The first step in enrollment for the QMB program is to find out if you’re eligible. A quick and easy way to do this is to call your local Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
Full Answer
What does QMB stand for in Medicare?
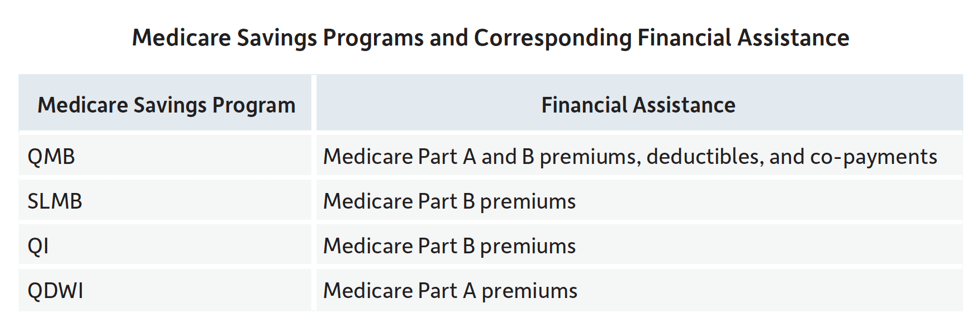
- The QMB Program is the Qualified Medicare Beneficiary program; Medicaid pays premiums for Part A and for Part B. ...
- The QDWI Program is the qualified disabled and working individuals program; it is a Medicare Assistance program for low or limited income persons. ...
- SLMB is the Specified Low-income Medicare Beneficiary program. ...
What is the income limit for QMB?
Someone can enroll in a QMB program providing they meet the monthly income limits. For an individual, the limit is $1,084 per month. For a married couple, the combined income must be less than $1,457 per month. The income limits are slightly higher in Alaska and Hawaii.
How to qualify for QMB?
To qualify for the QMB/SLMB program, applicants must meet three general eligibility requirements:
- Be enrolled in Part A Medicare (Hospital Insurance)
- Have resources not exceeding the QMB/SLMB resource maximums for an individual or couple. Refer to the Aged, Blind and Disabled Income and Asset Limit chart for current resource amounts.
- Have income not exceeding the QMB/SLMB standard of the Federal Poverty Level for the assistance group size
How do you qualify for QMB program?
You may be eligible if:
- You receive Medicare Part A,
- Your income must not be more than $867/month for one person or $1,167/month for a couple (These amounts change every April), and
- Your assets do not exceed $4,000 for yourself or $6,000 if you have one or more dependents living with you.

Is QMB automatic?
Beneficiaries who qualify for the QMB program automatically receive assistance with the costs of their prescription drugs through Extra Help.
Is QMB the same as Medicare?
The Qualified Medicare Beneficiary (QMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums. This Program helps pay for Part A premiums, Part B premiums, and deductibles, coinsurance, and copayments.
What does QMB mean on Medicare?
Qualified Medicare BeneficiaryIf you're among the 7.5 million people in the Qualified Medicare Beneficiary (QMB) Program, Medicare providers aren't allowed to bill you for services and items Medicare covers, including deductibles, coinsurance, and copayments. If a provider asks you to pay, that's against the law.
How much money can you have in the bank if your on Medicare?
You may have up to $2,000 in assets as an individual or $3,000 in assets as a couple. As of July 1, 2022 the asset limit for some Medi-Cal programs will go up to $130,000 for an individual and $195,000 for a couple. These programs include all the ones listed below except Supplemental Security Income (SSI).
Does Social Security count as income for QMB?
An individual making $1,000 per month from Social Security is under the income limit. However, if that individual has $10,000 in savings, they are over the QMB asset limit of $8,400.
What is a QMB patient?
The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program.
What does QMB without Medicare dollars mean?
This means that if you have QMB, Medicare providers should not bill you for any Medicare-covered services you receive.
Can you have Medicare and Medicaid?
Medicaid is a state and federal program that provides health coverage if you have a very low income. If you are eligible for both Medicare and Medicaid (dually eligible), you can have both. They will work together to provide you with health coverage and lower your costs.
What are the four factors of medical necessity?
Medicare defines “medically necessary” as health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Does Medicare look at your bank account?
Medicare will usually check your bank accounts, as well as your other assets when you apply for financial assistance with Medicare costs. However, eligibility requirements and verification methods vary depending on what state you live in. Some states don't have asset limits for Medicare savings programs.
Does Medicare look into your bank account?
Medicare plans and people who represent them can't do any of these things: Ask for your Social Security Number, bank account number, or credit card information unless it's needed to verify membership, determine enrollment eligibility, or process an enrollment request.
Does Medicare come out of your Social Security check?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
What is QMB in Medicare?
The Qualified Medicare Beneficiary ( QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program.
Can a QMB payer pay Medicare?
Billing Protections for QMBs. Federal law forbids Medicare providers and suppliers, including pharmacies, from billing people in the QMB program for Medicare cost sharing. Medicare beneficiaries enrolled in the QMB program have no legal obligation to pay Medicare Part A or Part B deductibles, coinsurance, or copays for any Medicare-covered items ...
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
How to enroll in QMB?
The first step in enrollment for the QMB program is to find out if you’re eligible. A quick and easy way to do this is to call your local Medicaid office. The next step is to complete an application. You can request Medicaid to provide you with an application form or locate a QMB program application from your state online.
What is a QMB premium?
The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
What is Medicare qualified?
A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays. Recipients must meet all criteria to qualify for the program assistance.
What is the QMB in North Carolina?
In North Carolina QMB is called MQB. If you live in Nebraska, Federal QMB is replaced with full Medicaid.
Why do you need a QMB with Advantage?
Pairing an Advantage Special Needs Plan with your QMB is a great way to protect yourself from unexpected health costs. It also provides extra benefits at an affordable price.
How to apply for QMB?
To apply for the QMB program, you’ll need to contact your state Medicaid office. You can check online to find your state’s office locations, or call Medicare at 800-MEDICARE. The documentation you’ll need varies by state, but your application process will likely include submissions of identification, proof of Medicare coverage, and financial information.
How to enroll in QMB?
To enroll in the QMB program, you first need to be enrolled in Medicare Part A. The next step is to review your income and assets to see if you fall below the limits set by Medicare. But remember there are exceptions to those limits, and you’re encouraged to apply even if your income or assets exceed them.
What is QMB program?
Since the QMB program aims to help individuals with low income, it places limits on the monthly income and financial resources available to you. If you exceed these limits, you may not be eligible for the program. Generally, participation is limited to individuals who meet the federal poverty level.
How long does it take to get a QMB denial?
Once you submit your application, you should receive a confirmation or denial within about 45 days. If you’re denied, you can request an appeal. Enrollment in any of the MSPs must be renewed each year. Even when your QMB is active, you may at times be wrongfully billed for items or services that it covers.
What is Medicare for older adults?
Medicare is meant to provide affordable healthcare coverage for older adults and other individuals in need. Even so, out-of-pocket costs can add up.
Can you be wrongfully billed for QMB?
Even when your QMB is active, you may at times be wrongfully billed for items or services that it covers. Contact Medicare for any billing problems. Be sure to carry documentation of your participation in the QMB program and show it to your providers.
Do you have to be a resident to qualify for QMB?
You must be a resident of the state in which you’re applying for the QMB program, and you must already be enrolled in Medicare Part A. Assets that aren’t counted when you apply for the QMB program include: your primary home.
What is QMB in Medicare?
Takeaway. The Qualified Medicare Beneficiary (QMB) program is one of the four Medicare savings programs. The QMB program helps those with limited income and resources pay for costs associated with Medicare parts A and B (original Medicare). To enroll in the QMB program, you must be eligible for Medicare Part A and meet certain income ...
What is QMB program?
The QMB program helps you pay for Medicare costs if you have lower income and resources. It’s estimated that more than 1 in 8 Medicare beneficiaries were enrolled in the QMB program in 2017.
What is Medicare savings program?
Medicare savings programs (MSPs) help people with limited income and resources pay for the costs of Medicare. There are four different MSPs available. The Qualified Medicare Beneficiary (QMB) program is one of them. The QMB program can help pay for Medicare costs including premiums, deductibles, coinsurance, and copays.
What are the eligibility criteria for QMB?
QMB eligibility. There are three different eligibility criteria for the QMB program. These include Medicare Part A eligibility, income limits, and resource limits. You can receive QMB benefits whether you have original Medicare (parts A and B) or a Medicare Advantage plan.
How much is the extra help for Medicare Part D 2021?
copays for prescriptions. Some pharmacies may still charge a small copay for prescriptions that are covered under Part D. For 2021, this copay is no more than $3.70 for a generic drug and $9.20 for each brand-name drug that is covered. Extra Help only applies to Medicare Part D.
What is the income limit for QMB 2021?
For 2021, the monthly income limits for the QMB program are: Individual: $1,094 per month. Married: $1,472 per month. Monthly income limits are higher in Alaska and Hawaii. Because of this, people living in these states may still be eligible for the QMB program, even if their monthly incomes are higher.
What is the enrollment process for Social Security?
The enrollment process requires you to fill out a short application form. The Social Security Administration (SSA) has a model form that can be found here. However, the form that you’ll actually fill out may be slightly different, depending on your state.
How to apply for QMB?
To apply for the QMB program, contact your state Medicaid program . Please not that if your income or financial resources are close to the totals listed above, you should still apply, as you may potentially be eligible.
What does QMB mean in Medicare?
QMB stands for “Qualified Medicare Beneficiary” and is a cost assistance program designed to help individuals who are eligible for both Medicare and Medicaid, a circumstance that is known as “dual eligibility.”
What is QMB insurance?
The QMB program helps pay for the full cost of Medicare Part A and Part B premiums along with complete coverage of deductibles, copayments and coinsurance. QMB offers the most comprehensive coverage of the programs available to dual-eligible beneficiaries.
What is a dual eligible special needs plan?
This is a particular type of Medicare Advantage plan with a benefits package that is tailored to the needs of those with the limited income and resources common among Medicaid recipients.
Can a QMB provider charge other Medicare beneficiaries?
Federal law prohibits providers from billing beneficiaries enrolled in the QMB program for any such costs. This law even pertains to non-participating providers, who are allowed to charge other Medicare beneficiaries more for care.
Do you have to be on Medicare to qualify for QMB?
You must be eligible for both Medicare and Medicaid to be eligible for QMB benefits. While Medicare’s eligibility requirements are federally mandated, each state may set its own qualifying restrictions for Medicaid.
Does QMB cover Medicaid?
The QMB improper billing protection even extends to health care providers who do not accept Medicaid. That means QMB members may receive care from a provider who does not accept Medicaid and still receive protection from deductibles, copayments and coinsurance.
What is QMB in Medicare?
QMB is one is of four Medicare Savings Programs designed to assist those with limited financial resources to more easily access Medicare coverage. These programs are federally funded and administered through state-run Medicaid agencies.
What is QMB program?
Beneficiaries who qualify for the QMB program automatically receive assistance with the costs of their prescription drugs through Extra Help. Also known as the Part D Low Income Subsidy, this program limits the costs you pay out of pocket to a few dollars per prescription.
How does QMB work?
The QMB program makes Medicare more accessible by paying for premiums, deductibles and cost-sharing of Medicare-covered expenses. About 7.7 million people, or 12.5% of people with Medicare coverage, receive assistance through the QMB program.
How to apply for qualified medicaid?
To apply for the Qualified Medicare Beneficiary program, contact your state Medicaid agency. Medicare encourages you to fill out an application if you think you might be eligible, even if your resources exceed the limits posted on their website.
What happens if you are charged for QMB?
If you're charged, advise the provider that you're enrolled in the QMB program. If you've made a payment while enrolled in the program, you're entitled to a refund.
Can a qualified Medicare beneficiary bill you?
Under the Qualified Medicare Beneficiary Program, health care providers are not permitted to bill you for Medicare services. QMB pays for:
Do you have to pay deductibles on QMB?
Once you're enrolled in the QMB program, you're no longer legally obligated to pay for deductibles, coinsurance or co-payments for any services or items covered by Medicare Part A or B.
What is a QMB?
The Qualified Medicare Beneficiary (QMB) Program is a Medicare Savings Program that helps pay for Medicare Part A and Part B premiums, deductibles, and coinsurance. Have countable assets at or below the program limit*. If there is one person in your family, the asset limit is $7,970.
When does medicaid start paying for Medicare?
If you are eligible for the Qualified Medicare Beneficiary Program, Medicaid will start paying for your Medicare Part A and B premiums, deductibles, and coinsurance the first day of the month after your application is approved .
How long does it take for Medicare to adjust for Social Security?
Even though you are enrolled in the Qualified Medicare Beneficiary Program in the month after your application is approved, your Social Security payment may not be increased for one to three months. This is the time that is needed for payments to be adjusted by Medicaid, Medicare, and the Social Security Administration.
How to contact Wisconsin Medigap?
Wisconsin offers a variety of resources to help Medicare beneficiaries understand options and solve problems related to their health insurance benefits: Call the Wisconsin Medigap Helpline at 800-242-1060. Contact your local aging and disability resource center. Contact a benefit specialist.
What is the maximum amount of assets you can have in your family?
Have countable assets at or below the program limit*. If there is one person in your family, the asset limit is $7,970. If there are two people in your family, the asset limit is $11,960.
Does medicaid pay Medicare Part A?
Medicaid should already be paying your Medicare Part A and B costs (meaning you do not need to apply for Qualified Medicare Beneficiary Program benefits) if you receive Medicare and Medicaid and either of the following apply to you: You are enrolled in the Supplemental Security Income (SSI) program. You were enrolled in SSI but lost it ...
What is the number to call for Medicare?
If your provider won't stop billing you, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048.
How to stop Medicare charges?
If you have a Medicare Advantage Plan: Contact the plan to ask them to stop the charges.
What is a Medicare notice?
A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare. It explains what the doctor, other health care provider, or supplier billed for, the Medicare-approved amount, how much Medicare paid, and what you must pay.
What is the QI program?
The QI Program is a state program that helps pay Part B premiums for people who have Part A and limited income and resources. You must apply every year for QI
How much money can you put aside for burial?
Up to $1,500 for burial expenses if you have put that money aside
Can you get help paying Medicare premiums?
You can get help from your state paying your Medicare premiums. In some cases, Medicare Savings Programs may also pay
Can you be charged for Medicare deductibles?
If you get a bill for Medicare charges: Tell your provider or the debt collector that you’re in the QMB Program and can’t be charged for Medicare deductibles, coinsurance, and copayments.
