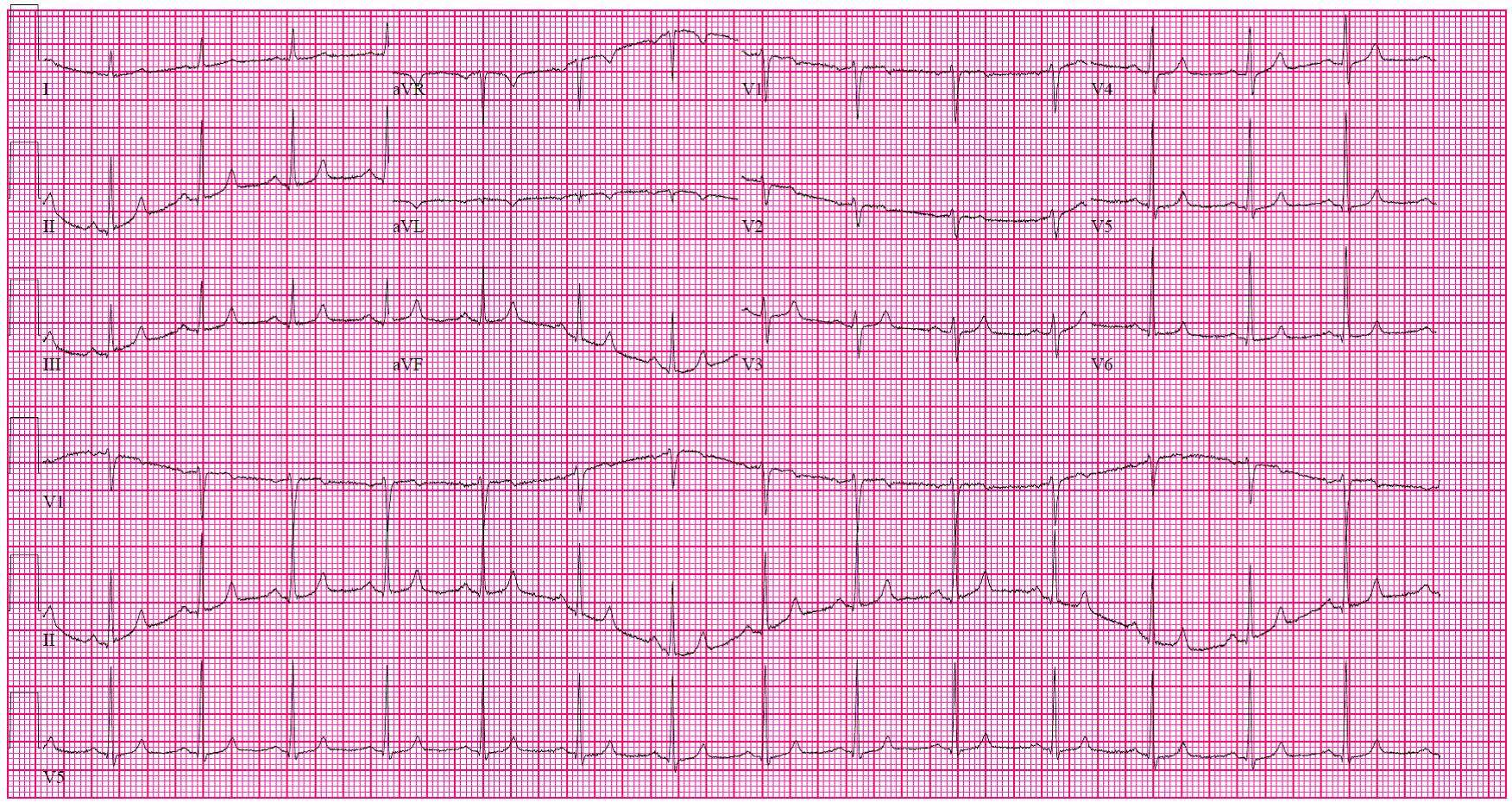
If an EKG
Electrocardiography
Electrocardiography is the process of producing an electrocardiogram, a recording – a graph of voltage versus time – of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle. Changes in the normal EC…
Will Medicare pay for an EKG?
Click here or call 1-800-729-9590. Medical Billing Advice: EKG and Medicare Billing. EKGs are what we we're going to talk about. Someone had asked about, they were having trouble getting their EKGs covered in the Medicare yearly physical, so they were billing annually for EKGs saying that the doctor and the patient had the understanding that EKGs were covered in the initial …
Does Medicare Part B cover electrocardiograms?
Apr 21, 2013 · EKG and Medicare Billing — VIDEO. November 20, 2016. April 21, 2013 by Laureen Jandroep. EKG and medicare billing s are what we we’re going to talk about. Someone had …
Does Medicare cover EKG g0404?
Electrocardiogram (EKG or ECG) screenings. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. A written order from your primary care doctor …
What is the CPT code for electrocardiogram?
Aug 09, 2019 · I do the coding and billing for a Rural Health Clinic and one of the providers is billing a G0402(Initial preventative physical exam-face to face visit) as well as G0403(EKG …
Does 93000 need a modifier for Medicare?
Is an EKG included in the Welcome to Medicare visit?
How do I bill Medicare for EKG?
Is EKG included in G0402?
What ICD 10 codes cover EKG?
Is an EKG included in a wellness exam?
Because they cost little and don't require incisions or needles, doctors often use EKGs to screen for heart disease in people who have no symptoms. You might receive one during your regular physical exam, especially if you have a close family member with heart disease.
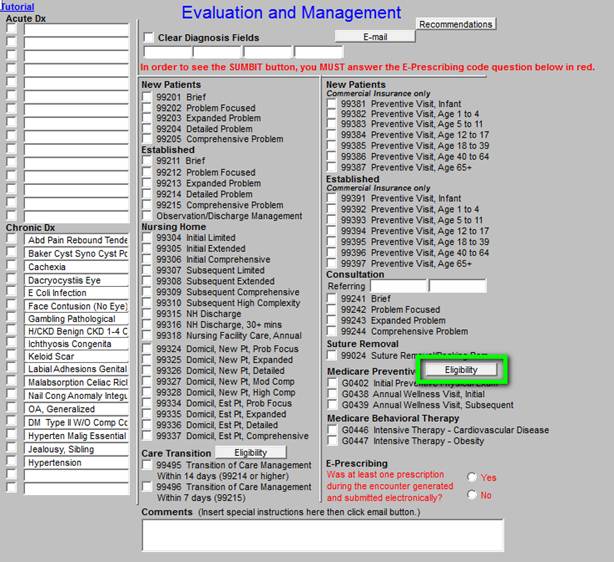
What are the CPT codes for EKG?
| Applicable CPT Codes | Description |
|---|---|
| 93000 | Electrocardiogram, routine ECG with at least 12 leads; with interpretation and report |
| 93005 | Electrocardiogram, routine ECG with at least 12 leads; tracing only, without interpretation and report |
Can 93000 and 93040 be billed together?
What is the CPT code for EEG?
| Code | Description |
|---|---|
| 95700 | ELECTROENCEPHALOGRAM (EEG) CONTINUOUS RECORDING, WITH VIDEO WHEN PERFORMED, SETUP, PATIENT EDUCATION, AND TAKEDOWN WHEN PERFORMED, ADMINISTERED IN PERSON BY EEG TECHNOLOGIST, MINIMUM OF 8 CHANNELS |
Can you bill EKG with G0438?
How often can you bill for G0179?
Is EKG required for Ippe?
How many payments are made for one interpretation of an EKG?
CMS Manual System, Publication 100-04, Medicare Claims Processing Manual, Chapter 13, §100.1, states that in general only one payment is made for one interpretation of an EKG.
What does an ECG provider need to keep in its records?
A laboratory or a portable X-ray supplier that supplies an ECG must maintain in its records the referring physician’s written order and the identity of the employee taking the tracing.
What is a double payment for EKG?
For double reading of an EKG, a similar circumstance must apply, an unusual reason why a second interpretation (for example, a reading by a cardiologist) was specifically medically necessary. Otherwise, the second interpretation must be denied per the manual as a “quality control service.”
What is the Medicare Carriers Manual?
Medicare Carriers Manual, §15047 (G), explains how to report preoperative tests. (The reference will be crosswalked to the CMS Manual System, Publication 100-04, Medicare Claims Processing Manual, Chapter 12, §30.6.6.1 as soon as it becomes available.)
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
Why do contractors specify bill types?
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service . Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type. Complete absence of all Bill Types indicates that coverage is not influenced by Bill Type and the article should be assumed to apply equally to all claims.
When several ECG rhythm (or monitor) strips from a single date of service are reviewed at a single answer
When several ECG rhythm (or monitor) strips from a single date of service are reviewed at a single setting, report only one unit of service, regardless of the number of strips reviewed.
What is Medicare Advantage?
Medicare Advantage plans are an alternative way to receive your Medicare Part A and Part B coverage, and these plans may have lower costs than Original Medicare. Medicare Supplement plans work alongside your Original Medicare coverage and may help pay for certain out-of-pocket costs.
What are the problems that a heart scan might reveal?
In addition to coronary artery disease, other medical problems that a heart scan might uncover include congenital defects, inflammation, and arrhythmia (a heartbeat that is too slow, too rapid, or irregular).
Does Medicare cover electrocardiograms?
Beneficiaries with Medicare Part B may be covered for electrocardiograms in certain circumstances:
Can you work with your doctor to treat heart problems?
However, people can work with their doctors to proactive ly detect and treat heart problems before they become life-threatening emergencies. Find affordable Medicare plans in your area. Find Plans.
Can a doctor refer you for a heart scan?
A medical practitioner might refer you for a heart scan at another time as a medically necessary diagnostic test.
Does Medicare cover EKGs?
Medicare Coverage of Electrocardiograms (EKGs) According to the Centers for Disease Control and Prevention, or CDC, Americans suffer from coronary artery disease more than any other kind of heart disease. Tragically, the first time that many people realize they have this disease is after they suffer from a heart attack.
What are the indications for ECG?
The following are indications for which the ECG is appropriate: Cardiac ischemia or infarction (new symptoms or exacerbations of known disease). Anatomic or structural abnormalities of the heart such as congenital, valvular or hypertrophic heart disease. Rhythm disturbances and conduction system disease.
What happens if CPT modifier 77 is not appropriate?
If CPT modifier 77 is not appropriate, both the physician treating the patient in the emergency room and the radiologist may still submit documentation with the initial claim to support that the interpretation results were provided in time and/or used in the diagnosis and treatment of the patient.
What are the patient-specific predictors of cardiac disease?
Patient-specific predictors are such things as age, absence or presence of cardiac disease or dysfunction, current and recent stability of cardiac symptoms and syndromes, and the absence or presence of comorbid conditions known to increase the risk that undisclosed cardiac disease is present. Surgery-specific risks relate to the type of surgery and its associated degree of hemodynamic stress. High-risk procedures include major emergency surgery, aortic and major vascular surgeries, peripheral vascular surgery and prolonged procedures associated with large fluid shifts or blood loss. Intermediate-risk procedures include carotid endarterectomy, prostate surgery, orthopedic procedures, head and neck procedures, intraperitoneal and intrathoracic surgery. Low-risk procedures include endoscopy, superficial procedures, cataract surgery and breast surgery.
What is the CPT code for Palmetto GBA?
The physician reviews the X-ray, treats, and discharges the beneficiary. Palmetto GBA receives a claim from a radiologist for CPT code 71010-26 indicating an interpretation with written report with a date of service of January 3. Palmetto GBA will pay the radiologist’s claim as the first bill received.
Is preoperative electrocardiography covered by Medicare?
Medicare coverage of preoperative electrocardiography is limited to those patients who possess one or more patient-specific indicators of increased risk for perioperative cardiac morbidity and who will undergo surgery of high or intermediate risk of cardiac morbidity/mortality. Preoperative ECGs performed in circumstances other than those listed above are considered screening and should be billed accordingly.
Do CPT codes have long descriptors?
Providers are reminded to refer to the long descriptors of the CPT codes in their CPT book. The American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS) require the use of short CPT descriptors in policies published on the Web.
Is orthostatic hypotension supported in the record?
3.Orthostatic hypotension should be supported in the record with specific vital signs or measurements, and clinical manifestations whenever possible. This note provided clear documentation to support the orthostatic hypotension and the link with the patient’s initial dehydration and hypovolemia. Given the patient’s presentation, and the resolution of the orthostatic intolerance with IV fluids, addressing the coding for autonomic dysfunction syndrome is not relevant.
What is a patient in Medicare?
The term “patient” refers to a Medicare beneficiary.
How long does Medicare cover AWV?
Medicare covers an AWV for all patients who aren’t within 12 months after the eligibility date for their first Medicare Part B benefit period and who didn’t have an IPPE or an AWV within the past 12 months. Medicare pays for only 1 IPPE per patient per lifetime and 1 additional AWV per year thereafter.
How many times can you report ACP?
There are no limits on the number of times you can report ACP for a certain patient in a certain time period. When billing this patient service multiple times, document the change in the patient’s health status and/or wishes regarding their end-of-life care. Preparing Eligible Medicare Patients for the AWV.
Does Medicare cover EKG?
No. Medicare waives both the coinsurance/copayment and the Medicare Part B deductible for the IPPE (HCPCS code G0402). Neither is waived for the screening electrocardiogram (ECG/EKG) (HCPCS codes G0403, G0404, or G0405).
Is IPPE covered by Medicare?
The IPPE is an introduction to Medicare and covered benefits and focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV and perform such visits. The SSA explicitly prohibits Medicare coverage for routine physical examinations.
Does Medicare waive ACP deductible?
Medicare waives the ACP deductible and coinsurance once per year when billed with the AWV. If the AWV billed with ACP is denied for exceeding the once-per-year limit, Medicare will apply the ACP deductible and coinsurance. The deductible and coinsurance apply when you deliver the ACP outside of the covered AWV.
Do you have to report a diagnosis code for IPPE?
You must report a diagnosis code when submitting an IPPE claim. Medicare doesn’t require you to document a specific IPPE diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.