Call your State Medical Assistance (Medicaid) office to see if you qualify. Individuals who qualify for both Medicare and Medicaid at the same time are called "dual" or "dual eligible." Dual Special Needs plans, or DSNPs, are designed specifically for dual-eligible people.
Full Answer
What is Medicare dual eligible and how do I qualify?
What type of coverage do you get if you are dual eligible for Medicare and Medicaid?
- Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
- Specified Low-Income Medicare Beneficiary (SLMB) Program. The SLMB program helps pay for Medicare Part B premiums.
- Qualifying Individual (QI) Program. ...
- Qualified Disabled Working Individual (QDWI) Program. ...
What does dual eligible mean in Medicare?
“Dual Eligible” is a term given to beneficiaries of both Medicare and Medicaid. In order to receive Medicare benefits, an individual must be at least 65 years of age or a recipient of Social Security Disability Insurance (SSDI) for at least 24 months.
Who is eligible for both Medicare and Medicaid?
You can also get Medicare and Medicaid if you’re under 65, have certain disabilities and have low income and asset levels. Since Medicare does not cover many types of home or nursing care considered to be custodial care, Medicaid often is the go-to source for care at home or in a nursing home. Who qualifies for dual eligible?
What is full benefit dual eligible?
dual-eligible beneficiaries: People who are jointly enrolled in Medicare and Medicaid and who are eligible to receive benefits from both programs. All dual-eligible beneficiaries qualify for full Medicare benefits, which cover their acute and postacute care.
When can a patient have both Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
Can you qualify for both Medicare and Medical?
If you qualify for full Medi-Cal (Medi-Cal without a share of cost (SOC)), Medi-Cal will also cover your Medicare Part A and B deductibles and copayments, and pay your monthly Medicare Part B premium. Learn more. If you have both Medicare and Medi-Cal, how you receive your benefits depends on the county you live in.
What plan provides both Medicare and Medicaid coverage?
UnitedHealthcare Connected® for One Care (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
What does it mean if a Medicare patient is dual eligible?
Dual-eligible beneficiaries are individuals who receive both Medicare and Medicaid benefits. The two programs cover many of the same services, but Medicare pays first for the Medicare-covered services that are also covered by Medicaid.
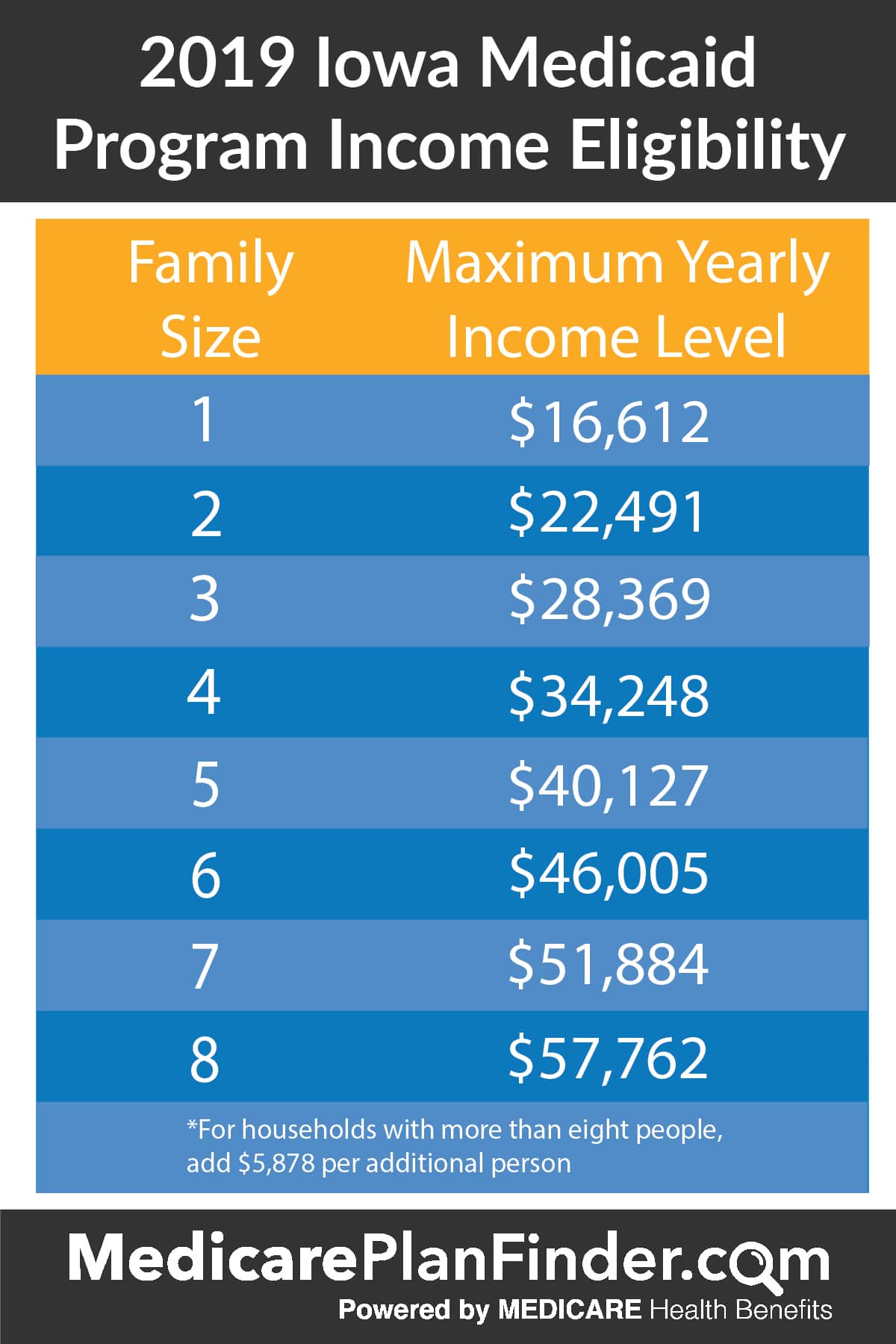
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Can you have Medicare and Medicaid?
Medicaid is a state and federal program that provides health coverage if you have a very low income. If you are eligible for both Medicare and Medicaid (dually eligible), you can have both. They will work together to provide you with health coverage and lower your costs.
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
How do I qualify for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
Does Medicaid pay Medicare premiums?
Medicaid pays Part A (if any) and Part B premiums. Medicaid is liable for Medicare deductibles, coinsurance, and copayments for Medicare-covered items and services. Even if Medicaid doesn't fully cover these charges, the QMB isn't liable for them.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is a dual complete plan?
A UnitedHealthcare Dual Complete plan is a DSNP that provides health benefits for people who are “dually-eligible,” meaning they qualify for both Medicare and Medicaid. Who qualifies? Anyone who meets the eligibility criteria for both Medicare and Medicaid is qualified to enroll in a DSNP.
How many Americans are dual eligible?
12.2 millionKey facts: There were 12.2 million dually eligible beneficiaries enrolled in both programs in calendar year 2019.
What is dual eligibility?
You’re also considered a dual eligible beneficiary if you’re enrolled in Medicare Part A or Part B and receiving cost-sharing through a Medicare savings program (MSP). Below is table summarizing the benefits and eligibility criteria for each of the different MSPs in 2021: MSP. Benefits.
What is the difference between Medicare and Medicaid?
Takeaway. Medicare is the federal health insurance program in the United States for people age 65 and older. Medicaid is a joint federal and state program to help people with limited resources or income pay for medical costs.
How many people are on Medicare and Medicaid?
According to Health Affairs, about 9.2 million people, representing about 16 percent of Medicare enrollees and about 15 percent of Medicaid enrollees, are enrolled in both Medicare and Medicaid. Keep reading to learn more about dual eligibility, benefits, and state-by-state differences.
What is fee for service Medicaid?
fee-for-service Medicaid coverage. plans that include all Medicare and Medicaid benefits. Income and resource standards are defined by federal law for full Medicaid and the Medicare Savings Programs. At their discretion, states can effectively raise the federally mandated limits.
Is Medicare a dual beneficiary?
If you’re eligible for both Medicare and Medicaid, you’re considered a dual eligible beneficiary. Dual eligibility is typically determined by your age, any disabilities, and income.
Is Medicare free for older people?
It also covers people with certain disabilities and health conditions. Medicare is not free coverage — you’ll still pay deductibles, premiums, and copays for medical services.
Is dual eligibility covered by insurance?
If you’re a dual eligibility beneficiary, it’s likely that most of your healthcare costs are covered. The information on this website may assist you in making personal decisions about insurance, but it is not intended to provide advice regarding the purchase or use of any insurance or insurance products.
What is dual eligible?
Full dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income (SSI) benefits, which provide cash assistance for basic food ...
What is partial dual eligibility?
Partial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
What is the Medicare and Medicaid program?
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly. PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities. Some of the things that can be covered by PACE include: Adult day primary care. Dental care.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What is a dual SNP?
If you are Medicare dual eligible, you may qualify for a Medicare D-SNP (Dual Special Needs Plan), which is a type of Medicare Advantage plan. 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2.
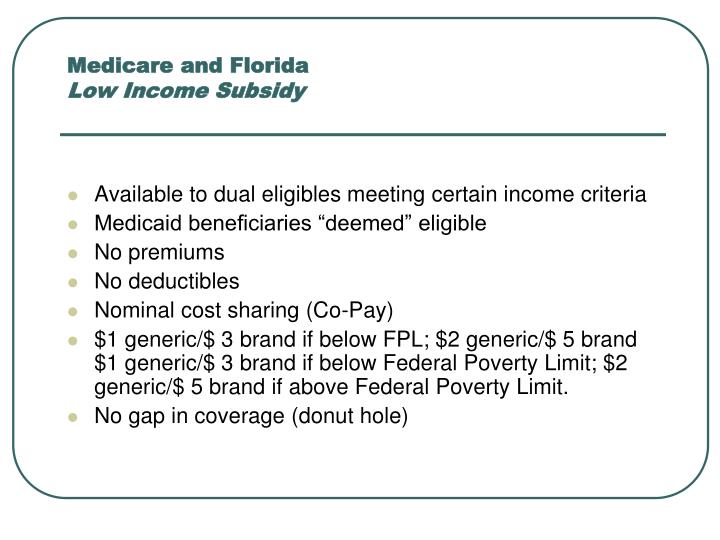
What is an annual special enrollment period?
An annual Special Enrollment Period to enroll in a Part D plan or switch to a new one. Elimination of Part D late enrollment penalties. You automatically qualify for Extra Help if you are enrolled in Medicaid, Supplemental Security Income or a Medicare Savings Program.
What is dual eligible for medicaid?
Qualifications for Medicaid vary by state, but, generally, people who qualify for full dual eligible coverage are recipients of Supplemental Security Income (SSI). The SSI program provides cash assistance to people who are aged, blind, or disabled to help them meet basic food and housing needs.
What is dual eligible?
The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”.
What is Medicare Advantage?
Medicare Advantage plans are private insurance health plans that provide all Part A and Part B services. Many also offer prescription drug coverage and other supplemental benefits. Similar to how Medicaid works with Original Medicare, Medicaid wraps around the services provided by the Medicare Advantage plan andserves as a payer of last resort.
What is Medicaid managed care?
Medicaid managed care is similar to Medicare Advantage, in that states contract with private insurance health plans to manage and deliver the care. In some states, the Medicaid managed care plan is responsible for coordinating the Medicare and Medicaid services and payments.
When will Medicare become the main health insurance?
July 08, 2020. Most Americans understand that when they turn 65, Medicare will become their main health insurance plan. However, many Americans are less familiar with another health care program, Medicaid, and what it means if they are eligible for both Medicare and Medicaid. If you are dual eligible, Medicaid may pay for your Medicare ...
Does Medicare cover Part A and Part B?
Some Medicare beneficiaries may choose to receive their services through the Original Medicare Program. In this case, they receive the Part A and Part B services directly through a plan administered by the federal government, which pays providers on a fee-for-service (FFS) basis. In this case, Medicaid would “wrap around” Medicare coverage by paying for services not covered by Medicare or by covering premium and cost-sharing payments, depending on whether the beneficiary is a full or partial dual eligible.
Is Medicaid a payer of last resort?
Medicaid is known as the “payer of last resort.”. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
What Is Medicare?
Medicare is a federal health insurance program for older people (65 and over), younger people with disabilities, and individuals who have ESRD (End-Stage Renal Disease).
What Is Medicaid?
Medicaid is a federal government and state health care program for low-income individuals of any age in the U.S. This health insurance offers affordable health care options to people who can't afford to pay for medical items, services, and treatments.
What Is Dual Eligibility?
There are a variety of reasons why people may struggle to cover the costs of Medicare insurance.
Who Can Apply for Dual Eligibility?
To qualify for dual eligibility, you need to meet the enrollment criteria for both the Medicare and Medicaid program.
Part A and B Financial Help
Once you're dual eligible, you’ll be able to use your Medicaid to pay some or all of your Original Medicare premiums and health care costs.
Dual-Eligible Benefit Types
There are six types of dual-eligible beneficiaries. Each one has its own financial requirements to enroll and offers other relief from Medicare health care costs.
Dual Eligible and Medicare Advantage
Certain dual eligibles are still allowed to enroll for Medicare Advantage plans. These are called Special Needs Plans (SNPs) and are designed to cater to dual eligibles and other specific groups.
