How do you Bill B12 injections?
Oct 03, 2018 · This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L33967 Vitamin B 12 Injections provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials. However, services performed for any given diagnosis must meet all of the indications and …
Where can you purchase B12 injections?
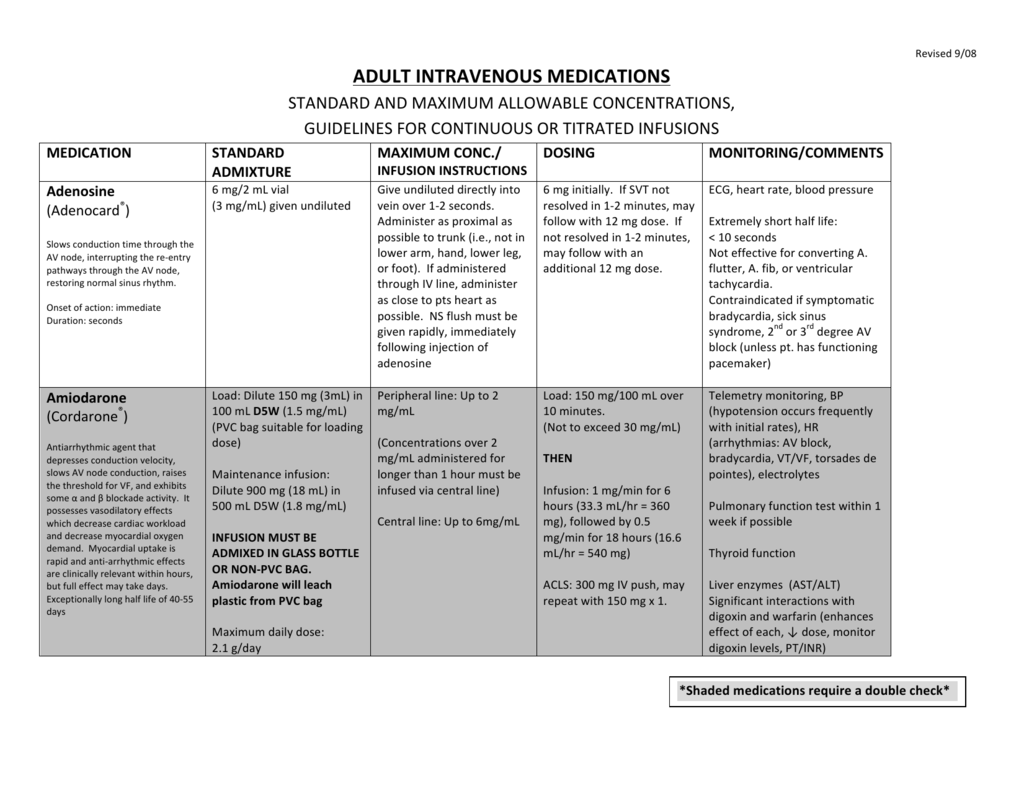
Jan 14, 2020 · It all depends on the circumstances. For the B12 injection, report the administration with 96372 (Therapeutic, prophylactic, or diagnostic injection [specify substance or drug]; subcutaneous or intramuscular). Include J3420 (Injection, vitamin B-12 cyanocobalamin, up to 1000 mcg) for the vitamin B-12 itself. Click to see full answer. Also know, how do you bill …
Is vitamin B12 covered by Medicare?
It is possible that Medicare benefits may be used to provide access to B12 shots through Part A and Part B under certain circumstances. If your Medicare-approved doctor determines that it is medically necessary to administer a B12 shot, it may be covered by Part B. If you have been formally admitted into a hospital, reside in a skilled nursing ...
Where to buy B12 shots?
Jun 23, 2016 · It has been my understanding that as long as a physician ordered something for a patient and there is documentation in the chart of that, ie shot of B12 or methotrexate for a diagnosed condition that is being followed by the MD, that it is perfectly acceptable for the nurse to give the injection and charge 99211 with the injection J code even if the MD is not present.
How do you bill a B12 injection?
What is the administration code for vitamin B12 injection?
What ICD 10 code covers vitamin B12 for Medicare?
When do you use CPT 96372?
Does Medicare cover vitamin B12 blood test?
What is the CPT code for Injection?
What DX code covers B12?
What ICD-10 covers B12 level?
D51. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM D51. 9 became effective on October 1, 2021.
What does CPT code 82607 mean?
How do I bill 96372 to Medicare?
How do you bill for injections?
Can you bill 96372 without an office visit?