Answer: CPT code 67820 Correction of trichiasis; epilation, by forceps only is payable per eye. For a Medicare Part B patient, bill 67820 -50 modifier and 1 unit. Other payers may prefer to see two lines using the modifiers –RT and –LT.
Full Answer
What is the CPT code 67820?
Feb 22, 2015 · Answer: CPT code 67820 Correction of trichiasis; epilation, by forceps only is payable per eye. For a Medicare Part B patient, bill 67820 -50 modifier and 1 unit. Other payers may prefer to see two lines using the modifiers –RT and –LT.
What is the modifier for Bill 67820-50?
on two lines with 67820-E2 and 67820-E4. But for a patient with lashes removed from the upper left and lower left lids, he should only append modifier LT, because you can only bill once per eye. Report Plugs Once Per Lid Most Medicare carriers want you to report code 68761 (Closure of the lacrimal punctum; by plug, each) once per eyelid, using E1-E4.
What are HCPCS billing codes?
ifies, “Codes 67820 and 67825 are intended to be reported per proce - dure, not per eyelash or per eyelid.” 3 However, for Medicare, the indicator is 1 so you may bill the code per eyelid but not per lash. Getting paid These coding guidelines are often not well known and therefore not followed. For Medicare, payments are calculated by RVUs (relative
What are the ophthalmology coding procedures for Medicare carriers?
on each eye, code epilation of a lash on either the upper or lower left lid (67820-LT), and code a lash on either the upper or lower right lid (67820-RT). If your carrier pays by the lid and you remove a lash on the upper left and lower right lids, report 67820-E1 and 67820-E4. Charge for Punctal Plug Supply
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
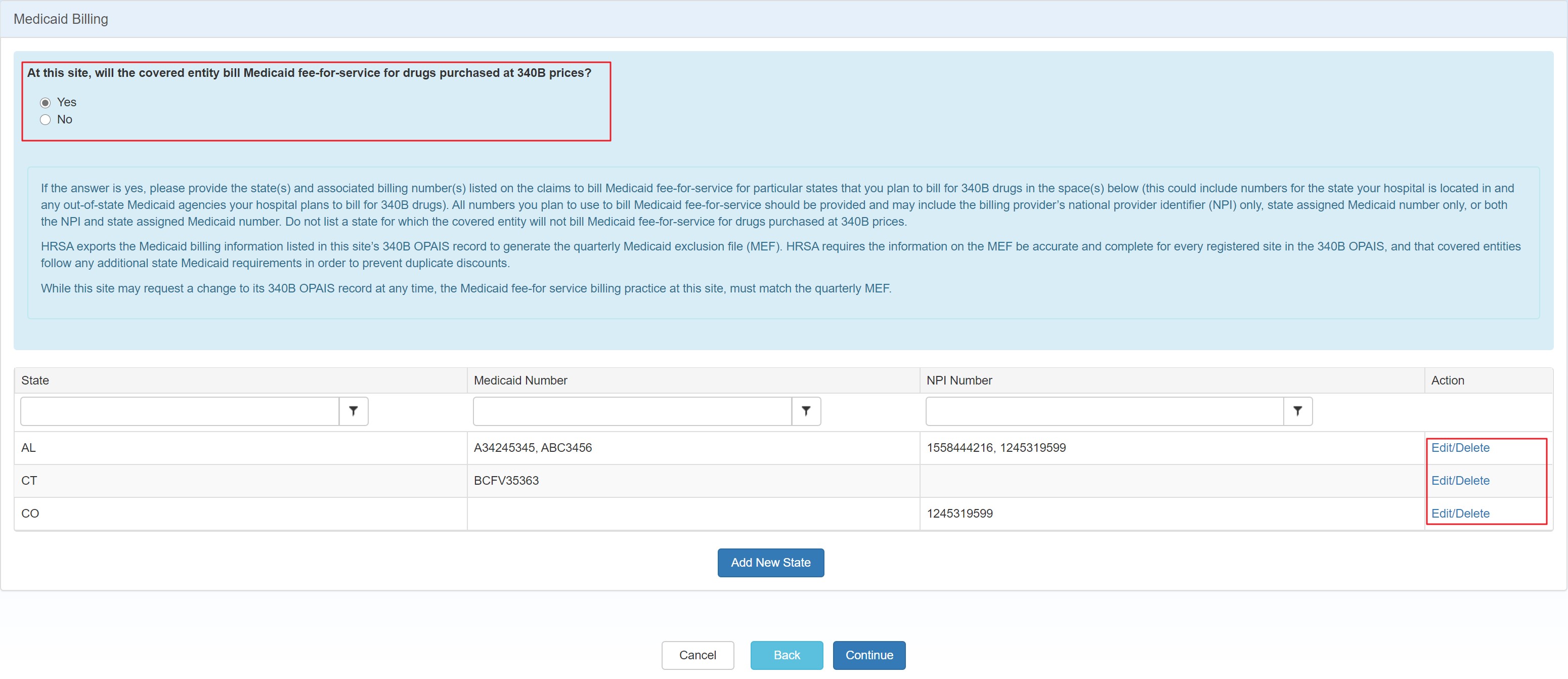
In order to facilitate claims processing and avoid denials for duplicate claims, claims which contain CPT®/HCPCS codes describing services performed on anatomic structures that can be distinguished as left or right require laterality modifiers.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is HCPCS code?
HCPCS codes are standardized five-character, alpha-numeric code sets used for billing Medicare and Medicaid patients that correspond to services, procedures, and equipment not covered by CPT® codes. The Centers for Medicare and Medicaid Services (CMS) monitors HCPCS billing codes. CPT codes are published by the American Medical Association® ...
What is a CPT modifier?
Modifiers are added to the Healthcare Common Procedure Coding System (HCPCS) or Current Procedural Terminology (CPT®) codes to provide additional information necessary for processing a claim, such as identifying why a doctor or other qualified healthcare professional provided a specific service and procedure.
What is a modifier 24?
Modifier 24 Definition: “Unrelated evaluation and management (E/M) service by the same physician or other qualified health care professional during a postoperative period.”. Modifier 24 is used when a doctor provides co-management services. It is only used to append to E/M codes.
What is the financial health of an eye care practice?
The financial health of any eye care practice depends on complete ophthalmology and optometry billing solutions and revenue cycle management. It’s critical to pay close attention to using modifiers correctly, accurately documenting patient records and physician notes, and ensuring claims are not under or over-coded.
What modifier do you use for cataract surgery?
For example, if a patient has cataract surgery and experiences complications in the eye not operated on—or if the patient suffers complications in the operated eye and it’s located in the region of the eye that was not impacted by the surgery—you can append modifier 24.
How much is Medicare audit fine?
Medicare audit fines might be as high as $10,000 for each occurrence. This means every time you bill a modifier on a claim incorrectly, you may have to pay $10,000 for each occurrence.
How many characters are in a CPT code?
CPT codes are published by the American Medical Association® and consist of three types or categories of five-character codes and two-character modifiers to describe any changes to the procedure.
