What are the timely filing guidelines for Medicare?
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan. File an appeal. How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
What is the timely filing limit for Medicare claims?
Mar 01, 2021 · Keep copies: Be sure to keep a copy of everything you send to your plan as part of your appeal. Start the process: Follow the directions in your plan’s initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late.
What is the deadline for filing a Medicare claim?
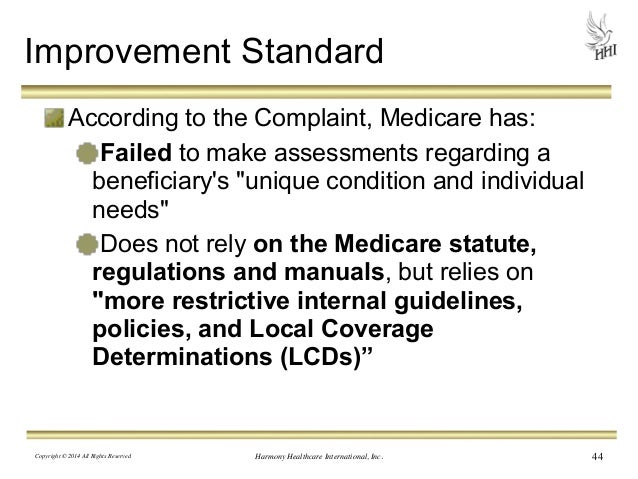
CMS Appeals and Medicare Appeals webpages. Appealing Medicare Decisions Medicare FFS has 5 appeal process levels: Level 1 - MAC. Redetermination. Level 2 - Qualified Independent Contractor (QIC) Reconsideration. Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition. Level 4 - Medicare Appeals Council (Council) Review. Level 5 -
What is proof of timely filing?
Jun 07, 2010 · Name of Insurance Company. Address (get address for appeals if it exists) Re: Appeal of Denial for Timely Filing. Patient Name: Group Number: DOS: Subscriber No: Reference No.: (etc – get this information from the denial) We are appealing the denial of claims for (patient name) and request that these claims be reviewed and paid.
How do I write a Medicare appeal letter?
What is Medicare appeal deadline?
The appellant (the individual filing the appeal) has 120 days from the date of receipt of the initial claim determination to file a redetermination request.Dec 1, 2021
What is the period of timely filing limit for Medicare?
What are the 5 levels of appeal for Medicare?
How successful are Medicare appeals?
Can I appeal Medicare premium?
How would you handle a denial for timely filing?
What is timely filing limit?
How do I correct a Medicare billing error?
How do you win a Medicare appeal?
What are Medicare appeals?
How many steps are there in the Medicare appeal process?
Sending Claims in A Timely Manner
In order to send a timely filing appeal, you have to have evidence to support your statement that the claim was sent within the timely filing deadl...
When You Get A Timely Filing Denial
Lets say that you have sent a batch of claims, checked them at the clearinghouse, and they have all gone out correctly.Unfortunately, however, some...
Sending A Timely Filing Appeal
When you send claims via your practice management system, make sure you print out your claims report, which says which claims went out on which day...
Can you appeal a denial of timely filing?
If you didn't then you have no reason for appeal, and you cannot appeal the claim.
How long does it take to get a federal appeals letter?
If you don't send your appeal to the right address, it won't be processed correctly! Most appeals take anywhere from 30 to 45 days to process, so make sure you keep a copy of the appeal for your own records and check the appeal in 30-45 days to see if it has been paid.
What happens when you send a claim through practice management system?
Typically, when you send claims through any type of practice management system, an internal report is generated. This says which claims were sent and on which day. Many of your claims will go out electronically to a claims clearinghouse, which is like a middleman between your office and the insurance company.
Can insurance claims be lost?
Unfortunately, however, some claims simply get lost. This means that even though you sent them to the right place and within the right time frame, they are lost in your electronic system and you never get a response from the insurance company.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is a redetermination in Medicare?
A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
How long does it take for a MAC to send a decision?
Generally, the MAC will send its decision (either in a letter, an RA, and/or an MSN) to all parties within 60 days of receipt of the request for redetermination. The decision will contain detailed information on further appeals rights, where applicable.
Can a MAC dismiss a request for redetermination?
A MAC may dismiss a request for a redetermination for various reasons, some of which may be: If the party (or appointed representative) requests to withdraw the appeal. The party fails to file the request within the appropriate timeframe and did not show (or the MAC did not determine) good cause for late filing.
How to appeal a health insurance claim?
Here are 4 tips to help you get started: 1 Get help: If you want help filing an appeal, contact your State Health Insurance Assistance Program (SHIP) or appoint a representative. Your representative could be a family member, friend, advocate, attorney, doctor, or someone else who will act on your behalf. 2 Gather information: Ask your doctor, other health care providers, or supplier for any information that may help your case. 3 Keep copies: Be sure to keep a copy of everything you send to your plan as part of your appeal. 4 Start the process: Follow the directions in your plan’s initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. See what information to include in your written request.
How long do you have to file a denial of health insurance?
Start the process: Follow the directions in your plan’s initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. See what information to include in your written request.
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.