To become a First Steps provider or service coordinator, all individuals must: Submit an enrollment application Email [email protected] to receive instructions to complete a Provider Enrollment Screening application and provide any required supporting documentation as indicated. Obtain a limited criminal history check through the Indiana ...
Full Answer
Why become an Indiana health coverage programs provider (IHCP)?
By becoming an Indiana Health Coverage Programs (IHCP) provider, you have the opportunity to improve the health and well-being of more Hoosiers, including the state’s most vulnerable populations. Through programs such as Traditional Medicaid, the Healthy Indiana Plan (HIP), Hoosier Healthwise, and Hoosier Care Connect, the IHCP performs a vital public service, …
How do I become a provider with Ohio Medicaid?
You can apply for an NPI on the NPPES website. Not sure if you have an NPI? Search the NPI Registry. 2 Step 2: Complete the Medicare Enrollment Application Enroll using PECOS, the online Medicare enrollment system. PECOS has video and print tutorials and will walk you through your enrollment to ensure your information is accurate.
Where can I find Medicare enrollment information for providers?
Dec 01, 2021 · Enroll as a Medicare provider or supplier Review information currently on file Upload your supporting documents Electronically sign and submit your information online Because PECOS is paperless, you no longer need to submit anything by mail. Additionally, PECOS applications tend to process faster than paper applications. Enroll online using PECOS.
How do I check the status of my NPI application?
To become a First Steps provider or service coordinator, all individuals must: Complete the online provider enrollment screening here. During the enrollment process providers and service coordinators will be asked to complete the following: Submit limited criminal history check through the Indiana State Police;

What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.Apr 1, 2020
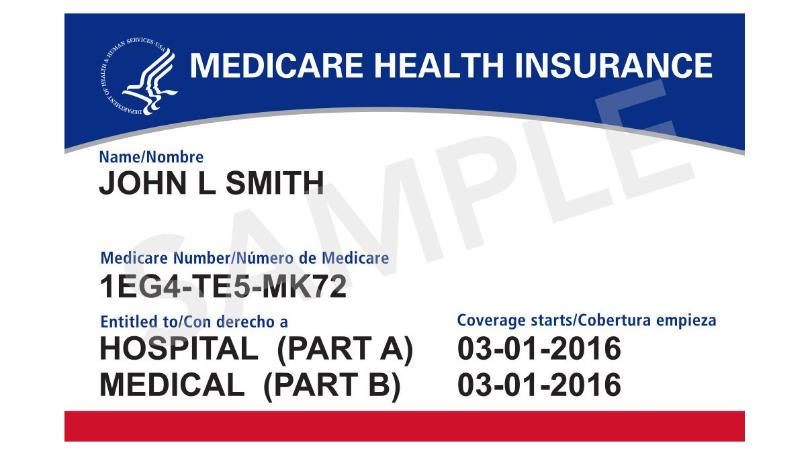
What is a Medicare Part B provider?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers. medically necessary.
What is Pecos certification?
PECOS is the online Medicare enrollment management system which allows you to: Enroll as a Medicare provider or supplier. Revalidate (renew) your enrollment. Withdraw from the Medicare program. Review and update your information.Dec 1, 2021
What is a Pecos provider?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.Dec 11, 2020
How long does it take to get a Medicare provider number?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.Jan 25, 2022
Does Medicare Part B pay 80 percent?
You will pay the Medicare Part B premium and share part of costs with Medicare for covered Part B health care services. Medicare Part B pays 80% of the cost for most outpatient care and services, and you pay 20%. For 2022, the standard monthly Part B premium is $170.10.
How do I add a practice place to Medicare?
0:3811:30PECOS Enrollment Tutorial – Adding a Practice Location (DMEPOS Only)YouTubeStart of suggested clipEnd of suggested clipHere you can see a summary of information such as the enrollment state the corresponding status ofMoreHere you can see a summary of information such as the enrollment state the corresponding status of the application the specialty type the practice location along with additional information.
What does Caqh stand for?
The Council for Affordable Quality Healthcare®The Council for Affordable Quality Healthcare® (CAQH) is a non-profit alliance of health plans and related associations working together to achieve the shared goal of streamlining the business of healthcare.
How often is Medicare revalidation required?
every five yearsYou're required to revalidate—or renew—your enrollment record periodically to maintain Medicare billing privileges. In general, providers and suppliers revalidate every five years but DMEPOS suppliers revalidate every three years. CMS also reserves the right to request off-cycle revalidations.Dec 1, 2021
Who needs to enroll in Pecos?
CMS developed PECOS as a result of the Patient Protection and Affordable Care Act. The regulation requires all physicians who order or refer home healthcare services or supplies to be enrolled in Medicare.
What is a CMS 855?
CMS 855A. Form Title. Medicare Enrollment Application - Institutional Providers.
Is the Medicare provider number the same as NPI?
What are the NPI and CCN numbers? The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
What is Hoosier Care Connect?
Hoosier Care Connect is a coordinated care program for Indiana Health Coverage Programs (IHCP) members age 65 and over, or with blindness or a disability who are residing in the community and are not eligible for Medicare. Members will select a managed care entity (MCE) responsible for coordinating care in partnership with their medical providers. Hoosier Care Connect members will receive all Medicaid-covered benefits in addition to care coordination services. Care coordination services will be individualized based on a member’s assessed level of need determined through a health screening.
What is MHS plan?
MHS' plan is called Ambetter from MHS. Ambetter offers affordable health care coverage for individuals and families. Depending on family size and income, a person may even qualify for help to pay their monthly premium.
What is a HIP 2.0?
The Healthy Indiana Plan (or HIP 2.0) is an affordable health insurance program from the State of Indiana for uninsured adult Hoosiers. The Healthy Indiana Plan pays for medical expenses and provides incentives for members to be more health conscious.
BECOME A REGISTERED USER
You may register for a user account if you are: an Individual Practitioner, Authorized or Delegated Official for a Provider or Supplier Organization, or an individual who works on behalf of Providers or Suppliers.
Helpful Links
Application Status - Self Service Kiosk to view the status of an application submitted within the last 90 days.
