You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the providers bill or invoice to your regional Medicare Administrative Contractor. Keep copies of everything you submit.
Full Answer
What information do I need to bill for Medicare?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes.
How does the process of Medicare billing work?
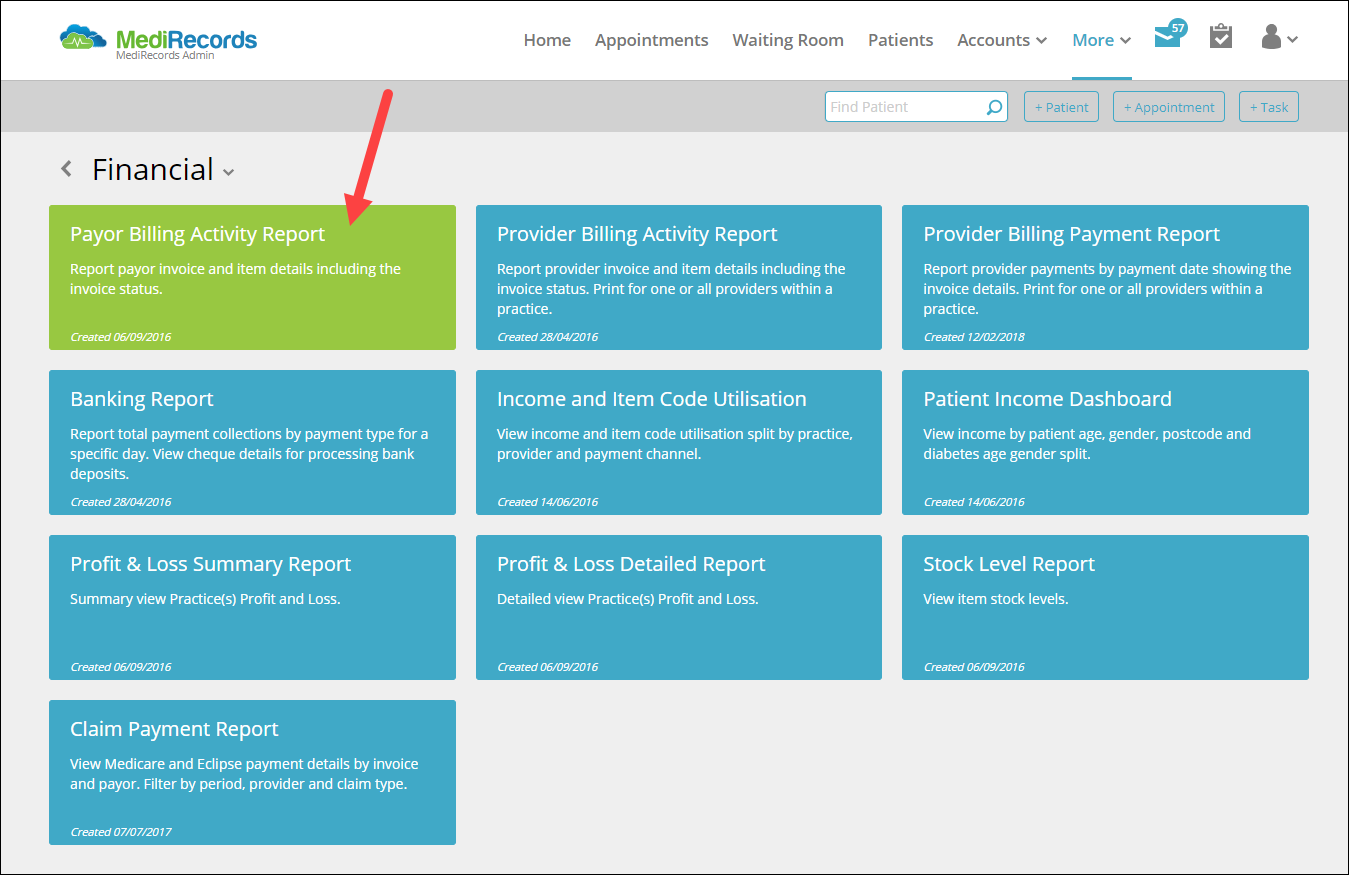
Billing for Medicare Before we get into specifics with Medicare, here’s a quick note on the administrative process involved. When a claim is sent to Medicare, it’s processed by a Medicare Administrative Contractor (MAC). The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim.
Do I need a manual form to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500.
Why do billers send claims directly to Medicare and Medicaid?
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
How do I bill a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Can you bill Medicare directly?
In short, providers may not bill Medicare for noncovered services, but, provided the patient has been informed that the service is not covered and still requests the service, the patient can be billed directly and will be personally responsible.
What is the KX modifier for Medicare?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
How do I bill Medicare Part B?
Talk to someone about your premium bill For specific Medicare billing questions: Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. For questions about your Part A or Part B coverage: Call Social Security at 1-800-772-1213. TTY: 1-800-325-0778.
Can you bill a Medicare patient for a non covered service without an ABN?
Medicare requires an ABN be signed by the patient prior to beginning the procedure before you can bill the patient for a service Medicare denies as investigational or not medically necessary. Otherwise, Medicare assumes the patient did not know and prohibits the patient from being liable for the service.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is the KF modifier used for?
Although not associated with a specific , the KF modifier is required for claim submission of this HCPCS code as well. This information will be added to the applicable -related Policy Articles in an upcoming revision....Publication History.Publication DateDescription08/29/19Originally PublishedFeb 19, 2020
What is KY modifier used for?
The KY Modifier is used to identify a wheelchair accessory that is for use with a base that was not part of the competitive bid program. This modifier is only for use in former competitive bid areas and is important to ensure appropriate pricing on the wheelchair accessories.
Is KX modifier for Medicare only?
Therapists should continue to affix the KX modifier to all medically necessary services above the designated limit ($2,010 in 2018), thus signaling Medicare to pay the claim. That means you must continue to track your patients' progress toward the threshold so you know when to affix the modifier.
Can I submit a paper claim to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
Does Medicare accept secondary paper claims?
Currently, Medicare does not accept electronically filed claims when there is more than one payer primary to Medicare. Claims that involve more than one primary payer to Medicare must be submitted on the 1500 paper claim form, with all appropriate attachments.
What are Medicare Part B payments based on and how is the allowable charge calculated?
What are the Medicare Part B payments based on, and how is the allowable charge calculated? It is based on diagnosis- related group (DRG's), they determine appropriate reimbursement.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is Medicaid the last payer to be billed?
One final note: Medicaid is the last payer to be billed for a service. That is, if a payer has an insurance plan, that plan should be billed before Medicaid. In general, it’s much too difficult to describe the full process of billing Medicaid without going into an in-depth description of specific state programs.
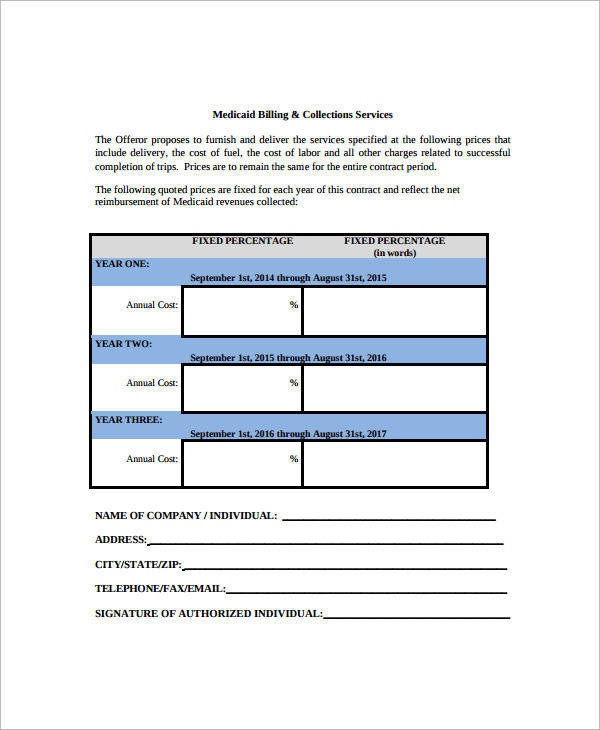
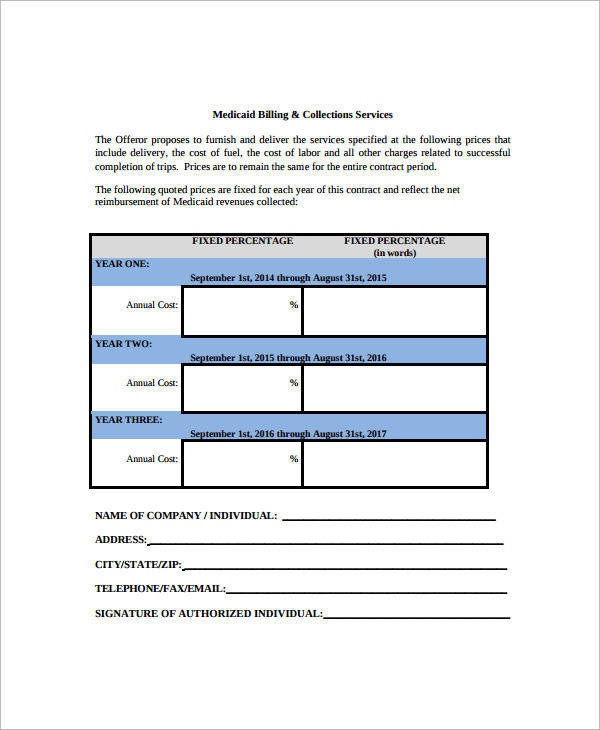
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
What Information Do You Need To Fill Out This Form
Medicare will need you to fill out a patient request form with some basic information about yourself as well as the service or medical item you are filing about. Youll need to provide:
Find Cheap Medicare Plans In Your Area
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.
Medicare Claims And Reimbursement
In most cases, you wont have to worry about filing Medicare claims. Here are some situations where you might or might not need to get involved in the claim process.
What Do I Do If My Doctor Does Not Accept Medicare
You can choose to stay and cover the costs out-of-pocket, but this is not an affordable option for most Americans. Instead, you can ask your doctor for a referral to another healthcare provider that does accept Medicare, do your own research, or visit an urgent care facility. Most urgent care offices accept Medicare.
How Long Do I Have To File A Claim
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
You Should Only Need To File A Claim In Very Rare Cases
Medicare claims must be filed no later than 12 months after the date when the services were provided. If a claim isn’t filed within this time limit, Medicare can’t pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How Do I File A Medicare Claim
Medicare beneficiaries occasionally have to submit their own healthcare claims instead of relying on a provider to submit them. | Photo credit: Helloquence | Unsplash
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Avoiding Denials on Priced Per Invoice Claims
Procedure codes that require pricing per invoice, must contain the below elements in Item 19 of the CMS-1500 claim form or its electronic equivalent for each line item submitted.
Procedure Codes that Require a Description and an Invoice
Providers must maintain an invoice copy in the patient's file and it must be made available to Noridian upon request.
What is CMS in Medicare?
CMS, the Centers for Medicare and Medicaid Services, governs all parts of Medicare, including Part B. CMS holds a great amount of influence over the way insurance companies pay doctors, as well as the services that doctors provide. This is, in large part, because of Medicare Part B restrictions. Every type of healthcare service eligible ...
How long does it take for Medicare to pay Part B?
Like other commercial insurances, you should send Medicare Part B claims directly to Medicare for payment, with an expected turnaround of about 30 days. Unlike typical commercial insurance, Medicare can pay either the provider or the patient, depending on the assignment.
What is Medicare Part B for eyeglasses?
Other preventative services are also covered under Medicare Part B: Preventive shots, including the flu shot during flu season, and three Hepatitis B shots, if you're considered at risk.
Why is Medicare important?
Because Medicare is a service provided for the elderly, disabled, and retired, the patients who are covered by Medicare will usually have limited financial resources . Because of this, it's very important to make sure that your office bills and codes within all Part B guidelines and provides only approved Part B services.
What is medically necessary?
Medically Necessary Services: These include services and supplies needed to treat your medical condition. To be covered, the service also has to be within the standards of medical practice. This means that holistic or naturopathic treatments wouldn't be covered.
What are the services that are considered medically necessary?
These services include: Home health services, only when they are medically necessary, and of limited duration. Chiropractic services, only if it is to correct spinal subluxation. Ambulance services, only if a different type of transportation would endanger the patient's health.
Is it important to understand the limitations of Medicare?
No matter what type of insurance a patient has, it's important to understand the limitations you may have because of their insurance coverage. The same goes for Medicare Part B billing. But in this case keeping in mind the rules, regulations, and guidelines is especially relevant.
How Do I Pay My Premium?
For Part B, your premium will be taken out of your Social Security check once you start collecting on Social Security. Before that time, or if you don’t qualify for Social Security, you can pay your Part B premium online using a debit card, credit card, or a connected bank account.
What To Do If There Is A Medicare Billing Error, Or You Suspect One Occurred
Billions of dollars move around the government, hospitals, and the population’s collective pockets every year for Medicare coverage. Billing issues can arise from all this money moving hands. In fact, a 2017 report said that there were about $36 billion worth of billing errors that year.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining ...
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…