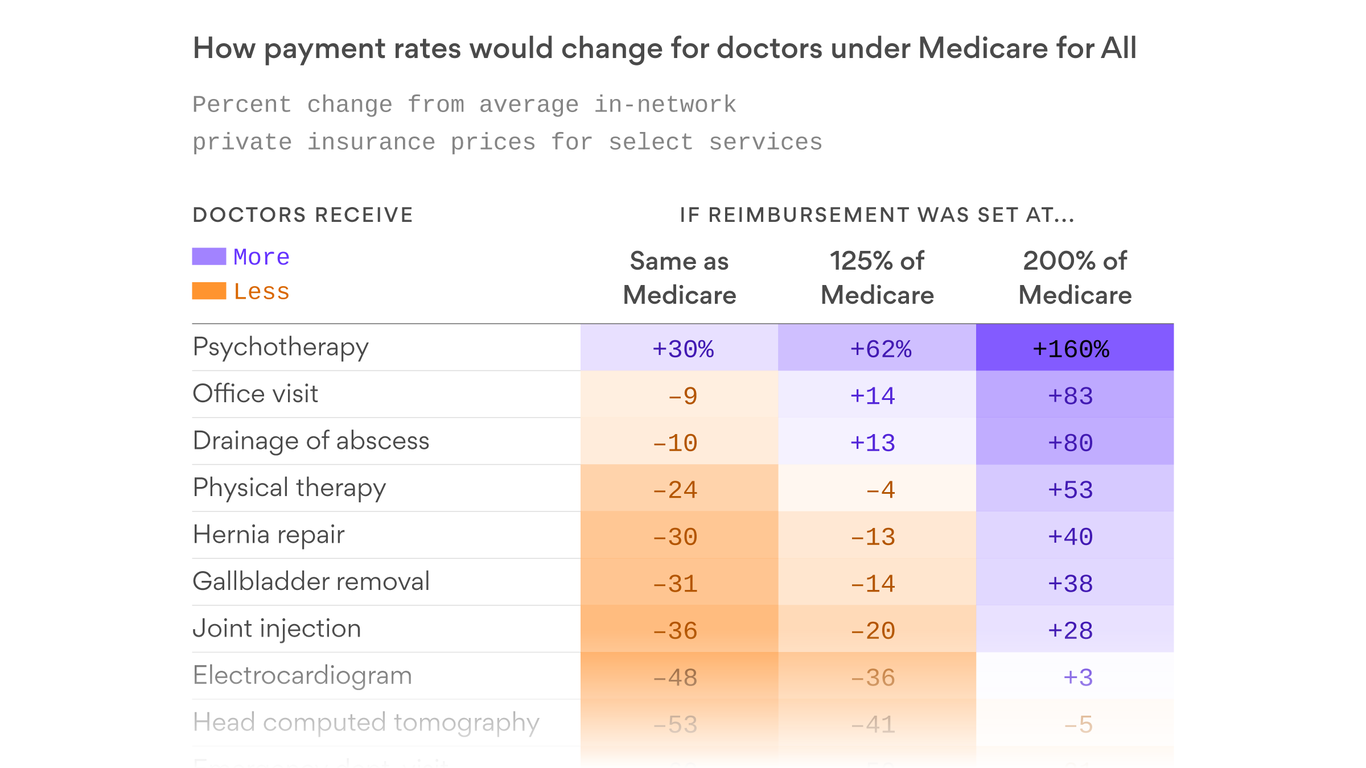
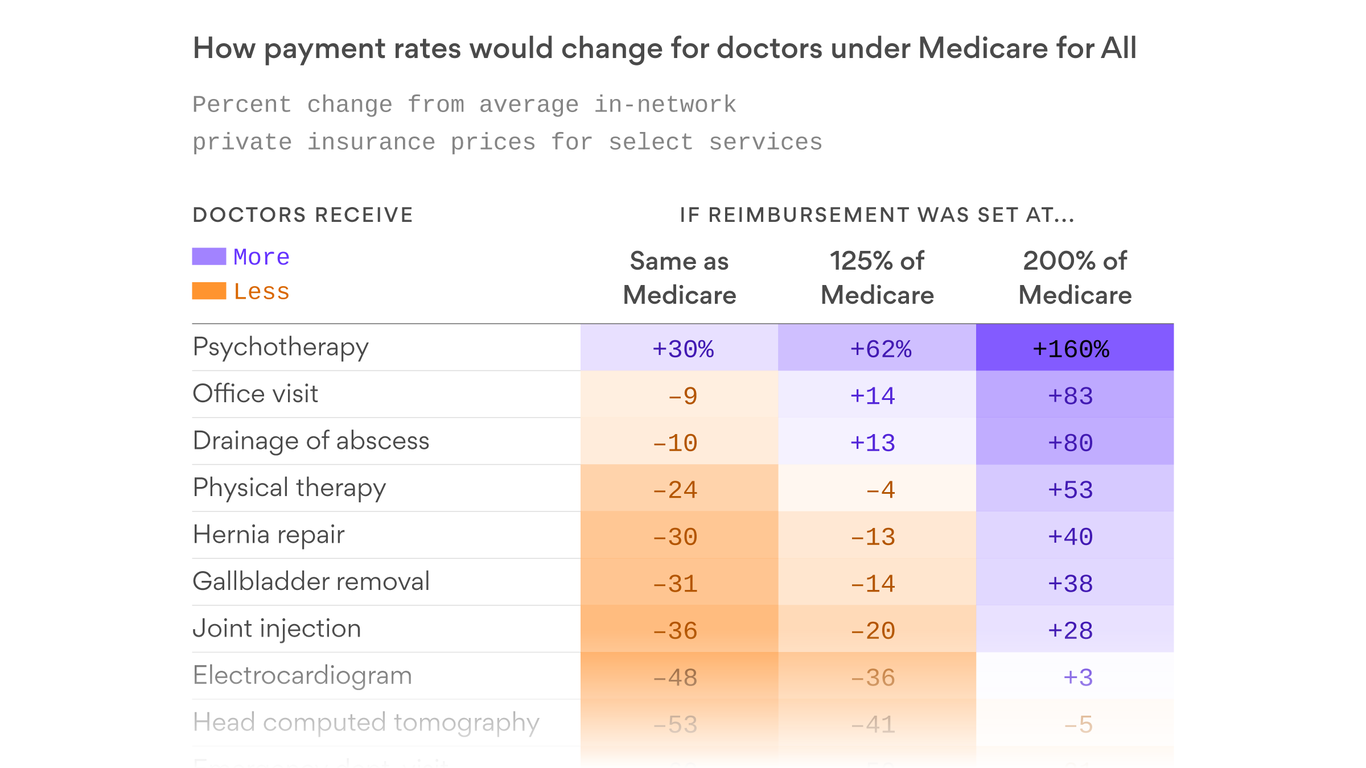
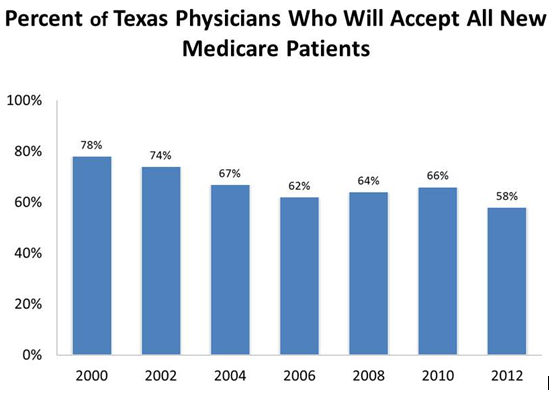
Does Medicare pay doctors less?
Fee reductions by specialty Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What Does Medicare pay for doctors visits?
If you see a GP Medicare will pay 100% of the cost if the GP bulk bills. If they don't bulk bill, Medicare will pay 100% of the public rate and you will have to pay any extra if the doctor charges more.
Is Medicare profitable for hospitals?
While the average hospital profit margin on Medicare patients has been relatively steady at negative 10%, it is closer to negative 18% for the three-quarters of hospitals that lost money on their Medicare business.
How much does Medicare pay for surgery?
After you meet your Part B deductible, Medicare will typically pay for 80% of the approved amount for medical services. This means that you will likely be responsible for 20% of the costs associated with your surgery.
How much is Medicare Part A coinsurance for 2021?
If your surgery involves a hospital visit longer than 60 days, then you will be responsible for a $371 coinsurance payment per day after day 60 in 2021. The Medicare Part A coinsurance rises to $742 per day for inpatient hospital stays of 91 days or more until your lifetime reserve day limit is reached. Medicare Part B.
What is the deductible for Medicare Part A 2021?
The deductible for Medicare Part A in 2021 is $1,484 for each benefit period. If your surgery involves a hospital visit longer than 60 days, then you will be responsible for a $371 coinsurance payment per day ...
Does Medicare cover cosmetic surgery?
Medicare does not cover cosmetic surgery of any kind, unless it is deemed necessary by a doctor. For any surgery that Medicare does cover, Medicare beneficiaries must first meet their Part A and/or Part B deductible before Medicare benefits kick in.
Does Medicare Supplement Insurance cover surgery?
A Medigap plan could help you cover some of the costs associated with your surgery, which can add up quickly.
How much does Medicare pay for surgery?
Medicare Part B will usually pay 80 percent of your eligible bills, leaving you to pay the remaining 20 percent , according to the Medicare website. If you have Medicare Supplement Insurance (Medigap), this policy may also cover some expenses related to your surgery.
How much does Medicare pay for a 90 day hospital stay?
If your hospital stay exceeds 90 days, you’ll pay $742 for every “lifetime reserve” day you spend in hospital. If you are still in hospital after exhausting your “lifetime reserve days,” Medicare Part A will no longer cover your expenses. This might sound scary, but such long hospital stays are far from the norm.
How much is Medicare deductible for 2021?
If you haven’t paid your deductible yet, add this amount to your expected expenses. In 2021, Medicare lists the annual deductible for Part A at $1,484 and for Part B at $148.50. Make sure your doctor or medical provider accepts assignment of the Medicare charges.
How long can you stay in the hospital after surgery?
That doesn’t mean people needing surgery don’t stay in the hospital longer than 60 days, but the number of people who do is very rare. Medicare Part B covers doctor services, including those related to surgery, some kinds of oral surgery, and other care you’ll receive as an outpatient.
How much is coinsurance for a hospital stay?
If your hospital stay extends beyond 60 days, days 61 to 90 will cost you (2021) $371 per day in coinsurance.
Is Medicare a good option for surgery?
Facing a surgery is scary enough without worrying about your finances. Medicare is there to help reduce your surgery bills and stress levels. Read on to get a better idea of your out-of-pocket surgery costs.
Does Medicare cover eye lifts?
For example, Medicare will cover an eye lift if the droopy lids impact vision. Medicare Part A covers expenses related to your hospital stay as an inpatient. The amount you’ll pay depends on your recovery time. You won’t incur any coinsurance if your inpatient stay lasts between one and 60 days.
Does Part B cover dental anesthesia?
Part B covers most anesthesia. But, only sometimes is dental anesthesia covered, such as when the patient has jaw cancer or a broken jaw. Parts A and B don’t cover most dental costs, so, a dental plan can help you.
Is bariatric surgery covered by the FDA?
Weight loss surgery, such as bariatric surgery, can be the answer for the morbidly obese. Luckily, certain FDA-approved weight-loss surgeries have coverage. However, the surgeries get approval or denial on a case-by-case basis.
Does Medicare cover plastic surgery?
But, Medicare covers a portion of costs for plastic surgery if it’s necessary. Examples of this are reconstruction surgery after an accident or severe burns.
What is the procedure that Medicare requires prior authorization for?
Medicare requires prior authorization before you get these hospital outpatient services that are sometimes considered cosmetic: Blepharoplasty – Surgery on your eyelid to remove “droopy,” fatty, or excess tissue. Botulinum toxin injections (or “Botox”) – Injections used to treat muscle disorders, like spasms and twitches.
Do you need prior authorization for Medicare?
If your procedure requires prior authorization before Medicare will pay for it, you don’t need to do anything. Your provider will send a prior authorization request and documentation to Medicare for approval before performing the procedure.
Does Medicare cover breast reconstruction?
Medicare usually doesn’t cover cosmetic surgery unless you need it because of accidental injury or to improve the function of a malformed body part. Medicare covers breast prostheses for breast reconstruction if you had a mastectomy because of breast cancer.
What is the SGR for Medicare?
Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending. For more than a decade this formula has called for cuts in physician payments, reaching as high as 24 percent.
Does Medicare have a fee for service?
Current payment systems in traditional Medicare have evolved over the last several decades, but have maintained a fee-for-service payment structure for most types of providers. In many cases, private insurers have modeled their payment systems on traditional Medicare, including those used for hospitals and physicians.
Does Medicare use prospective payment systems?
Medicare uses prospective payment systems for most of its providers in traditional Medicare. In general, these systems require that Medicare pre-determine a base payment rate for a given unit of service (e.g., a hospital stay, an episode of care, a particular service).
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. if you expect to be admitted to the hospital. Check your Part B deductible for a doctor's visit and other outpatient care.
Does Medicare cover bariatric surgery?
Bariatric surgery. Medicare covers some bariatric surgical procedures, like gastric bypass surgery and laparoscopic banding surgery, when you meet certain conditions related to morbid obesity.
What is a flat fee for a medical group?
When a doctor, medical group, hospital or integrated health system receives a certain flat fee every month for taking care of an individual enrolled in a managed health care plan, regardless of the cost of that individual’s care.
What is pay for performance?
A pay-for-performance model where the physician’s training, skills and time expended to provide a given service are taken into account when establishing compensation. With this model, the actual care provided by the physician is the driving force of compensation more so than the number of visits.
What is concierge medicine?
An alternative to traditional payment models, where medical practices have a direct financial relationship with patients. They typically charge a monthly or annual fee so that the patient receives additional access and personalized care. These practices are known by a variety of names: concierge healthcare, direct primary care, direct care, direct practice medicine, retainer-based, membership medicine, cash-only medicine, cash-only practice, boutique medicine, personalized healthcare.
Do surgeons get a single payment?
Many surgeons will often receive a single payment for pre-op, post-op and the surgery. However, bundled payments can also be much broader, encompassing longer periods of time and multiple providers. With bundled payments, there are four models: – Retrospective Acute Care Hospital Stay Only.