What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.Apr 1, 2020
How long does it take to get CMS approval?
CMS is presently averaging between four and six months to provide a response. Failure to provide CMS with all the necessary information and documentation at the time of submission can result in a “development request” from CMS which can delay the approval process further.
What does it mean to be CMS certified?
Certification is when the State Survey Agency officially recommends its findings regarding whether health care entities meet the Social Security Act's provider or supplier definitions, and whether the entities comply with standards required by Federal regulations.
What is a Medicare provider?
A Medicare provider is a physician, health care facility or agency that accepts Medicare insurance. Providers earn certification after passing inspection by a state government agency. Make sure your doctor or health care provider is approved by Medicare before accepting services.
Does Medicare cover experimental drugs?
Routine costs associated with Medicare approved Clinical Trials is Medicare's financial responsibility. Experimental and investigational procedures, items and medications are not covered.Aug 17, 2021
What triggers payment of Medicare Part A benefits?
If you're under 65, you get premium-free Part A if: You have Social Security or Railroad Retirement Board disability benefits for 24 months. You have End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS) and meet certain requirements.
How is Medicare regulated?
Medicare is a federal health insurance program regulated by the Centers for Medicare and Medicaid Services (CMS). As a member currently enrolled in a CalPERS Medicare health benefits plan, you don't need to provide CalPERS with your new card or MBI number.Feb 23, 2022
What is the difference between credentialing and accreditation?
Credentialing is the umbrella term that includes concepts such as “accreditation,” “licensure,” “registration,” and professional “certification.” Credentialing establishes criteria for fairness, quality, competence and even safety for professional services provided.Feb 7, 2018
What is Medicare compliance?
The Medicare Compliance Program is specifically designed to prevent, detect, and correct noncompliance as well as fraud, waste, and abuse.
How do providers bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
What are provider types?
Provider types include individuals, facilities, and vendors. The provider's specialty is a value indicating what field of medicine a provider has additional education in to make him/her a specialist in a certain field.
How long does it take to get a Medicare provider number?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.Jan 25, 2022
What is included?
You will receive a personal Medicare provider number also known as your PTAN as well as a business Medicare PTAN.
What is not included?
If your business is a partnership or has more than one owner the additional charge for each additional therapist is $150 per therapist.
5 Common Mistakes to AVOID Before Starting PECOS Application for a Physical Therapist in Private Practice
1.) Make sure you have your CP 575 IRS Letter Ready to Scan and Upload – Click here for sample: Click Here
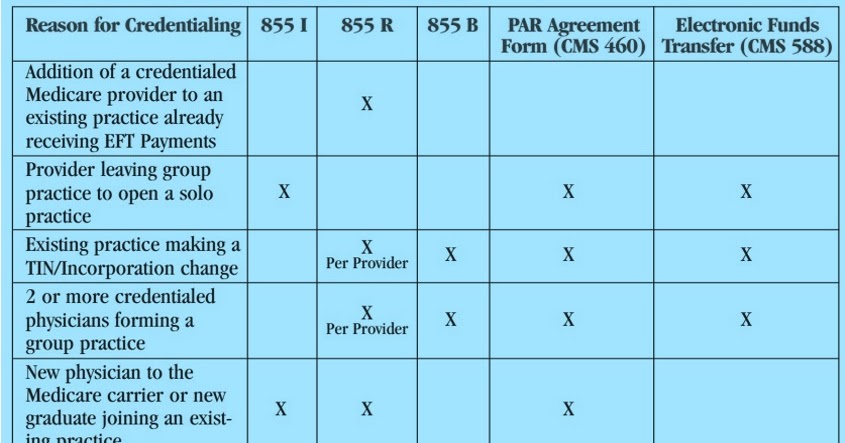
If you choose not to use PECOS, you may also enroll using paper applications
The CMS 855i is the individual enrollment for a sole proprietor or a sole owner.
Does a Physical Therapist Need To Enroll In Each Medicare Advantage Plan?
You are not automatically enrolled as a Medicare Part C ‘aka’ Medicare Advantage plan provider simply because you are enrolled in Medicare part B.
Is a Physical Therapist Required to Contract with Each Supplemental Plan?
Physical Therapists who are contracted Medicare providers do not contract with Medicare supplemental insurance plans.
What is Medicare application?
application is used to initiate a reassignment of a right to bill the Medicare program and receive Medicare payments (Note: only individual physicians and non-physician practitioners can reassign the right to bill the Medicare program).
What is NPI in Medicare?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. Suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
Earning Those Credentials
Getting credentialed (i.e., enrolling in an insurance company’s preferred provider network) requires more than merely filling out paperwork. It’s actually a fairly involved process.
Jumping Through Other Hoops
When a new therapist joins your practice, you’ll need to investigate his or her credentialing status with your insurance carriers. Now, even if you or your other therapists aren’t credentialed with a specific insurance company, you still have the option of billing as out-of-network providers.
How much advance notice do you need to credential a new provider?
As a practice grows, new providers are needed to manage heavier patient flow. Especially when this need is unexpected, a clinic owner may not have four to six months advance notice to fully credential a new clinician.
What is reciprocal billing?
Reciprocal billing definition: A reciprocal billing arrangement is an agreement between physicians to cover each other’s practice when the regular physician is absent. This is usually an informal arrangement and is not required to be in writing.
Why do clinics need to fill roles?
A clinic may need to fill a role quickly due to the unexpected loss of a provider ( i.e. termination or leave without notice), or temporarily when a clinician is absent due to illness, pregnancy, vacation, or other situations .
What is locum tenens?
Locum Tenens Definition: A locum tenens is considered a substitute physician, who is only intended to fill in for an absent physician and does not plan to join the urgent care practice. Locum physicians may only practice and bill for 60 days.
Do you have to follow Medicare policy for reciprocal billing?
Verify with your contracted health plans to make sure you are following your contract and billing policies for reciprocal billing. If you do not know what is required by a specific payer, again, it is a good rule of thumb to follow Medicare policy.
Can locum physician be billed under NPI?
Locum physician services can be billed under the NPI of the doctor absent, with the Q6 modifier (service provided by a locum physician) added to each CPT code on the claim. If the locum physician performs post-op services in the global period—the substitute services do not need to be identified on the claim. Practices must maintain a record of patients seen by the locum physician (including the locum’s NPI), and this listing should be made available to commercial insurance carriers if needed.
