MSP billing. When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.
Full Answer
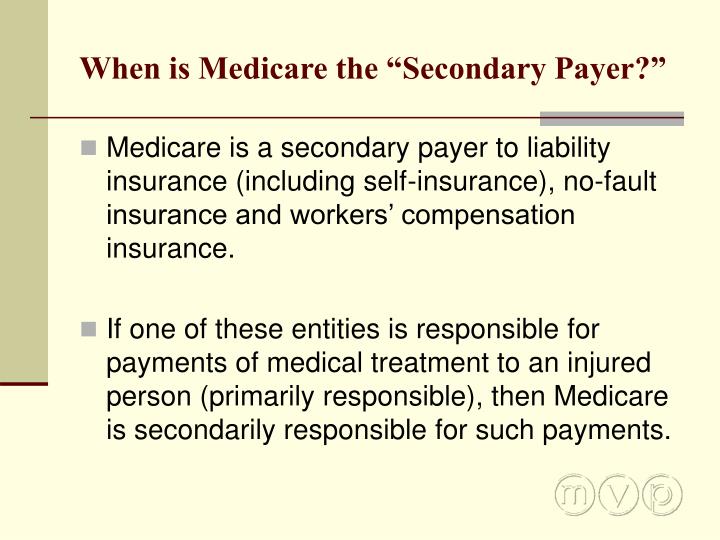
What does it mean when Medicare is a secondary payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility; that is, when another entity has the responsibility for paying beforeMedicare. Over the years, Congress has made an effort to shift costs from Medicare to the appropriate private sources of payment, which has resulted in significant savings to the Medicare Trust Fund.
Does Medicare automatically Bill secondary insurance?
Medicare usually covers most of your healthcare costs, but if you have other insurance coverage, it can act as a secondary payer for some of the costs.
How does Medicare calculate secondary payment?
How does Medicare calculate secondary payment? Medicare's secondary payment will be based on the full payment amount (before the reduction for failure to file a proper claim) unless the provider, physician, or other supplier demonstrates that the failure to file a proper claim is attributable to a physical or mental incapacity of the ...
How to deal with Medicare as a secondary insurance?
- Vision: Your medical plan will not cover you for vision care. ...
- Dental: A dental plan can cover you for preventive care such as routine teeth cleanings and some X-rays. ...
- Disability: Short- and long-term disability plans are a type of secondary insurance coverage. ...
How do I bill Medicare secondary claims?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
How Does Medicare pay as a secondary payer?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
What is the payer code for Medicare secondary?
Use payer code Z for Medicare. Payer codes (Code IDs): A = Working Aged beneficiary/spouse with an EGHP (beneficiary age 65 or over) – Beneficiary must be enrolled in Part A for this Provision to apply (VC 12) B = ESRD beneficiary with EGHP in MSP/ESRD 30-month coordination period (VC 13)
Is Medicare billed as primary or secondary?
Medicare is primary and your providers must submit claims to Medicare first. Your retiree coverage through your employer will pay secondary. Often your retiree coverage will provide prescription drug benefits, so you may not need to purchase Part D.
How do you fill out CMS 1500 when Medicare is secondary?
0:239:21Medicare Secondary Payer (MSP) CMS-1500 Submission - YouTubeYouTubeStart of suggested clipEnd of suggested clipHere when the insured. And the patient are the same the biller enters the word. Same if medicare isMoreHere when the insured. And the patient are the same the biller enters the word. Same if medicare is primary this item is left blank.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
What is MSP Code W?
OTHER. 5371.1 The CWF and contractor shared systems shall accept a new MSP code “W” for Workers' Compensation Medicare Set- aside Arrangement (WCMSA) for use on the HUSP records for application on the HUSP Auxiliary file.
What is MSP code G?
Primary Payer Code = G. 44. Amount provider was obligated/required to accept from a primary payer as payment in full due to contract/law when that amount is less than charges but higher than amount actually received. An MSP payment may be due.
How do you use MSP codes?
How do I redeem a Gift Certificate?Log in to your MovieStarPlanet account.Click the “Settings” button in the top right corner.Click the “Redeem Gift Certificate” button.Type in the code on your Gift Certificate and press “Redeem Code”
Is Medicare always the primary payer?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Is Medicare Secondary Payer questionnaire required?
Providers are required to complete a Medicare Secondary Payer Questionnaire (MSPQ) upon admission of each Medicare patient. A sample of the MSPQ can be found in the Centers for Medicare & Medicaid Services' (CMS) Internet-Only Manual (IOM), Publication 100-05, Medicare Secondary Payer Manual, Chapter 3, Section 20.2.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
When is Medicare a secondary payer?
The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.
What is MSP in Medicare?
The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Physicians, non-physician practitioners and suppliers are responsible for gathering MSP data to determine whether Medicare is the primary payer by asking Medicare beneficiaries questions concerning their MSP status.
How much is Medicare fee schedule?
The Medicare fee schedule amount is $185, and no Medicare benefits are payable. The patient can be billed for the remaining $110, and $185 would go toward the Part B deductible. A patient has a $185 deductible, which he or she has paid $50 toward. He or she incurred $100 in charges, which the primary payer paid in full.
Do you have to ship a claim off to the primary payer?
Similar to any other scenario involving primary and secondary payers, you’ll need to ship the claim off to the primary payer first. Only once you’ve received an Explanation of Benefits (EOB) from the primary insurance can you attempt to bill Medicare.
Does Medicare credit deductibles?
In other words, Medicare will credit any amount paid by the primary insurance up to the amount allowed by the Medicare fee schedule toward the deductible. Here are a couple of examples: Say a patient’s deductible is $185, which he or she has not yet met.
Can Medicare and other insurances work together?
And for Medicare patients with other health insurance providers, few things are better than when Medicare and their private payers work together cooperatively. However, Medicare has a lot of unique rules, which means providers should tread carefully when their patients have Medicare and a second insurance. To that end, here’s a rundown of all the things PTs, OTs, and SLPs need to know about Medicare as a secondary payer:
Is Medicare a secondary insurance?
This first part is often where things go awry: Medicare functions differently depending on the other types of insurance benefits the patient receive s (i.e., Medicare always functions as the secondary in some instances).
Do Medicare patients have to pay deductibles?
As CMS explains in the Medicare Secondary Payer Manual, patients will likely still have to make payments toward their deductibles, which “are credited to those deductibles even if the expenses are reimbursed by a [group health plan].”.
Do you have to follow Medicare plan of care rules?
Follow all plan of care rules—even if Medicare is the secondary. According to PT compliance expert Rick Gawenda (as mentioned in a comment here ), you must adhere to all of Medicare’s plan of care rules and documentation standards when you submit claims to Medicare—even when it’s a secondary insurance.
Submitting MSP Claims via FISS DDE or 5010
All MSP claims submitted via FISS DDE or 5010 must report claim adjustment segment (CAS) information. In FISS DDE, the CAS information is entered on the "MSP Payment Information" screen (MAP1719), which is accessed from Claim Page 03 by pressing F11. This is in addition to the normal MSP coding information.
Correcting MSP Claims and Adjustments
Return to Provider (RTP): MSP claims may be corrected out of the RTP file (status/location T B9997). However, providers must ensure that claim adjustment segment (CAS) information is reported on the "MSP Payment Information" screen (MAP1719), accessed from Claim Page 03 by pressing F11.
