
Per CPT guidelines, physicians consulting for patients in observation should bill the outpatient consult code (99242) and subsequent observation care codes (99224-99226) for additional visits. For Medicare, and other payers that do not accept consultation codes, the outpatient codes 99201-99215 should be billed instead.
How does Medicare pay for hospital observation?
Medicare Advantage (Part C) plans may also cover observation in a hospital if it’s ordered by your doctor. Medicare Advantage plans also include an annual out-of-pocket spending limit, which can potentially save you money in Medicare costs for your observation services. Original Medicare does not include an out-of-pocket spending limit.
What determines observation vs inpatient?
Inpatient status means that if you have serious medical problems that require highly technical skilled care. Observation status means that have a condition that healthcare providers want to monitor to see if you require inpatient admission.
How to use the new Medicare outpatient observation notice?
than 24 hours. Notice of non-inpatient status must be provided within 36 hours. CMS requires hospitals to use a standardized notice that it drafted, known as the Medicare Outpatient Observation Notice (MOON). After a space for the patient’s name and Medicare number, the
What is observation status under Medicare?
defined as the following: Under Medicare payment policy, observation status is considered an outpatient service. As such it is billed under Medicare Part B, which covers physician visits, outpatient services and home healthcare. Patients hospitalized under observation can encounter significant financial burdens because Medicare Part B may carry
How do you bill for consult on observation patient?
Other physicians who provide services to your patients should use office visit or outpatient consult codes. If you ask another physician to see your patient during his or her observation stay, that physician should use office or outpatient visit codes 99201-99215 or outpatient consult codes 99241-99245.
Does Medicare pay for under observation stay in hospital?
Key takeaways. Medicare Part B – rather than Part A – will cover your hospital stay if you're assigned observation status instead of being admitted.
Does Medicare accept observation codes?
Same-day observation admit/discharge codes 99234-99236 for Medicare patients must include a minimum stay of at least 8 hours. For duration of less than 8 hours on the same date, the Initial observation code series 99218-99220 are used for Medicare patients.
What is the CPT code for hospital observation?
99234-99236Observation or Inpatient Hospital Care (including admission and discharge) CPT codes 99234-99236 are used to report observation or initial hospital services for a patient that is admitted and discharged on the same date of service.
How does Medicare reimburse for observation?
Does Medicare Pay for Observation Services? Medicare considers observation care an outpatient service. Outpatient services are covered under Medicare Part B, which means that patients on observation status have fewer Medicare benefits and will pay more out of pocket.
What is the reimbursement that Medicare uses for observation services?
Observation services are reimbursed under the Outpatient Prospective Payment System using the CMS-1500 as an alternative to inpatient admission. To report more than six procedures or services for the same date of service, it is necessary to include a letter of explanation.
What type of bill is used for an observation claim?
Therefore, hospitals should bill HCPCS code G0378 when observation services are provided to any patient in “observation status,” regardless of the patient's condition.
What criteria must be met to bill a Medicare patient as an inpatient observation patient?
For a physician to bill observation care codes, there must be a medical observation record for the patient which contains dated and timed physician's orders regarding the observation services the patient is to receive, nursing notes, and progress notes prepared by the physician while the patient received observation ...
How does Medicare explain outpatient observation Notice?
The notice must explain the reason that the patient is an outpatient (and not an admitted inpatient) and describe the implications of that status both for cost-sharing in the hospital and for subsequent “eligibility for coverage” in a skilled nursing facility (SNF).
What is the CPT code for a 23 hour observation?
23-hour observation stay According to CPT, 99218–99220 plus 99217 are for admission and discharge on two separates dates of service, and 99234–99236 are for admission and discharge on the same date of service.
How are observation hours calculated?
Observation time begins at the clock time documented in the patient's medical record, which coincides with the time that observation care is initiated in accordance with a physician's order. Observation time ends when all medically necessary services related to observation care are completed.
How do you bill observation less than 8 hours?
If a patient is in observation for less than eight hours on one calendar day, you would bill initial observation care codes (99218–99220).
What is a medical expert request?
A request (verbal or written) from the referring physician. The specific opinion or recommendations of the consulting physician. A written report of each service performed or ordered on the advice of the consulting physician. The medical expertise requested is beyond the specialty of the requesting physician.
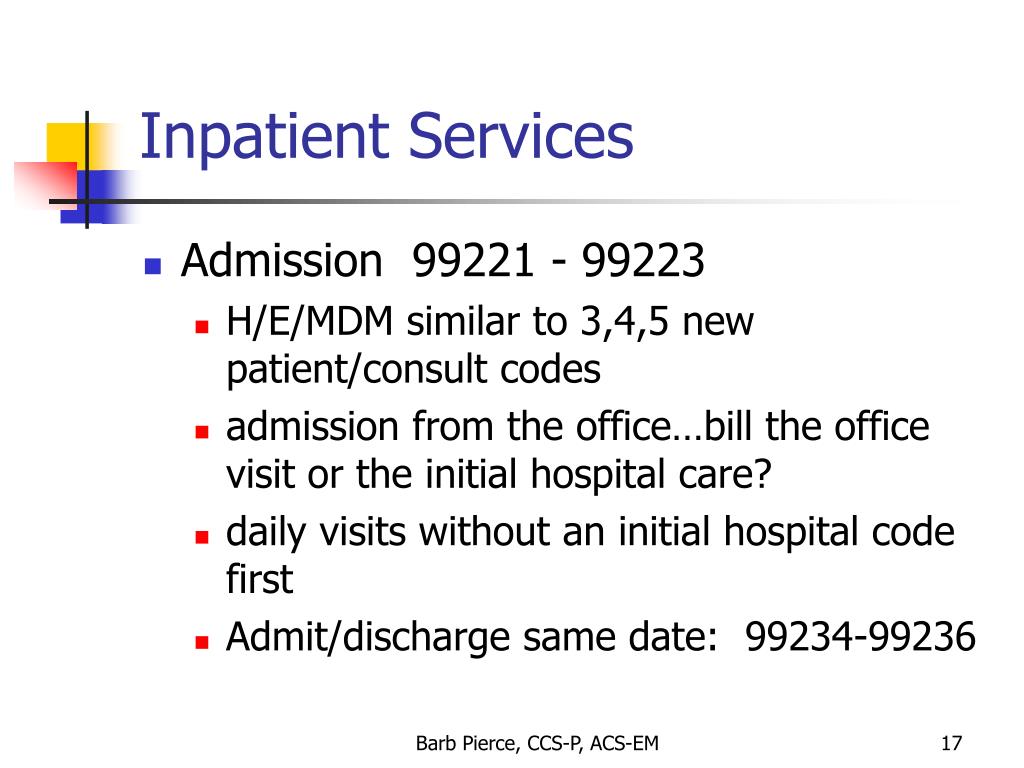
Is an office admission considered part of the initial hospital care?
All services performed in an office and the resulting hospital admission are reflected (i.e., admission following any evaluation and management (E/M) services received by the patient in an office, emergency room, or nursing facility). If these services are on the same date as admission, they are considered part of the initial hospital care.
Does Medicare recognize new or established billing codes?
Second, the old initial consultation codes (99251-99255) are no longer recognized by Medicare Part B, although many non-Medicare providers still use them if ...
What is the code for a hospital consultation?
Inpatient consultations should be reported using the Initial Hospital Care code (99221-99223) for the initial evaluation, and a Subsequent Hospital Care code (99231-99233) for subsequent visits. In some cases, the service the physician provides may not meet the documentation requirements for the lowest level initial hospital visit (99221).
What is the code for ED visit?
The ED physician evaluates the patient and codes an ED visit (99281-99285). He also requests a consult from a cardiologist. The cardiologist evaluates the patient and decides to admit him. The admitting cardiologist would report an initial hospital visit (99221-99223) with modifier AI appended.
Why would an endocrinologist not append modifier AI?
But, the endocrinologist would not append modifier AI because he is not the admitting physician overseeing the patient’s overall care. Per CMS guidelines, “In all cases, physicians will bill the available code that most appropriately describes the level of the services provided.”.
Does Medicare accept 99241?
Consultation Coding for Medicare. Medicare does not accept claims for either outpatient (99241-99245) or inpatient (99251-99255) consultations, and instead requires that services be billed with the most appropriate (non-consultation) E/M code.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
Medicare rules and regulations regarding acute care inpatient, observation and treatment room services are outlined in the Medicare Internet-Only Manuals (IOMs).
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the Medicare outpatient consult code?
If he was called in to consult, he could bill an outpatient consult code (99241-99245) if the patient is not covered by Medicare or an outpatient visit code (99201-99215) for a Medicare patient.
When to use 99234-99236?
You recommended billing the service with a 99234-99236 (observation, admit and discharge on the same date) and using only the date of day 2 as the service date.
What is CPT 99234?
The bulletin states: “NAS recommends the use of CPT 99234-99236 (observation or inpatient care services including admission and discharge services) if the patient is seen on at least two separate occasions on day 2 and these separate occasions are at least 8 hours apart.”. Inpatient to observation status.
What happens if you bill with same day admit code?
If you bill with a same-day admit/discharge code and the claim is denied because of a conflicting initial date of service, submit your documentation that the date of service you billed for was the date the physician actually saw the patient. As for needing to see a patient twice on the same day to bill 99234-99236, ...
Can a resident's note stand on its own?
As you know, residents’ notes can’t stand on their own, but must be supported with attending documentation. But this scenario isn’t necessarily resident-specific. Sometimes, patients may be admitted to observation (with no resident involvement) but not seen by a physician until the next calendar day.
How long does a patient have to wait to receive an observation notice from Medicare?
All patients receiving services in hospitals and clinical access hospitals (CAHs) must receive a Medicare outpatient observation notice (MOON) no later than 36 hours after observation services as an outpatient begin. The MOON informs patients, who receive observation services for more than 24 hours, of the following:
How many hours of observation should be billed?
Should be billed according to observation billing guidelines. All hours of observation up to 72 hours should be submitted on a single line. The date of service being the date the order for observation was written. Orders for observation services are not considered to be valid inpatient admission levels of care orders.
What is an inpatient admission?
An order simply documented as “admit” will be treated as an inpatient admission. A clearly worded order such as “inpatient admission” or “place patient in outpatient observation” will ensure appropriate patient care and prevent hospital billing errors.
What is an observation status?
Observation status. Outpatient; released when the physician determines observation is no longer medically necessary. Physician’s order is required. Lack of documentation can lead to claim errors and payment retractions. An order simply documented as “admit” will be treated as an inpatient admission.
How long after observation can you get a moon?
Hospitals and CAHs may deliver the MOON to a patient receiving observation services as an outpatient before the patient has received more than 24 hours of observation services but no later than 36 hours after observation services begin.
What is outpatient observation?
Outpatient observation services are covered only when provided by order of a physician or another individual authorized by state licensure and hospital staff bylaws to admit patients to the hospital or to order outpatient tests. Do not order observation services for a future elective surgery or outpatient surgery cases.
When is observation not considered medically necessary?
Observation services are not considered medically necessary when the patient’s current medical condition does not warrant observation, or when there is not an expectation of significant deterioration in the patient’s medical condition in the near future.
Can you bill for the first day only if only the resident saw the patient?
The answer is yes: You must base your claim on the supervising physician’s date of service, so you can’t bill for the first day when only the resident saw the patient. In this case, day 2 would be considered the only date of service.
Can observation services be paid?
Who can bill? Observation services provided for the convenience of the patient, the patient’s family or the physician are not considered reasonable or necessary and, therefore, won’t be paid.
Is observation off limits after surgery?
Also off limits: observation services for routine stays after surgery or after diagnostic tests or outpatient procedures done in the hospital—unless a physician documents that a patient’s condition is unstable. In that case, observation care would be warranted.
Can you bill for hospital admissions on a per diem basis?
Hospital services are paid on a “per diem” basis, so you can bill only an initial inpatient admission code (99221–99223) on the date of admission. That would be true even if you performed a subsequent observation service for that patient on the second calendar date.
Does Medicare see a single physician?
Medicare isn’ t clear on this, but the Centers for Medicare and Medicaid Services (CMS) does view physicians in the same practice and of the same specialty as a single physician.
Can you bill for observation discharge the same day?
And when a patient is admit ted to the hospital, you cannot bill for an observation discharge that same calendar day.
