How do I appeal the denial of a Medicare claim?
Filing an initial appeal for Medicare Part A or B: File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think …
What if Medicare denies my claim?
You should only need to file a claim in very rare cases. Check the status of a claim. Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan. File an appeal
How do I file an appeal?
Jan 11, 2022 · The initial judgment may be appealed in one of the following ways: Completing a Redetermination Request Form and submitting it to the contractor assigned to your case on the MSN Adhere to the appeals guidelines as specified on the MSN. You may choose to consult your physician or healthcare... Making ...
When can I file an appeal to a Medicare claim?
May 25, 2021 · Requesting Reconsideration (Appeal Level 2) 1. Fill out a request form. You can request reconsideration by filling out a “Medicare Reconsideration Request Form” and... 2. Write a letter. If you do not want to use the form, you can write a …
How do I appeal a Medicare rejection?
If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
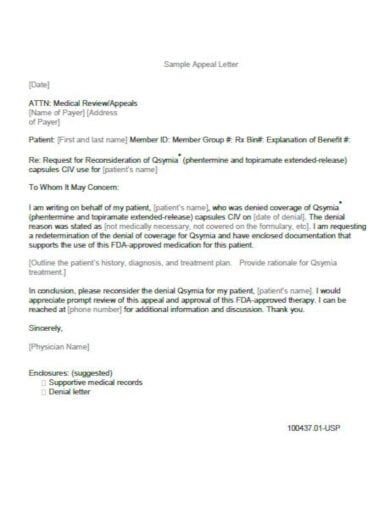
How do I write a Medicare appeal letter?
Submit a written request that must include: Your name, address, phone number, and Medicare Number. If you've appointed a representative, include their name, address, and phone number. The appeal number included on the “QIC reconsideration decision,” if any.
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
How do you win a Medicare appeal?
To increase your chance of success, you may want to try the following tips: Read denial letters carefully. Every denial letter should explain the reasons Medicare or an appeals board has denied your claim. If you don't understand the letter or the reasons, call 800-MEDICARE (800-633-4227) and ask for an explanation.Nov 12, 2020
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
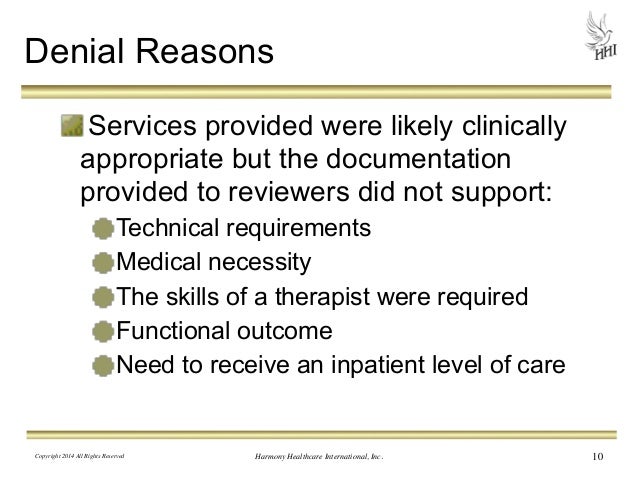
Why would Medicare deny a claim?
Medicare may issue denial letters for various reasons. Example of these reasons include: You received services that your plan doesn't consider medically necessary. You have a Medicare Advantage (Part C) plan, and you went outside the provider network to receive care.May 18, 2020
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.Jul 11, 2018
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
What is a Medicare administrative contractor?
A Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B (A/B) medical claims or Durable Medical Equipment (DME) claims for Medicare Fee-For-Service (FFS) beneficiaries.Jan 12, 2022
What is a Livanta appeal?
Livanta is here to protect your rights. If you are a Medicare recipient, Livanta can help you: Get immediate help in resolving a healthcare concern. Appeal a notice that you will be discharged from the hospital or that other types of services will be discontinued.
What is a 2nd level appeal?
Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Any party to the redetermination that is dissatisfied with the decision may request a reconsideration.Apr 4, 2022
Are Social Security Offices affected by Coronavirus (COVID-19)?
All local Social Security offices will be closed to the public for in-person service starting Tuesday, March 17, 2020.
How do I apply for Social Security disability benefits?
Social Security offers an online online disability application. Contact your local Social Security office.
How do I change or correct my name on my Social Security card?
There is no charge for a Social Security card. This service is free. The same applies once you receive the I-766 card, Employment Authorization Doc...
How do I get a new or replacement Social Security Card?
If your Social Security card is lost or stolen you can replace it through the Social Security Administration (SSA) website www.ssa.gov , or by v...
Can I schedule an appointment with the Social Security office?
The SSA does not have an online appointment scheduler.
How do I find out my Social Security benefits?
Sign up for your "My Social Security" account online to review your information, apply for benefits and manage your account. Visit www.ssa.gov/mya...
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
What is a denial of a request?
Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition. Denials of a request you and your doctor have made to change the price you pay for a prescription drug. For example: Your Medicare Part D drug plan rejects ...
How to request a plan exception?
Requests for plan exceptions can be made by phone or in writing if you are asking for a prescription drug you haven’t yet received. If you are asking to be reimbursed for the price of drugs you have already bought, you must make your request in writing.
Can you appeal a Part D plan?
If your life or health could be at risk by having to wait for a medication approval from your plan, you or your doctor can request an expedited appeal by phone. If you disagree with your Part D plan’s decision, you can file a formal appeal.
Can you appeal a Medicare Advantage plan?
Medicare Advantage plans, which are administered by private insurance companies, are required by Medicare to have an appeals process by which you can get a redetermination if your plan denies you a service or benefit you think should be covered. If you disagree with the decision, you can request an independent review.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How to appeal a denial of Medicare?
However, you initially need to start by talking to your doctor. Ask if there are any generic, over-the-counter medicines that you could take instead of the medication Medicare refuses to pay for.
How many levels of appeals are there for Medicare?
There are five levels of Medicare appeals for Medicare Parts A and B (original Medicare). Begin with an initial request to your plan for a redetermination. If you are unhappy with the result, then you can continue to appeal all the way up to a federal district court.
How to appoint a representative for Medicare?
You can also appoint a representative by writing a letter. Make sure the letter contains the following information: your name and contact information. your Medicare number. a statement in which you appoint someone as your representative. the name and contact information of the representative.
How long does it take to get a Medicare redetermination?
Receive your Medicare Redetermination Notice. After you submit your appeal and all supporting documentation, you will receive a decision within 60 days. You will receive a Medicare Redetermination Notice in the mail. If you disagree with the determination, you may appeal to the next level.
How to request reconsideration of Medicare?
Fill out a request form. You can request reconsideration by filling out a “Medicare Reconsideration Request Form” and mailing it to a Qualified Independent Contractor (QIC). QICs are private companies that contract with Medicare to handle appeals. They are not involved in the initial redetermination.
How long does it take to appeal an ALJ decision?
In most cases, the ALJ will mail you a written decision within 90 days. If you disagree with the ALJ’s decision, then you have 60 days to file an appeal. If the ALJ doesn’t issue a timely decision, then you can request that your case be forwarded to the Medicare Appeals Council, which is the fourth level of appeals.
What to do when appealing a prescription drug determination?
If you are appealing a prescription drug determination, then you should involve your doctor. Your doctor can make the argument that you need the drug and can also speak to how denial of the drug could harm your health.
How long does it take to appeal a Medicare claim?
For amounts of at least $1,400, the final level of appeal is judicial review in U.S. district court. Medicare Advantage and Part D. You have 60 days to initiate an appeal involving a Medicare Advantage or Part D prescription-drug plan.
How many levels of appeals are there for Medicare?
Traditional Medicare. There are five levels of claims appeals for traditional Medicare; most people have to go through several levels to get a denial overturned.
How long does it take for Medicare to redetermine a claim?
At the first level, you are given 120 days after receiving the Medicare summary notice to request a "redetermination" by a Medicare contractor—that is, the person who reviews the claim.
What is an appeal letter for health insurance?
Writing an appeal letter for your denied health insurance claim is a matter of sharing the proper information to have your case looked at as soon as possible. If you request an appeal but can't share why your claim was denied, the insurance company may find it hard to review your appeal.
What is a denial of a claim?
A health insurance claim denial is when an insurance company does not approve payment for a specific claim. In this case, the health insurer decides not to pay for a procedure, test, or prescription. A claim rejection, on the other hand, can be easy to correct.
Why is my health insurance denied?
Here are five common reasons health insurance claims are denied: There may be incomplete or missing information in the submitted claim documents or there could be medical billing errors. Your health insurance plan may not cover what you are claiming, or the procedure may not be deemed medically necessary.
Who is Mila Araujo?
Mila Araujo is a certified personal lines insurance broker and the director of personal insurance for Ogilvy Insurance. She has over 20 years of experience in the insurance industry, and as insurance expert, has written about homeowners, auto, health, and life insurance for The Balance.