How to appeal when someone with Medicare is being discharged?
If you’re getting Medicare services from a hospital, skilled nursing facility, home health agency, comprehensive outpatient rehabilitation facility, or hospice, and you think your Medicare‑covered services are ending too soon (or that you’re being discharged too soon), you can ask for a fast appeal. Your provider will give you a notice called a Notice of Medicare Non Coverage before …
What is Medicare right to appeal discharge?
May 27, 2021 · You must ask for a Medicare hospital discharge appeal no later than the day you're scheduled to be discharged. If you appeal within this time frame, you can stay in the hospital while you wait to get the BFCC-QIO's decision. You won't have to pay for your stay (except for applicable coinsurance or deductibles).
How Medicare beneficiaries can fight a hospital discharge?
Jul 04, 2016 · To implement the appeals process, the family must first inform the discharge planner that they feel the patient is being discharged prematurely and ask to file an appeal. The discharge planner cannot legally release the patient from the hospital until the process is reviewed and a decision handed down. The family must work quickly; appeals are handled …
How to review Medicare Appeals in the SNF?
How do you fight a Medicare discharge?
Can you appeal a discharge?
You may appeal if you disagree with the termination and — if the services are provided by an HHA or CORF — a doctor certifies that failure to continue the service may place your health at significant risk.
What should I say in a Medicare appeal?
- your name and address.
- your Medicare number (as shown on your Medicare card)
- the items you want Medicare to pay for and the date you received the service or item.
- the name of your representative if someone is helping you manage your claim.
Can a patient appeal a discharge from the hospital?
How do I write a Medicare appeal letter?
- Your name, address, and the Medicare Number on your Medicare card [JPG]
- The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.
How long does Medicare have to respond to an appeal?
What are the five steps in the Medicare appeals process?
How successful are Medicare appeals?
What is the first level of the Medicare appeals process?
How do you contest a hospital discharge?
Can a hospital discharge a patient without a diagnosis?
What is the latest time a hospital can discharge you?
What does a nurse say when you're discharged?
She wanted to know what her options were. Often when you're in the hospital, the nurse comes in and says, "hey, you're being discharged" without any warning.
What to do if you feel like you're being discharged too soon?
So, if you feel like you're being discharged too soon, you can file a Medicare hospital discharge appeal.
What to do if playback doesn't begin?
If playback doesn't begin shortly, try restarting your device.
Does Medicare cover SNF?
Medicare may continue to cover your SNF, HHA, CORF, or hospice services (except for applicable coinsurance or deductibles).
Do you have to pay for hospice after the end of your coverage?
You won't be responsible for paying for any SNF, HHA, CORF, or hospice services provided before the termination date. If you continue to get services after the coverage end date, you may have to pay.
Can you appeal a Medicare discharge?
You must ask for a Medicare hospital discharge appeal no later than the day you're scheduled to be discharged. If you appeal within this time frame, you can stay in the hospital while you wait to get the BFCC-QIO's decision. You won't have to pay for your stay (except for applicable coinsurance or deductibles).
Why appeal a hospital discharge?
Appealing a hospital discharge allows the patient more time to be treated in a hospital and offers the family more time to prepare for home care or to find the right rehab facility.
How long does it take to appeal a nursing home?
An appeal can be reviewed within a one- to two-day time period. So use the time wisely. If you need to research nursing home rehab centers, start making calls and touring facilities. If the patient will be returning home, use this time to prepare the apartment properly.
What is a QIO in Medicare?
Every state has at least one Medicare Quality Improvement Organization , (QIO), that will intervene when a person appeals a hospital discharge. A QIO is a private, usually not-for-profit organization that is staffed by health care professionals who are trained to review medical care and determine if a case has merit.
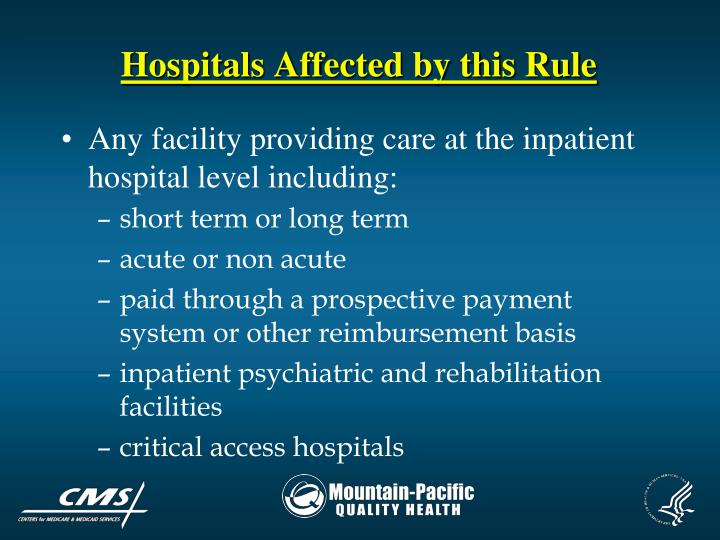
Why do hospitals have to discharge patients?
In fact this is the standard protocol for hospitals. Hospitals are under intense pressure to discharge patients as quickly as possible after they are out of immediate danger. This is due to Medicare’s payment policy. Medicare pay hospitals a predetermined fixed amount that is tied to each patient’s diagnosis.
Can a hospitalized patient appeal a discharge?
Fortunately, Medicare offers a safe recourse—any hospitalized patient covered by Medicare can appeal a hospital discharge. An even greater benefit is the patient can stay in the hospital during the appeal process and continue to be treated at no extra cost.
Can a QIO decide that a patient can be discharged safely?
The good news is, even If the QIO decides that patient can be discharged safely, the patient will not be responsible for paying the hospital charges (except for applicable coinsurance or deductibles). When a patient is first admitted to the hospital he is given a written notice titled “An Important Message from Medicare about Your Rights”. ...
What is the first level of appeal for Medicare?
Your first level of appeal is to the BFCC-QIO for the area in which you received Medicare services. You will find the name and phone number of the BFCC-QIO for your area in your IM.
What to do if discharge is too early?
If you think your hospital discharge is too early, file a fast appeal with Medicare. If you think your Medicare-covered stay in a hospital is ending too soon, you have the right to request an expedited, or "fast," appeal if you disagree with this decision.
What is a fast appeal?
The Basics of a Fast Appeal. Beneficiaries who receive services under Medicare Part A for a hospital stay may request an expedited review, also known as a "fast appeal," if the hospital decides to terminate your services or discharge you too soon. While there are five total levels of appeal, only the first two levels can be done on an "expedited" ...
What are the levels of appeal for QIC?
If you receive an unfavorable QIC reconsideration decision that says Medicare will not cover or pay for your continued stay in the hospital, you have three remaining levels of appeal: a Level 3 hearing with an administrative law judge; a Level 4 request for review from the Medicare Appeals Council (MAC); and finally, ...
How long does it take for a hospital to give you an IM?
The hospital must also give you a copy of the IM you signed within two (2) days of your scheduled discharge date. It is very important to follow the directions found in the IM; otherwise, your financial responsibility and appeal rights may be negatively affected.
How many levels of appeal are there?
While there are five total levels of appeal, only the first two levels can be done on an "expedited" basis. It is important to follow the correct procedure for a fast appeal of a discharge from a hospital, which is different from the procedures for requesting a fast appeal in a non-hospital setting, such as a skilled nursing facility (SNF), ...
How long does it take to get an IM from Medicare?
Your appeal rights are found in a notice called "An Important Message from Medicare about Your Rights," also called the "IM." You should have received a copy of the IM within two days of your hospital admission and should have been asked to sign it. Ask for the IM if you didn't get it.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How to appeal Medicare summary notice?
If you have Original Medicare, start by looking at your " Medicare Summary Notice" (MSN). You must file your appeal by the date in the MSN. If you missed the deadline for appealing, you may still file an appeal and get a decision if you can show good cause for missing the deadline.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
What is a Pace plan?
A special type of health plan that provides all the care and services covered by Medicare and Medicaid as well as additional medically necessary care and services based on your needs as determined by an interdisciplinary team. PACE serves frail older adults who need nursing home services but are capable of living in the community. PACE combines medical, social, and long-term care services and prescription drug coverage.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What happens if you file an appeal with Medicare?
After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan. If you believe you're being discharged from a hospital too soon, you have a right to immediate review by your.
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
When do you have the right to a fast track appeal?
You'll have the right to a fast-track appeals process when you disagree with a decision that you no longer need services you're getting from a skilled nursing facility, home health agency, or a comprehensive outpatient rehabilitation facility.