1) Submit a claim with the FULL billing amount you usually bill. a. Date of Service should be Date of Refusal or Date of Death 2) Include in the narrative section a brief explanation of the situation. Mention that the item ‘has no salvage value and is a complete loss’.
Full Answer
Can Medicare deny a claim that has already been billed?
Therefore, claims for services that have already been billed to Medicare shall be denied (with appeal rights) by Medicare’s contractors. In addition, Medicare payment cannot be made under the IPP for services that are payable for a particular beneficiary under any other Part of Medicare.
How does Medicare determine whether to Bill or not?
Such determinations are made by Medicare when processing related claims. Sometimes, providers and beneficiaries make their own agreements on payment without billing Medicare, which Medicare allows them to do. More often, Medicare is billed, since resulting denials of claims, even when submitted with non-
How does Medicare pay billing and collection services?
The Medicare program may make payment in the name of the provider to an agent who furnishes billing or collection services. The payment arrangement between the provider and an agent must meet the same requirements as the payment arrangement between a physician and an agent. (See §30.2.4 for payment to an agent of a physician.) Indirect Payment.
What do I do if my Medicare claim is not filed?
If your claims aren't being filed in a timely way: Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I bill a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Does Medicare accept paper secondary claims?
The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.
Can you submit your own claims to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Does Medicare accept replacement claims?
RTP claims are not finalized claims and do not appear on your Remittance Advice (RA). Therefore, you may submit a new (corrected) claim and it will not reject as a duplicate to the original claim. You must submit a new claim if: You do not have access to the DDE system.
What are Medicare Secondary Payer rules?
Generally the Medicare Secondary Payer rules prohibit employers with 20 or more employees from in any way incentivizing an active employee age 65 or older to elect Medicare instead of the group health plan, which includes offering a financial incentive.
How does Medicare Secondary Payer work?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
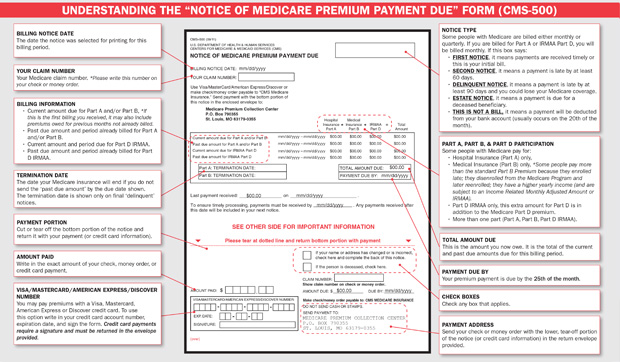
What form is used to send claims to Medicare?
The CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is a 1490 form?
A CMS 1490s form will be used by the Centers for Medicare and Medicaid Services. This particular form is known as the Patient's Request for Medical Payment form. This is a commonly used form that will be submitted in order to request that a medical service be covered under Medicare or Medicaid.
Can you submit Medicare claims online?
Submit your completed Patient's Request for Medical Payment form, itemized medical bill or bills, and any supporting documents to your state's Medicare contractor. All claims must be submitted by mail; you can't file a Medicare claim online.
What goes in box 33 on a HCFA?
Box 33 is used to indicate the name and address of the Billing Provider that is requesting to be paid for the services rendered.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
What is a 130 bill type?
TOBs that have a value of “non-pay”—those which end with a zero—will not receive payment for services. Examples include 110 (inpatient hospital non-pay) and 130 (outpatient hospital non-pay).
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article contains coding guidelines that complement the Local Coverage Determination (LCD) for Salvage High-intensity Focused Ultrasound (HIFU) Treatment in Prostate Cancer (PCa).
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
How to determine Part B payment?
To determine the Part B payment to a provider other than nominal charge provider, A/B MACs (A) and (HHH) subtract any unmet Part B deductible from the lower of the actual charge or the fee schedule amount for the item or service and multiply the remainder by
How to determine Part B payment to nominal charge?
To determine the Part B payment to a nominal charge HHA , A/B MACs (HHH) subtract any unmet Part B deductible from the fee schedule amount and multiply the remainder by
How to determine liability to a provider other than an HHA?
To determine patient liability to a provider other than an HHA (including nominal charge providers other than a HHA), A/B MACs (A) subtract any unmet deductible from the actual charge and multiply the remainder by 20 percent. The result, plus the unmet deductible is the patient's liability. Coinsurance is applied as applicable.
What is an enteral care kit?
Enteral care kits contain all the necessary supplies for the enteral patient using the syringe, gravity, or pump method of nutrient administration. Parenteral nutrition care kits and their components are considered all-inclusive items necessary to administer therapy during a monthly period.
How long do DME MACs pay rental fees?
For these items of DME, A/B MACs (HHH) and DME MACs pay the fee schedule amounts on a monthly rental basis not to exceed a period of continuous use of 15 months. In the tenth month of rental, the beneficiary is given a purchase option (see §30.5.2). If the purchase option is exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees not to exceed a period of continuous use of 13 months and ownership of the equipment passes to the beneficiary. If the purchase option is not exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees until the 15 month cap is reached and ownership of the equipment remains with the supplier (see §30.5.4). In the case of electric wheelchairs only, the beneficiary must be given a purchase option at the time the equipment is first provided (see §30.5.3).
What is PIM in Medicare?
Chapter 5, section 5.2.1 of the Medicare Program Integrity Manual (PIM) states that, in order for Medicare to make payment for an item of Durable Medical Equipment Prosthetic, and Orthotic Supplies (DMEPOS), the DMEPOS supplier must obtain a prescription from the
What is the CPM code for DME?
The CPM devices (HCPCS code E0935) are classified as items requiring frequent and substantial servicing and are covered as DME as follows (see the Medicare National Coverage Determinations Manual.):
What is the minimum number of codes required for a remittance notice?
The remittance advice must demonstrate all applicable error codes. However, there must be a minimum of two codes on the remittance notice (including code MA130). 2.
Do interim bills have to include charges billed on an earlier claim?
Each bill must include all applicable diagnoses and procedures. However, interim bills are not to include charges billed on an earlier claim since the “From” date on the bill must be the day after the “Thru” date on the earlier bill. No-payment bills should be submitted until the beneficiary is discharged.
Does a hospital use a summary log?
The hospital uses the summary log for late charges only under cost settlement (outpatient hospital), except in Maryland. Maryland and cost hospitals are required to meet the 27-month timeframe for timely filing of claims, including late charges.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…