What is Medicare conditional billing?
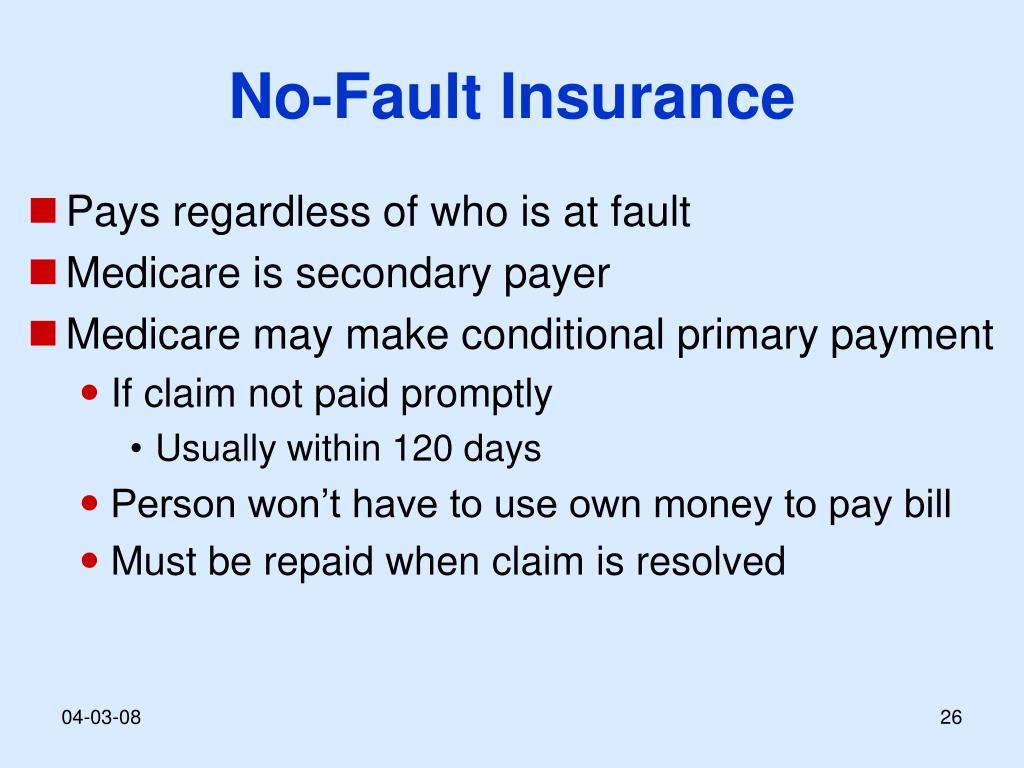
• A conditional payment is a payment that Medicare makes. for services where another payer may be responsible. This. conditional payment is made so that the Medicare beneficiary won't have to use their own money to pay the bill.
How do I file a Medicare conditional payment?
You can obtain the current conditional payment amount and copies of CPLs from the BCRC or from the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627.
When would Medicare make a conditional payment to a beneficiary?
MSP provisions allow conditional payments in certain situations when the primary payer has not paid or is not expected to pay within 120 days after receipt of the claim for specific items and/or services. Medicare makes these payments “on condition” that it will be reimbursed if it is shown another payer is primary.
How do you fill out CMS 1500 when Medicare is secondary?
0:239:21Medicare Secondary Payer (MSP) CMS-1500 Submission - YouTubeYouTubeStart of suggested clipEnd of suggested clipHere when the insured. And the patient are the same the biller enters the word. Same if medicare isMoreHere when the insured. And the patient are the same the biller enters the word. Same if medicare is primary this item is left blank.
Do I have to pay back conditional payments?
If you continue to certify for benefits while we review, you may have to pay back any conditional payments you received if we later find you ineligible.
What is a CMS Lien?
A Medicare lien results when Medicare makes a “conditional payment” for healthcare, even though a liability claim is in process that could eventually result in payment for the same care, as is the case with many asbestos-related illnesses.
What is a conditional claim?
Conditional (or “contingent”) claim limitations recite a step or function that is only performed upon the satisfaction of some condition. In a method claim, a conditional limitation might follow the structure, “if A, then B,” reciting that the step B is performed if the condition A occurs.
How does Medicare calculate final demand?
Step number two: take the gross settlement amount and subtract the total procurement cost to determine Medicare's final lien demand.
What is a Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.
How does Medicare calculate secondary payment?
As secondary payer, Medicare pays the lowest of the following amounts: (1) Excess of actual charge minus the primary payment: $175−120 = $55. (2) Amount Medicare would pay if the services were not covered by a primary payer: . 80 × $125 = $100.
What goes on box 24c on CMS-1500?
24c. EMG-Emergency Enter a Y in the unshaded area of the field. If this is not an emergency, leave this field blank.
What goes in box 24c on HCFA?
Box 24c. EMG indicator (also called emergency indicator) is a carryover from the older CMS-1500 form and is unlikely to be required on current claims. If needed, however, you can add the 'EMG' field via the service line Column Chooser.
Why is Medicare considered a conditional payment?
Medicare may make a conditional payment when there is evidence that payment has not been made or cannot reasonably be expected to be made promptly by workers’ compensation, liability insurance (including self-insurance), or no-fault insurance. These payments are referred to as conditional payments because the money must be repaid to Medicare ...
What is prompt payment for Medicare?
These payments are referred to as conditional payments because the money must be repaid to Medicare when a settlement, judgment, award, or other payment is secured. Prompt or promptly means: Liability insurance (including self-insurance) Payment within 120 days after the earlier of the following: Date a general liability claim is filed ...
How long does it take to get Medicare after a car accident?
No-fault and workers' compensation. Payment within 120 days after receipt of the claim. After the 120-day period, you may bill Medicare conditionally. Note: If an injury resulted from an automobile accident and/or there is an indication ...
What is conditional payment?
Conditional payment. A provider may submit a claim to Medicare for conditional payment for services for which another payer is responsible. If payment has not been made or cannot be expected to be made promptly from the other payer, Medicare may make a conditional payment, under some circumstances, subject to Medicare payment rules.
Does Medicare pay workers compensation?
The primary insurer denied the claims in full or when the claim was fully applied to deductible or coinsurance. Medicare will not make conditional payments associated with Workers' Compensation Medicare Set Aside or for an Ongoing Responsibilities for Medicals under auto/no-fault, liability, or workers' compensation.
Does Medicare deny a conditional claim?
Medicare will deny claims submitted for conditional payment when the provider submits the claim to the liability, no-fault, or WC claims and payment is denied if: There is an employer GHP that is primary to Medicare; and. You did not send the claim to the employer GHP first.
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
Who has the right to appeal a demand letter?
This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the right to appeal.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.