Secondary claim submission CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
Full Answer
How do I bill Medicare as the secondary payer?
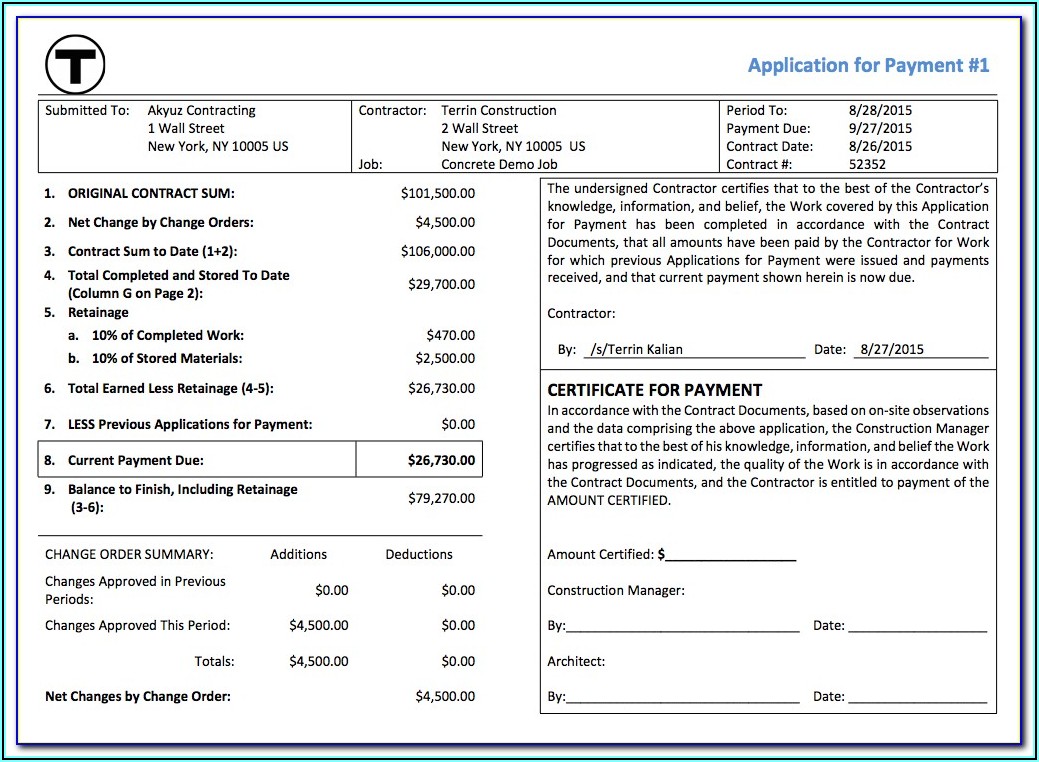
· Paper claim submission. When submitting a paper claim to Medicare as the secondary payer, the CMS-1500 (02-12) claim form must indicate the name and policy number of the beneficiary's primary insurance in items 11-11c. For additional instructions on completing the CMS 1500 (02-12) claim form, please refer to the Completion of CMS 1500 (02-12) claim form.
How do Part B providers bill Medicare?
· The proposed rule, Medicare Program; Part B Inpatient Billing in Hospitals, proposes that if the beneficiary is enrolled in Part B, Medicare would pay for all reasonable and necessary Part B hospital inpatient services when a Part A inpatient admission is denied as not reasonable and necessary, instead of just the limited list of Part B inpatient services currently …
Do Medicare supplemental insurance plans cover Medicare Part B claims?
Submitting Medicare Part B billing claims After you've determined that your patient has active coverage and that the service will be covered, you'll have to bill the claim to insurance. Like other commercial insurances, you should send Medicare Part B claims directly to Medicare for payment, with an expected turnaround of about 30 days.
How long does it take to bill Medicare Part B?
· Medicare law and regulations require all entities that bill Medicare for services or items given to Medicare beneficiaries to decide whether Medicare is the primary payer for those services or items before submitting a claim to Medicare. (See . Section 1862(b)(2) of the Social Security Act and regulations at 42 CFR 489.20g.)
How do I submit Medicare secondary claims?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
How do I bill Medicare as a secondary payer?
When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract.
Is Medicare Part B My primary or secondary?
Your group insurance plan is the secondary insurer, so you should enroll in Medicare Part B before your group plan will pay its portion of the claim.
What is Medicare Secondary Payer Rule?
Generally the Medicare Secondary Payer rules prohibit employers with 20 or more employees from in any way incentivizing an active employee age 65 or older to elect Medicare instead of the group health plan, which includes offering a financial incentive.
What is a Medicare Secondary qualifier?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.
Does Medicare automatically forward claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
How do you determine which insurance is primary and which is secondary?
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.
What is the purpose of the Medicare Secondary Payer questionnaire?
CMS developed an MSP questionnaire for providers to use as a guide to help identify other payers that may be primary to Medicare. This questionnaire is a model of the type of questions you should ask to help identify MSP situations.
How does two health insurances work?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
When would a biller most likely submit a claim to secondary insurance?
If a claim has a remaining balance after the primary insurance has paid, you will want to submit the claim to the secondary insurance, if one applies.
Will Medicare pay secondary if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
What is the timely filing limit for Medicare secondary claims?
12 monthsQuestion: What is the filing limit for Medicare Secondary Payer (MSP) claims? Answer: The timely filing requirement for primary or secondary claims is one calendar year (12 months) from the date of service.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What happens if a group health plan doesn't pay?
If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment. Medicare may pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim.
What is MSP in Medicare?
The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Physicians, non-physician practitioners and suppliers are responsible for gathering MSP data to determine whether Medicare is the primary payer by asking Medicare beneficiaries questions concerning their MSP status.
What is MSP billing?
MSP billing. When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, ...
What is Medicare Part B billing?
An important thing to understand about Medicare Part B billing is that each person must pay a premium each month, and pay a yearly deductible and copay. As such, Part B is a lot like regular commercial insurance plans. But unlike regular commercial insurance plans, Part B Medicare coverage only includes two types of services:
What is the difference between Medicare Part B and Part A?
Medicare part B is the plan that you use to go see your doctor, whereas Medicare part A is the plan that you'd use if you were an inpatient in a hospital. The two are not interchangeable!
What is CMS in Medicare?
CMS, the Centers for Medicare and Medicaid Services, governs all parts of Medicare, including Part B. CMS holds a great amount of influence over the way insurance companies pay doctors, as well as the services that doctors provide. This is, in large part, because of Medicare Part B restrictions. Every type of healthcare service eligible ...
Why is Medicare important?
Because Medicare is a service provided for the elderly, disabled, and retired, the patients who are covered by Medicare will usually have limited financial resources . Because of this, it's very important to make sure that your office bills and codes within all Part B guidelines and provides only approved Part B services.
What is Part C?
Part C combines Parts A and B (and sometimes D), and is managed by private insurance companies as approved by Medicare. Part D is a prescription drug coverage program which is also managed by private insurance companies as approved by Medicare. Each of these parts provides a different type of coverage, with different limitations ...
What is medically necessary?
Medically Necessary Services: These include services and supplies needed to treat your medical condition. To be covered, the service also has to be within the standards of medical practice. This means that holistic or naturopathic treatments wouldn't be covered.
What is Part B reimbursement?
Every type of healthcare service eligible for reimbursement by Part B is subject to a great deal of rules, regulations, and guidelines. These range from the rule that all medical procedures must meet the standards of currently accepted medical practice, to the way certain claims must be billed for special services.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
What is secondary payer?
A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
:max_bytes(150000):strip_icc()/CMS-1500-claim-form-57a2d3a85f9b589aa99caf8b.jpg)