Part B New Provider Resource Center
- Enroll in the CGS ListServ Notification Service and CMS Listserv. ...
- Become familiar with the CGS and CMS Websites. Access the CGS Part B Website for a variety of educational, billing, and coverage information. ...
- Enroll and Learn About Electronic Billing and myCGS. Read the Electronic Enrollment Packet. This packet provides information about submitting your claims electronically to Medicare.
- Get Acquainted with Medicare. Below is a list of critical resources you will need for providing and billing Medicare-covered services.
Full Answer
When do I have to apply for Medicare Part B?
Jan 01, 2022 · I have Part A & want to add Part B. Contact Social Security to sign up for Part B: Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). Send the completed form to your local Social Security office by fax or mail. Call 1-800-772-1213. TTY users can call 1-800-325-0778. Contact your local Social Security office.
How do you enroll in Medicare Part B?
ENROLLMENT. Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Step 2: Complete the Proper Medicare Enrollment Application. Step 3: Respond to MAC Requests for More Information. Step 4: Use PECOS to Keep ...
How can I sign up for Medicare Part B?
Oct 27, 2020 · Information for Physicians, Practitioners, Suppliers, & Institutional Organizations. Access PECOS - the. Medicare Enrollment System. Become a Medicare. Provider or Supplier. Pay the Medicare. Application Fee. Revalidations (Renewing. Your Enrollment)
Where do I apply for Medicare Part B?
Oct 02, 2019 · In order for you to do that, you must first complete an online application at the United States Department of Health and Human Services website. This online application process is called the Providers Enrollment, Chain and Ownership System (PECOS). This is the only way for you to apply to become a Medicare provider in the United States. Once you apply, a Medicare …
What is a Medicare Part B provider?
How do I submit Medicare Part B?
- Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). ...
- Call 1-800-772-1213. ...
- Contact your local Social Security office.
- If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
What does it mean to be CMS certified?
What is the difference between 855I and 855R?
How long does it take for Medicare Part B to go into effect?
Can Medicare Part B be added at any time?
If you are eligible for the Part B SEP, you can enroll in Medicare without penalty at any time while you have job-based insurance and for eight months after you lose your job-based insurance or you (or your spouse) stop working, whichever comes first.
How long does it take to become Medicare certified?
What is the difference between credentialing and accreditation?
Does Medicare have to be accredited to Bill?
How do I submit my Pecos 855R?
What is Medicare third party reassignment?
What is CMS 855I used for?
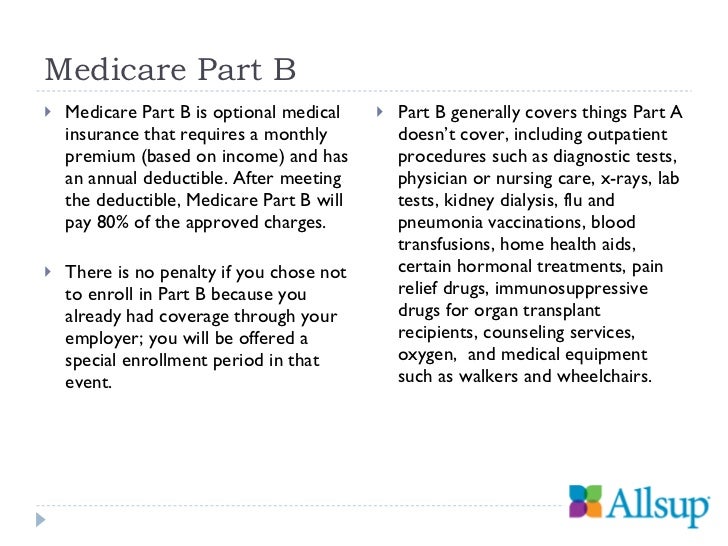
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
Do health care providers have to enroll in Medicare?
Health care providers must enroll in the Medicare Program to get paid for providing covered services to Medicare patients. Learn how to determine if you’re eligible to enroll and how to do it.
How much is the Medicare application fee for 2021?
Application Fee Amount. The enrollment application fee sent January 1, 2021, through December 31, 2021, is $599. For more information, refer to the Medicare Application Fee webpage. How to Pay the Application Fee ⤵. Whether you apply for Medicare enrollment online or use the paper application, you must pay the application fee online:
Does Medicare require EFT?
If enrolling in Medicare, revalidating, or making certain changes to their enrollment, CMS requires E FT. The most efficient way to enroll in EFT is to complete the PECOS EFT information section. When submitting a PECOS web application:
How long does it take to change Medicare enrollment?
Providers and suppliers must report a change of ownership or control, a change in practice location, and final adverse legal actions (such as revocation or suspension of a federal or state license) within 30 days of the change and report all other changes within 90 days of the change.
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
Can MACs see Medicare PECOS?
Only you, authorized surrogates, authorized CMS officials, and MACs may enter and view your Medicare PECOS enrollment information. CMS officials and MACs get security standards training and must protect your information. CMS doesn't disclose your Medicare enrollment information to anyone, except when authorized or required by law.
Step 1: Enroll in the CGS ListServ Notification Service and CMS Listserv
Sign up for the CGS ListServ Notification Service, which is the primary means used by CGS to communicate new or changing Medicare information with providers. CGS also communicates information via Facebook, and Twitter.
Step 2: Become familiar with the CGS and CMS Websites
Access the CGS Part B Website for a variety of educational, billing, and coverage information.
Step 3: Enroll and Learn About Electronic Billing and myCGS
Read the Electronic Enrollment Packet. This packet provides information about submitting your claims electronically to Medicare. You must bill your claims electronically, unless you meet the exception for a small provider. Complete the Electronic Data Interchange (EDI) forms, which can be accessed from the Electronic Enrollment Packet.
Step 4: Get Acquainted with Medicare
Below is a list of critical resources you will need for providing and billing Medicare-covered services. Consider bookmarking these web addresses for future reference.
How many Medicare beneficiaries are there?
Seize a huge business opportunity. There are over 31 million Medicare beneficiaries and this number continues to grow as the baby boomers age.
Is Medicare more black and white?
Participating in Medicare is simpler than you think: While Medicare rules and regulations may appear complicated, they actually are more “black and white” than those of private payers and are consistent no matter the state in which you practice.
