If you are enrolled in Medicare Part A and you want to enroll in Part B, please complete form CMS-40B, Application for Enrollment in Medicare – Part B (medical insurance). If you are applying for Medicare Part B due to a loss of employment or group health coverage, you will also need to complete form CMS-L564, Request for Employment Information.
Full Answer
When do I have to apply for Medicare Part B?
Feb 11, 2022 · To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Persons might find it helpful to learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Do you really need Medicare Part B?
Jan 01, 2022 · I have Part A & want to add Part B. Contact Social Security to sign up for Part B: Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). Send the completed form to your local Social Security office by fax or mail. Call 1-800-772-1213. TTY users can call 1-800-325-0778. Contact your local Social Security office.
When should I sign up for Medicare?
To be eligible for premium Part A, an individual must be age 65 or older and be enrolled in Part B. Enrollment in premium Part A and Part B can only happen at certain times. (The section titled Enrollment Periods and When Coverage Begins explains the times when someone can enroll).
What are the requirements to apply for Medicare?
Nov 24, 2021 · Views: 95933. If you are already enrolled in Medicare Part A and you would like to enroll in Part B under the Special Enrollment Period (SEP), you can apply online at Apply for Medicare Part B Online during a Special Enrollment Period. You can upload your application and documents that verify your group health plan coverage through your employer. You can also …

When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.Mar 26, 2022
How do you qualify for Medicaid and Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).Feb 11, 2022
How does Medicaid check income?
Documentation of income might include any of the following: Most current pay stubs, award letter for Social Security, SSI, Railroad Retirement, or VA, pension statement, alimony checks, dividend checks, a written statement from one's employer or from a family member who is providing support, or an income tax return.Mar 14, 2022
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
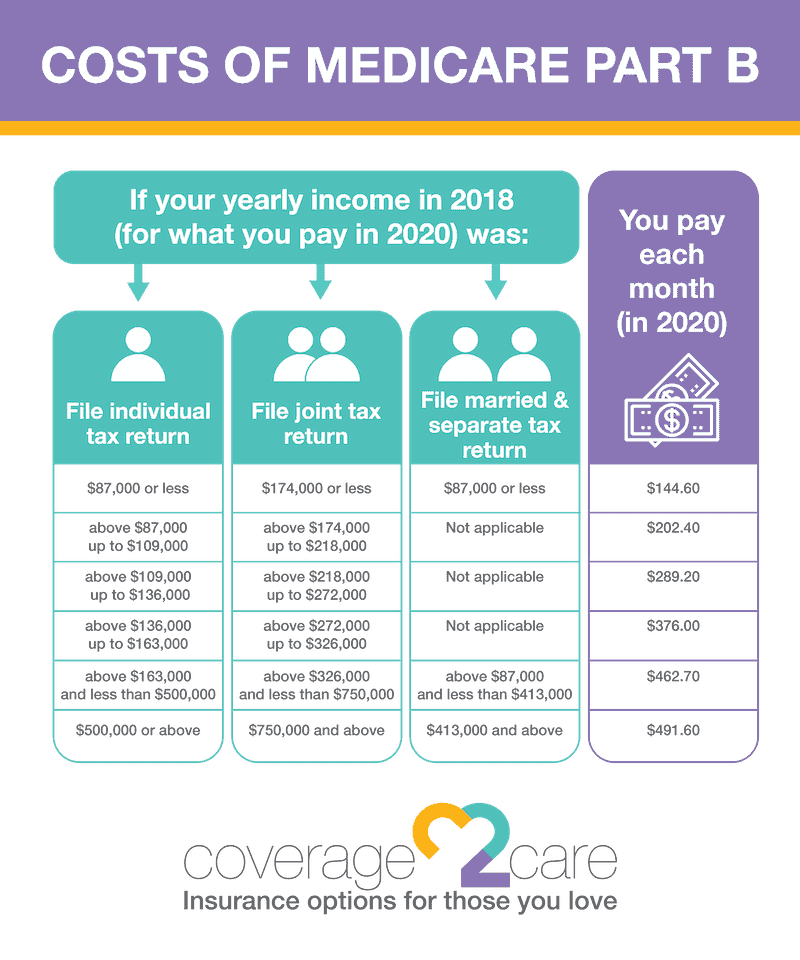
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
Why does Part A end?
There are special rules for when premium-free Part A ends for people with ESRD. Premium Part A and Part B coverage can be voluntarily terminated because premium payments are required. Premium Part A and Part B coverage ends due to: Voluntary disenrollment request (coverage ends prospectively); Failure to pay premiums;
Key takeaways
What costs should you expect if you’re moving from expanded Medicaid to Medicare?
Millions under expanded Medicaid will transition to Medicare
There are currently almost 20 million people covered under expanded Medicaid, accounting for almost a quarter of all Medicaid enrollees nationwide. Under ACA rules, there are no asset limitations for Medicaid eligibility for pregnant women, children, or adults eligible due to Medicaid expansion.
Moving from expanded Medicaid to Medicare Advantage
Depending on your circumstances, you might choose to enroll in a Medicare Advantage plan that provides prescription, dental, and vision coverage – and caps enrollees’ annual out-of-pocket costs for Parts A and B, which traditional Medicare does not do.
Transitioning from expanded Medicaid to Medigap
The more expensive way to cover the gaps in traditional Medicare is to buy a Medigap policy, which generally costs anywhere from a minimum of $25/month to more than $200/month to cover out-of-pocket costs for Parts A and B. That’s on top of premiums for Medicare Parts B and D (prescription drugs).
Medicare can pull you out of the coverage gap
Although the transition from expanded Medicaid to Medicare can be financially challenging, eligibility for Medicare will likely come as a welcome relief if you’ve been in the coverage gap in one of the 11 states that have refused to expand Medicaid.
What steps do I need to take to move from expanded Medicaid to Medicare?
If you’re enrolled in expanded Medicaid and you’ll soon be 65, you’ll want to familiarize yourself with the health coverage and assistance programs that might be available to you.
Legislation aims to make Medicare more affordable for lower-income Americans
The Improving Medicare Coverage Act, introduced in the U.S. House in September by Washington Representative Pramila Jayapal, would do away with cost-sharing and premiums for Medicare beneficiaries with income up to 200% of the poverty level (it would also lower the Medicare eligibility age to 60).
Does Medicaid cover cost sharing?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Is medicaid the primary or secondary insurance?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
Qualifying For Different Types Of Coverage
Medicare is a federal insurance program that helps pay medical bills from a fund to which users have contributed. It covers people 65 and older, people younger than 65 with certain disabilities and patients with end-stage kidney disease and other conditions requiring dialysis. Participants usually pay part of the cost.
Can I Select An Insurance Plan For My Medicare And Medicaid Benefits
If you are dual eligible, you are can enroll in a dual eligible special needs plan that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid dont over individually, including over-the-counter items, hearing aids, and vision or dental care.
If I Have Other Health Insurance Do I Need Part B
65 Incorporated came across this question from a Medicare beneficiary.
Do You Need Medicare Part B
Ever wonder if you really need Medicare Part B? For most people over 65 the answer is: Yes, you need to enroll in Part B and you should do so when first eligible. If you miss your Part B deadline, you could be subject to penalties. Check out our Medicare deadline Calculator here
Medicare Part B Enrollment And Penalties
Medicare Part B is optional, but in some ways, it can feel mandatory, because there are penalties associated with delayed enrollment. As discussed later, you dont have to enroll in Part B, particularly if youre still working when you reach age 65.
Do I Need Medicaid If I Have Medicare
Medicaid and Medicare are the two largest publicly funded health programs in the country, with different missions that often overlap. Medicare provides health coverage to seniors and some individuals with disabilities. Medicaid covers adults and children who cannot afford insurance, or who have health care costs they cannot afford.
What The Part B Late Enrollment Penalty
If you do not have creditable coverage after you first become eligible for Medicare Part B, you incur a penalty that you will pay when you eventually do enroll in Part B.
