
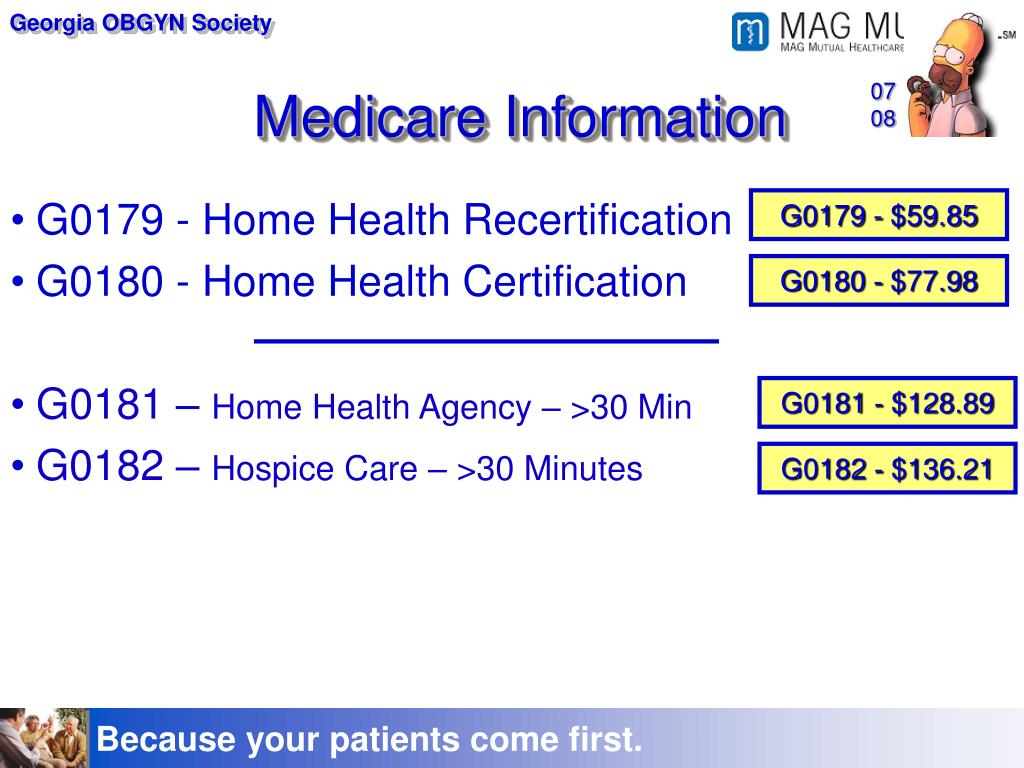
Bill using procedure codes G0179 or G0180. The place of service code should represent the place where the preponderance of the plan development and review was performed. Enter the provider number of the HHA from which the beneficiary is receiving Medicare-covered services in Item 23 of the CMS The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…Centers for Medicare and Medicaid Services
Full Answer
What is a g0180 form?
G0180 IS JUST FOR THE CERTIFICATION OF THE MEDICARE-COVERED HOME HEALTH SERVICES. Physicians may bill for the initial certification of Medicare-covered home health services.
What is the difference between HCPCS codes g0179 and g0180?
HCPCS code G0179 may be reported only once every 60 days, except in the rare situation when the patient starts a new episode before 60 days elapses and requires a new plan of care to start a new episode. Submit HCPCS code G0180 when the patient has not received Medicare covered home health services for at least 60 days.
What is physician re-certification (billing code g0179)?
Physician Re-Certification (Billing Code G0179) a. Physician re-certification is used when the physician signs the Plan of Care (Form 485) to re-certify a patient for home health services. A physician will re-certify a patient after a 60 day certification period.
How many times can you claim g0181?
G0181 : Home health care supervision (a minimum of 30 minutes per month required) The short description for G0179 is “MD recertification HHA PT” and can only be claimed once every 60 days unless the patient starts a new episode within 60 days, but this is rare. Otherwise, it is only used once per certification period.
Does Medicare pay for CPT G0180?
G0180 can only be billed if the provider certifies a patient to at least 60 days of home health care services. A patient receives G0180 certification has not received Medicare covered home health service for the minimum of 60 days.
How do I bill G0179 and G0180?
You may bill for codes G0179 and G0180 immediately following reviewing and signing a Cert or Recert of patient's Plan of Care. However, if a patient is readmitted to Home Health with a different Plan of Care during the same month as the original Cert or Recert, the physician can only bill once during that month.
Is G0180 a Medicare code?
The short description for G0180 is “MD certification HHA patient.” G0180 is used for the initial certification when the patient has not received Medicare-covered home health services for over 60 days. It also cannot be used along with the code G0181 on the same date of service.
What is the correct place of service for G0180?
Physician OfficeHence the Place of service code for Home Health Certification and Care Plan Oversight Services (G0179 place of service, G0180 place of service , G0181 and G0182) would be 11 (Physician Office).
How often are g0179 and G0180 billed?
once every 60 daysGuest. You can only bill these codes once every 60 days and at least 60 days from the previous dos.
What is billing code G0180?
G0180 - Physician or allowed practitioner certification for Medicare-covered home health services under a home health plan of care (patient not present), including contacts with home health agency and review of reports of patient status required by physicians to affirm the initial implementation of the plan of care ...
Does Medicaid pay for CPT G0180?
Expert. In North Carolina Medicaid will pay G0180 but ONLY if Medicare is primary and paid. (Sometimes Medicare doesn't pay if the patient is in a global period.) You are supposed to use either 99374 or 99375 for billing to Mediciad or commercial insurances but those codes are time-based.
Who can bill G0182?
G0182 Physician supervision of a patient under a Medicare-approved hospice (patient not present) requiring complex and multidisciplinary care modalities involving regular physician development and/or revision of care plans, review of subsequent reports of patient status, review of laboratory and other studies, ...
How do I bill a Medicare oversight plan?
The care plan oversight services are billed using Form CMS-1500 or electronic equivalent. Submit HCPCS code G0180 when the patient has not received Medicare covered home health services for at least 60 days.
What date of service should be used for G0180?
Date of service for HCPCS codes G0179 and G0180 must be submitted as the date physician/NPP saw the patient, not the date the physician/NPP signed the certification or recertification.
What is G0180 service date?
The home health agency certification code (G0180) is valid when the patient begins a new episode of home health care. A new episode of care begins after the patient has not received Medicare-covered home health (HH) services for at least 60 days.
Can you bill TCM and E&M together?
A7: Yes, for an E/M visit you can bill additional visits other than the one bundled E/M visit in the TCM.
When to submit HCPCS code G0180?
Submit HCPCS code G0180 when the patient has not received Medicare covered home health services for at least 60 days. The initial certification (HCPCS code G0180) cannot be filed on the same date of service as the supervision service HCPCS codes (G0181 or G0182). HCPCS Codes.
How often do you report HCPCS code G0179?
HCPCS code G0179 may be reported only once every 60 days, except in the rare situation when the patient starts a new episode before 60 days elapses and requires a new plan of care to start a new episode. Submit HCPCS code G0180 when the patient has not received Medicare covered home health services for at least 60 days.
Does Medicare pay for home health care?
Medicare does not pay for care plan oversight services for nursing facility or skilled nursing facility patients. Separate payment is allowed for the services involved in physician certification/re-certification and development of a plan of care for Medicare covered home health services.
Can you file HCPCS code G0180 on the same date?
The initial certification (HCPCS code G0180) cannot be filed on the same date of service as the supervision service HCPCS codes (G0181 or G0182). Submit CPT codes 99201-99263 and 99281-99357 only when there has been a face-to-face meeting/encounter.
What is the role of a physician in Medicare?
Physician play a key role in documenting eligibility and medical necessity for home health care for Medicare beneficiaries. If you certify the need for home health care for any of your patients, we encourage you to review this article carefully. As a physician, you are responsible for providing appropriate, accurate supporting documentation of your face-to-face (FTF) encounters with your patients regarding home health care and certification of need. Medicare provides payment for physician initial and re-certification of Medicare-covered home health services under a home health plan of care (G0180 and G0179).
Does Medicare cover home health?
Medicare provides payment for physician initial and re-certification of Medicare-covered home health services under a home health plan of care (G0180 and G0179). The attending provider (not staff) must perform these services. The medical record must document the medical necessity as well as the level of service.
What is a G0179?
G0179 - Physician re-certification for Medicare-covered home health services under a home health plan of care (patient not present), including contacts with home health agency and review of reports of patient status required by physicians to affirm the initial implementation of the plan of care that meets patient’s needs, per re-certification period
How long is a home health provider billed?
This may be billed when the patient has not received Medicare-covered home health services for at least 60 days. Physician or allowed practitioner services for recertification ...
How many days can a physician bill for HHA?
Only one physician or allowed practitioner may bill for services for certification of Medicare-covered HHA services for a beneficiary, in a 60-day period. All other claims will be denied. Recertification services reported in excess of one per 60 days when a new plan of care is not required (e.g., patient condition worsens requiring new care plan) ...
How often do you have to recertify for Medicare?
Physician or allowed practitioner services for recertification of Medicare-covered home health services may be billed after a patient has received services for at least 60 days when the physician or allowed practitioner signs the certification after the initial certification period. This recertification may be reported only once every 60 days, ...
What elements should be evident in the medical record for Medicare home health services?
Since the certification and recertification of Medicare-covered home health services include either the creation of a new or review of an existing plan of care, the following elements should be evident in the medical record: Patient’s mental status. Types of services, supplies, and equipment required.
Is physician recertification necessary for Medicare?
Physician certification and recertification will be considered medically reasonable and necessary for a patient receiving Medicare-covered home health services requiring the development of a plan of care by the physician when the following conditions are met:
Can a physician be reimbursed for home health services?
Physician or allowed practitioner services involving certification and recertification of Medicare-covered home health services may be separately coded and reimbursed. These services include creation and review of a plan of care, and verification that the home health agency initially complies with the practitioner's plan of care.
How long does a CPT 99490 bill take?
The service period for CPT 99490 is one calendar month, and CMS expects the billing practitioner to continue furnishing services during a given month as applicable after the 20 minute time threshold to bill the service is met (see #3 above). However practitioners may bill the PFS at the conclusion of the service period or after completion of at least 20 minutes of qualifying services for the service period. When the 20 minute threshold to bill is met, the practitioner may choose that date as the date of service, and need not hold the claim until the end of the month.
When is CPT 99490 billed?
CPT 99490 can be billed if the beneficiary dies during the service period, as long as at least 20 minutes of qualifying services were furnished during that calendar month and all other billing requirements are met.
What is provider based outpatient?
provider-based outpatient department of a hospital is part of the hospital and therefore may bill for CCM services furnished to eligible patients, provided that it meets all applicable requirements. A hospital-owned practice that is not provider-based to a hospital is not part of the hospital and, therefore, not eligible to bill for services under the OPPS; but the physician (or other qualifying practitioner) practicing in the hospital-owned practice may bill under the PFS for CCM services furnished to eligible patients, provided all PFS billing requirements are met.
What is CPT 99490?
CPT 99490 describes activities that are not typically or ordinarily furnished face-to-face, such as telephone communication, review of medical records and test results, and consultation and exchange of health information with other providers. If these activities are occasionally provided by clinical staff face-to-face with the patient but would ordinarily be furnished non-face-to-face, the time may be counted towards the 20 minute minimum to bill CPT 99490. However, see #12 below regarding care coordination services furnished on the same day as an E/M visit.
What is Medicare outpatient?
Per section 20.2 of publication 100-04 of the Medicare Claims Processing Manual, a hospital outpatient is a person who has not been admitted by the hospital as an inpatient but is registered on the hospital records as an outpatient and receives services (rather than supplies alone) from the hospital. Since CPT code 99490 will ordinarily be performed non face-to-face (see # 11 above), the patient will typically not be a registered outpatient when receiving the service. In order to bill for the service, the hospital’s clinical staff must provide at least 20 minutes of CCM services under the direction of the billing physician or practitioner. Because the beneficiary has a direct relationship with the billing physician or practitioner directing the CCM service, we would expect a beneficiary to be informed that the hospital would be performing care management services under their physician or other practitioner’s direction.
How many times can you bill Medicare for E/M?
Under longstanding Medicare guidance, only one E/M service can be billed per day unless the conditions are met for use of modifier -25. Time cannot be counted twice, whether it is face-to-face or non-face-to-face time, and Medicare and CPT specify certain codes that cannot be billed for the same service period as CPT 99490 (see #13, 14 below). Face-to-face time that would otherwise be considered part of the E/M service that was furnished cannot be counted towards CPT 99490. Time spent by clinical staff providing non-face-to-face services within the scope of the CCM service can be counted towards CPT 99490. If both an E/M and the CCM code are billed on the same day, modifier -25 must be reported on the CCM claim.
Do you need to change billing practitioners for PFS?
No, as provided in the CY 2014 PFS final rule (78 FR 74424), a new consent is only required if the patient changes billing practitioners, in which case a new consent must be obtained and documented by the new billing practitioner prior to furnishing the service.
When will Medicare start certifying home health services?
These changes are effective for Medicare claims with a date on or after March 1, 2020. Previously, only physicians were allowed to do so.
How long does it take to recertify a HHA?
The initial certification period lasts 60 days. Near the end of this initial period, the physician or allowed practitioner must decide whether to recertify the patient for a subsequent 60-day certification period. Recertification is required at least every 60 days unless the patient elects to transfer services to another HHA. There’s no need to recertify if discharge goals are met or if there’s no expectation that the patient will return to home health care. Medicare doesn’t limit the number of continuous 60-day recertification periods for patients who continue to be eligible for the home health benefit.
What is PDGM in home health?
In November 2018, CMS finalized the Patient Driven Groupings Model (PDGM) case-mix adjustment payment model effective for home health periods of care beginning on or after January 1, 2020. Medicare now pays HHAs a national, standardized rate based on a 30-day period of care. The PDGM case-mix method adjusts this rate based on clinical characteristics of the patient and their resource needs. Some of this information is found on the Medicare claims and some from certain Outcome and Assessment Information Set (OASIS) items. Medicare also uses a wage index to adjust the payment rate to reflect differences in wages between geographical areas. There are no changes to timeframes for recertifying eligibility and reviewing the home health plan of care, both of which will occur every 60 days (or in the case of updates to the plan of care, more often as the patient’s condition warrants).
