
Billing Claims Submit a completed hardcopy red and white UB04 form. Ensure you are obtaining the beneficiary's Medicare Beneficiary Identification (MBI) card and asking about any other applicable insurance.
How does Medicare affect medical billing?
Obamacare’s Affect on Medical Billing and Coding
- Increased Demand for Work. One of the undeniable facts about Obamacare is that more Americans will have health insurance, which means that demand for coding and billing professionals is bound ...
- Cumbersome Government-Related Processing Issues. ...
- Increased Medicare Efficiency. ...
- Job Outlook. ...
Is there a deductible for Medicare Part?
The Medicare Part A deductible for inpatient hospital services will increase by $72 in calendar year 2022, to $1,556, the Centers for Medicare & Medicaid Services announced Friday.
How to file your claims with Medicare?
- The date of your treatment
- Where you received treatment (hospital, doctor’s office, etc.)
- Description of each treatment or medical supply received
- Itemized charge (s) for each treatment or medical supply
What are the requirements for Medicare billing?
- The regular physician is unavailable to provide the service.
- The beneficiary has arranged or seeks to receive the services from the regular physician.
- The locum tenens is NOT an employee of the regular physician.
- The regular physician pays the locum tenens physician on a per diem or fee-for-service basis.
How are Medicare Part A claims paid?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What claim form is used for Medicare Part A?
Form CMS-1500The Form CMS-1500 is the standard paper claim form used by health care professionals and suppliers to bill Medicare Carriers or Part A/B and Durable Medical Equipment Medicare Administrative Contractors (A/B MACs and DME MACs).
Who pays Medicare Part A claims?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
What is the difference between UB-04 and CMS-1500?
The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities. This would include things like surgery, radiology, laboratory, or other facility services. The HCFA-1500 form (CMS-1500) is used to submit charges covered under Medicare Part B.
What is a CMS-1500 claim form used for?
The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of ...
What criteria must be met to bill a Medicare patient as an inpatient?
An inpatient admission is generally appropriate for payment under Medicare Part A when you're expected to need 2 or more midnights of medically necessary hospital care, but your doctor must order this admission and the hospital must formally admit you for you to become an inpatient.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
How do providers bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
How do I get reimbursed from Medicare?
How to Get Reimbursed From Medicare. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out.
How do I complete CMS 1500?
2:3419:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipNumber fields 2 & 5 capture patient name and address and must be completed. The only optional fieldMoreNumber fields 2 & 5 capture patient name and address and must be completed. The only optional field is telephone number fields 4 & 7 will contain the same name and address as fields 2 & 5 although.
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
How long does it take to see a Medicare claim?
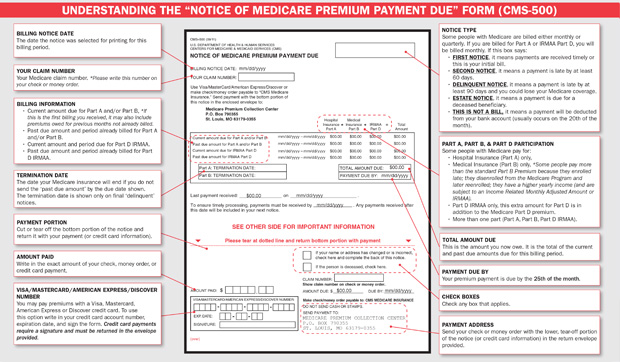
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is a PACE plan?
PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. claims: Contact your plan.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
What is a consolidated billing for SNF?
Effective January 1, 2005, section 410 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) amended the SNF consolidated billing law to specify that when a SNF’s Part A resident receives the services of a physician (or another type of practitioner that the law identifies as being excluded from SNF consolidated billing) from a RHC or a FQHC, those services are not subject to CB merely by virtue of being furnished under the auspices of the RHC or FQHC. Accordingly, under section 410 of the MMA, services otherwise included within the scope of RHC and FQHC services that are also described in clause (ii) of section 1888(e)(2)(A) are excluded from consolidated billing, effective with services furnished on or after January 1, 2005. Only this subset of RHC/FQHC services may be covered and paid separately when furnished to SNF residents during a covered Part A stay (see the regulations at 42 CFR 411.15(p)(2)(xvii) and 405.2411(b)(2)). Use TOBs 71x and 73x, respectively, to bill for these RHC/FQHC services. See Pub. 100-02, Medicare Benefit Policy Manual, chapter 13 for additional information on Part B coverage of RHC/FQHC services.
How long does a beneficiary have to transfer to a second SNF?
It is certainly possible that a beneficiary may remain at a facility under sanction for a period of time and later transfer to a second SNF. The 30-day transfer requirement will be applied in the same way it would be for a beneficiary transferring between two SNFs that are not under sanction. Part A coverage will be available to the second SNF for all remaining days in the benefit period as long as the beneficiary:
What is the revenue code for SNF?
The SNF Pricer shall calculate the rate for each line item with revenue code 0022 on a SNF claim. The SNF Pricer shall determine the rate using the following information:
Can SNF bill accommodation charges?
The SNF must not put accommodation charges incurred in different accounting years on the same bill. (See §40.3.5.1 when billing for ancillary charges for services furnished on the day of discharge or death when it is also the day after the end of the accounting year.) At the end of the accounting year, the SNF must submit a bill that contains the charges for all services furnished to the patient since the last bill and through the end of that year. The SNF shows services furnished in the following accounting year on a separate bill.
Can a provider furnish a covered item?
provider may have others furnish certain covered items and services to their patients through arrangements under which receipt of payment by the provider for the services discharges the liability of the beneficiary or any other person to pay for the service. In permitting providers to furnish services under arrangements, it is not intended that the provider merely serve as a billing mechanism for the other party. Accordingly, for services provided under arrangements to be covered, the provider must exercise professional responsibility over the arranged-for services. See the Medicare General Information, Eligibility, and Entitlement Manual, Chapter 5, “Definitions,” §10.3, for additional discussion on services furnished under arrangement.
Does Medicare coordinate care require consolidated billing?
Services for beneficiaries covered under the Medicare Coordinated Care Demonstration will not be subject to consolidated billing. Common Working File (CWF) will appropriately edit for these codes so that the A/B MACs (B) will pay them separately.
Can a physician pay Part B benefits?
Subject to the conditions and limitations described below, payment of Part B benefits due a physician under assignment for services furnished in a facility may be made to the facility if the facility and physician have an agreement under which only the facility may bill and receive fees or amounts charged for the services.
What is Medicare contractor edit?
Medicare contractors perform a series of edits. The initial edits are to determine if the claims in a batch meet the basic requirements of the HIPAA standard. If errors are detected at this level, the entire batch of claims would be rejected for correction and resubmission.
Can a provider purchase software?
Providers can purchase software from a vendor, contract with a billing service or clearinghouse that will provide software or programming support, or use HIPAA compliant free billing software that is supplied by Medicare carriers, DMEMACs and A/B MACs.
What is Medicare claim processing manual?
The Medicare Claims Processing Manual (Internet-Only Manual [IOM] Pub. 100-04) includes instructions on claim submission. Chapter 1 includes general billing requirements for various health care professionals and suppliers. Other chapters offer claims submission information specific to a health care professional or supplier type. Once in IOM Pub. 100-04, look for a chapter(s) applicable to your health care professional or supplier type and then search within the chapter for claims submission guidelines. For example, Chapter 20 is the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS).
What is MSP in Medicare?
MSP provisions apply to situations when Medicare isn’t the patient’s primary health insurance coverage.MSP provisions ensure Medicare doesn’t pay for services and items that pertain to other health insurance or coverage that’s primarily responsible for paying. For more information, refer to the Medicare Secondary Payer
What is the 837P form?
This booklet offers education for health care administrators, medical coders, billing and claims processing personnel, and other medical administrative staff who are responsible for submitting Medicare professional and supplier claims for Medicare payment using the 837P or Form CMS-1500.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…