Part B New Provider Resource Center
- Enroll in the CGS ListServ Notification Service and CMS Listserv. ...
- Become familiar with the CGS and CMS Websites. Access the CGS Part B Website for a variety of educational, billing, and coverage information. ...
- Enroll and Learn About Electronic Billing and myCGS. Read the Electronic Enrollment Packet. This packet provides information about submitting your claims electronically to Medicare.
- Get Acquainted with Medicare. Below is a list of critical resources you will need for providing and billing Medicare-covered services.
Full Answer
How much will you pay for Medicare Part B?
Mar 22, 2019 · Medicare for payment under Part A, the hospital must cancel its Part A claim prior to submitting a claim for payment of Part B inpatient services. Whether or not the hospital submitted aclaim to Part A for payment, Medicarerequires the hospital to submit a Part A claim indicating that the provider is liable under Section 1879 of the Social ...
Does everyone pay the same for Medicare Part B?
An individual already enrolled as a Medicare Part B provider may submit claims listing themselves as the ordering or certifying provider without re-enrolling using Form CMS-855O. Those who enroll as eligible providers using Form CMS-855O may not bill Medicare or get paid by Medicare for their services. They have no Medicare billing privileges.
How do I pay for Medicare Part B?
Pay directly from your savings or checking account through your bank's online bill payment service Some banks charge a service fee. Get details so your payment goes through on time. Mail your payment to Medicare. Pay by check, money order, credit card, or debit card. Fill out the payment coupon at the bottom of your bill, and include it with your payment.
Do I have to pay for Medicare Part B?
As a Part B provider (i.e. physicians and suppliers), you should: Obtain billing information at the time the service is rendered. It is recommended that you use the CMS Questionnaire (available in the Downloads section below), or a questionnaire that asks similar types of questions; and.
How do providers bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
What provider numbers do you need in order to bill Medicare?
To enroll in and obtain payment from Medicare, you must apply for: 1) A National Provider Identifier (NPI); and 2) Enrollment in the Medicare Program. may agree to have an EFI Organization (EFIO) submit application data on your behalf (i.e., through a bulk enumeration process) if an EFIO requests permission to do so.
Can you balance bill a Medicare patient?
Balance billing is prohibited for Medicare-covered services in the Medicare Advantage program, except in the case of private fee-for-service plans. In traditional Medicare, the maximum that non-participating providers may charge for a Medicare-covered service is 115 percent of the discounted fee-schedule amount.Nov 30, 2016
What portion does a Medicare Part B patient pay for services with a participating provider?
For most services, Part B medical insurance pays only 80% of what Medicare decides is the approved charge for a particular service or treatment. You are responsible for paying the other 20% of the approved charge, called your coinsurance amount.
What is the difference between ordering and referring physician?
Referring physician - is a physician who requests an item or service for the beneficiary for which payment may be made under the Medicare program. Ordering physician - is a physician or, when appropriate, a non-physician practitioner who orders non-physician services for the patient.Jan 29, 2018
Who is the rendering provider?
The Rendering Provider is the person or company (laboratory or other facility) who rendered the care. In the case where a substitute provider (locum tenens) was used, enter that provider's information here. Future Versions of 837P. The Rendering Provider is the individual who provided the care.
How do you handle balance billing?
Steps to Fight Against Balance BillingReview the Bill. Billing departments in hospitals and doctor offices handle countless insurance claims on a daily basis. ... Ask for an Itemized Billing Statement. ... Document Everything. ... Communicate with Care Providers. ... File an Appeal with Insurance Company.May 18, 2020
How should Procedures designated as each in the CPT manual be coded billed?
How should procedures designated as "each" in the CPT manual be coded/billed? They should be billed as per unit on the claim form. (Procedures designated as "each" should be billed per unit.)
When a Medicare patient seeks care from a non par provider?
Non-participating providers accept Medicare but do not agree to take assignment in all cases (they may on a case-by-case basis). This means that while non-participating providers have signed up to accept Medicare insurance, they do not accept Medicare's approved amount for health care services as full payment.
Which of the following expenses would be paid by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
What is a participating provider?
Participating Provider — a healthcare provider that has agreed to contract with an insurance company or managed care plan to provide eligible services to individuals covered by its plan. This provider must agree to accept the insurance company or plan agreed payment schedule as payment in full less any co-payment.
How much does Medicare Part B pay for physician fees quizlet?
Part B of Medicare pays 80% of physician's fees (based upon Medicare's physician fee schedule) for surgery, consultation, office visits and institutional visits after the enrollee meets a $185 deductible/yr. (2019). Then the patient pays 20% coinsurance of the Medicare approved amount for services.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What are the two types of NPIs?
There are 2 types of NPIs: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs for solely ordering items or certifying services. Apply for an NPI in 1 of 3 ways:
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.
How long does it take for Medicare to pay Part B?
Like other commercial insurances, you should send Medicare Part B claims directly to Medicare for payment, with an expected turnaround of about 30 days. Unlike typical commercial insurance, Medicare can pay either the provider or the patient, depending on the assignment.
What is Medicare Part B for eyeglasses?
Other preventative services are also covered under Medicare Part B: Preventive shots, including the flu shot during flu season, and three Hepatitis B shots, if you're considered at risk.
What is CMS in Medicare?
CMS, the Centers for Medicare and Medicaid Services, governs all parts of Medicare, including Part B. CMS holds a great amount of influence over the way insurance companies pay doctors, as well as the services that doctors provide. This is, in large part, because of Medicare Part B restrictions. Every type of healthcare service eligible ...
Why is Medicare important?
Because Medicare is a service provided for the elderly, disabled, and retired, the patients who are covered by Medicare will usually have limited financial resources . Because of this, it's very important to make sure that your office bills and codes within all Part B guidelines and provides only approved Part B services.
What is medically necessary?
Medically Necessary Services: These include services and supplies needed to treat your medical condition. To be covered, the service also has to be within the standards of medical practice. This means that holistic or naturopathic treatments wouldn't be covered.
What is a lab and pathology?
Laboratory and Pathology services such as blood tests and urinalyses. Preventive services that will help prevent, manage, or diagnose a medical condition. Other services are covered by Part B Medicare, as long as they're related to one of the conditions that are considered medically necessary by Medicare.
What are the services that are considered medically necessary?
These services include: Home health services, only when they are medically necessary, and of limited duration. Chiropractic services, only if it is to correct spinal subluxation. Ambulance services, only if a different type of transportation would endanger the patient's health.
Step 1: Enroll in the CGS Email Notification Service and CMS Listserv
Sign up for the CGS Email Notification Service, which is the primary means used by CGS to communicate new or changing Medicare information with providers. CGS also communicates information via Facebook and LinkedIn.
Step 2: Become familiar with the CGS and CMS Websites
Access the CGS Part B Website for a variety of educational, billing, and coverage information.
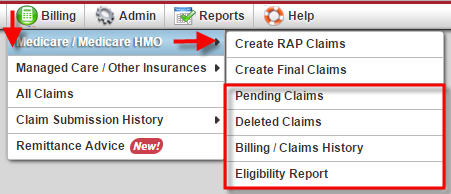
Step 3: Enroll and Learn About Electronic Billing and myCGS
Read the Electronic Enrollment Packet. This packet provides information about submitting your claims electronically to Medicare. You must bill your claims electronically, unless you meet the exception for a small provider. Complete the Electronic Data Interchange (EDI) forms, which can be accessed from the Electronic Enrollment Packet.
Step 4: Get Acquainted with Medicare
Below is a list of critical resources you will need for providing and billing Medicare-covered services. Consider bookmarking these web addresses for future reference.
How long does it take to file Medicare claims?
Medicare claims must be filed within one full calendar year ...
Why is it important to check your Medicare summary notice?
It’s important to check your Medicare Summary Notice (MSN) to make sure your claims are being filed on time. If you discover claims are not being filed in a timely manner, you should first contact your physician and/or supplier and ask them to file the claim.
What happens if you don't file a claim with Medicare?
If a claim isn’t filed within the time limit, Medicare may not pay its share. It’s important to check your Medicare Summary Notice ...
