What is the CMS dental program?
The Centers for Medicare & Medicaid Services (CMS) is committed to improving access to dental and oral health services for children enrolled in Medicaid and CHIP. We have been making considerable progress (PDF, 303.79 KB) in our efforts to ensure that low-income children have access to oral health care. From 2007 to 2011, almost half of all states (24) achieved at least a ten percentage point increase in the proportion of children enrolled in Medicaid and CHIP that received a preventive dental service during the reporting year. Yet, tooth decay remains one of the most common chronic childhood diseases.
What is a referral to a dentist for children?
A referral to a dentist is required for every child in accordance with the periodicity schedule set by a state. Dental services for children must minimally include: Relief of pain and infections. Restoration of teeth. Maintenance of dental health.
What is benchmark dental?
The benchmark dental package must be substantially equal to the (1) the most popular federal employee dental plan for dependents, (2) the most popular plan selected for dependents in the state's employee dental plan, or (3) dental coverage offered through the most popular commercial insurer in the state. States are also required to post ...
Do you need separate chip coverage for dental?
Dental coverage in separate CHIP programs is required to include coverage for dental services "necessary to prevent disease and promote oral health, restore oral structures to health and function, and treat emergency conditions.". States with a separate CHIP program may choose from two options for providing dental coverage: a package ...
Is dental insurance required for children?
Dental health is an important part of people's overall health. States are required to provide dental benefits to children covered by Medicaid and the Children's Health Insurance Program (CHIP), but states choose whether to provide dental benefits for adults.
Do you need to have dental insurance for adult?
There are no minimum requirements for adult dental coverage.
Does Medicaid cover dental care?
Medicaid covers dental services for all child enrollees as part of a comprehensive set of benefits, referred to as the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Though oral screening may be part of a physical exam, it does not substitute for a dental examination performed by a dentist.
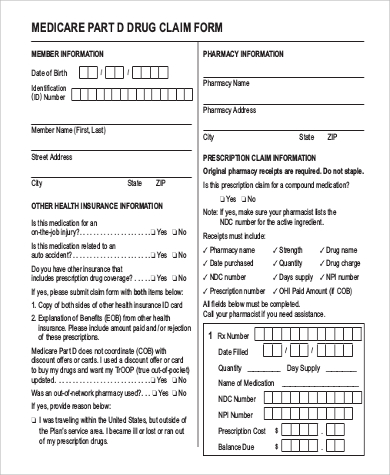
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
What is Medicare Advantage Dental?
Understanding Medicare Advantage dental coverage. Dental care is a vital part of maintaining your health and well-being, especially as you age. And one of the main perks of joining a Medicare Advantage (MA) plan is that many plans offer dental coverage to help you keep up with your oral health.
How long do you have to enroll in dental insurance in MA?
Members must enroll in this option when they enroll in their plan, or within 30 days of their plan’s start date.
How long does it take for Aetna to reimburse you for dental care?
You’ll pay for your dental care up front when you see a dentist, and then submit your receipts to Aetna to get reimbursed within four to six weeks. “With a direct member reimbursement allowance, you’re given a set amount of money to spend each year on dental care.”.
Does Medicare cover dental cleanings?
Original Medicare, on the other hand, does not cover routine dental care, such as cleanings, X-rays, and fillings. Due to the relatively high out-of-pocket costs for these procedures, some older adults end up forgoing necessary dental care. There is one exception, however: If you need medical dental procedures while you’re in the hospital, ...
Does Aetna have dental insurance?
Dental benefits are already included in the majority of Aetna MA plans. For some Aetna MA plans that don’t include dental coverage, you may have the choice of paying extra each month for dental benefits. This is done through an optional supplemental benefit.
How to contact a dental provider in California?
If you have any questions or need assistance finding a dental provider, call the Medi-Cal Dental Customer Service Line at (800) 322-6384, or visit Smile, California. DHCS encourages non-Medi-Cal dental providers to enroll with Medi-Cal.
What is DTI in dental?
Within the Medi-Cal 2020 Waiver, the Dental Transformation Initiative (DTI) represents a critical strategy to improve dental health for eligible Medi-Cal children by focusing on high-value care, improved access, and utilization of performance measures to drive delivery system reform.