For untimed codes, multiply the total time spent by 10% to determine if OTA treatment time exceeded it. The untimed codes are: 97165, 97166, 97167, 97168, 97150, 92610, 92526, 96110, and 96127, supervised modalities Clinical Scenarios
Full Answer
How are untimed codes billed?
Untimed Codes are billed one unit per date of service regardless of the number of anatomical body areas treated. It does not matter if you spend 2 minutes or an hour treating the patient using these codes, you can only report one unit per code.
How many minutes must be provided to Bill a timed code?
The following chart documents how many minutes must be provided in order to bill the corresponding number of units. Note how 1 billable unit for a timed code must be at least 8 minutes, and it does not increase to a second billable unit until you have at least 8 minutes past the 15-minute mark.
What is the billable time for timed CPT codes?
Note how 1 billable unit for a timed code must be at least 8 minutes, and it does not increase to a second billable unit until you have at least 8 minutes past the 15-minute mark. If more than one timed CPT code is billed during a calendar day, then the total treatment time determines the number of units billed.
Can procedure codes be billed by units of time?
Can procedure codes be billed by units of time? Most speech-language pathology codes do not have time units assigned to them, such as 92507 (speech-language treatment). If no time is noted in the descriptor, each code counts as one session.

How do you bill untimed codes?
How do I bill timed and untimed codes? Let's start with the easier of the two: untimed codes. As mentioned above, you may bill one unit of each untimed service per patient per date of service. Whether you provide an untimed service for five minutes or 50, you will always bill one single unit.
Which of the following is an example of an untimed CPT code?
The following are examples of untimed codes: Evaluations/Re-evaluations (97161-97168). Group therapy (97150). Supervised modalities (97012).
How many units is 40 minutes?
3 unitsAppropriate billing for 40 minutes is for 3 units. Bill 2 units of 97110 and 1 unit of 97140.
How do you bill a physical therapy unit?
To calculate the number of billable units for a date of service, providers must add up the total minutes of skilled, one-on-one therapy and divide that total by 15. If eight or more minutes remain, you can bill one more unit.
What are untimed codes?
When a therapy service is not defined by a specific timeframe, it is an “untimed” therapy procedure (CPT or HCPCS) code. Untimed codes are billed with a unit of one (1) per date of service. The unit for untimed codes is one regardless of how long the evaluation or service took.
Is mechanical traction timed or untimed?
untimedBecause mechanical traction is an 'untimed' treatment code, it is the only counted in the total treatment time.
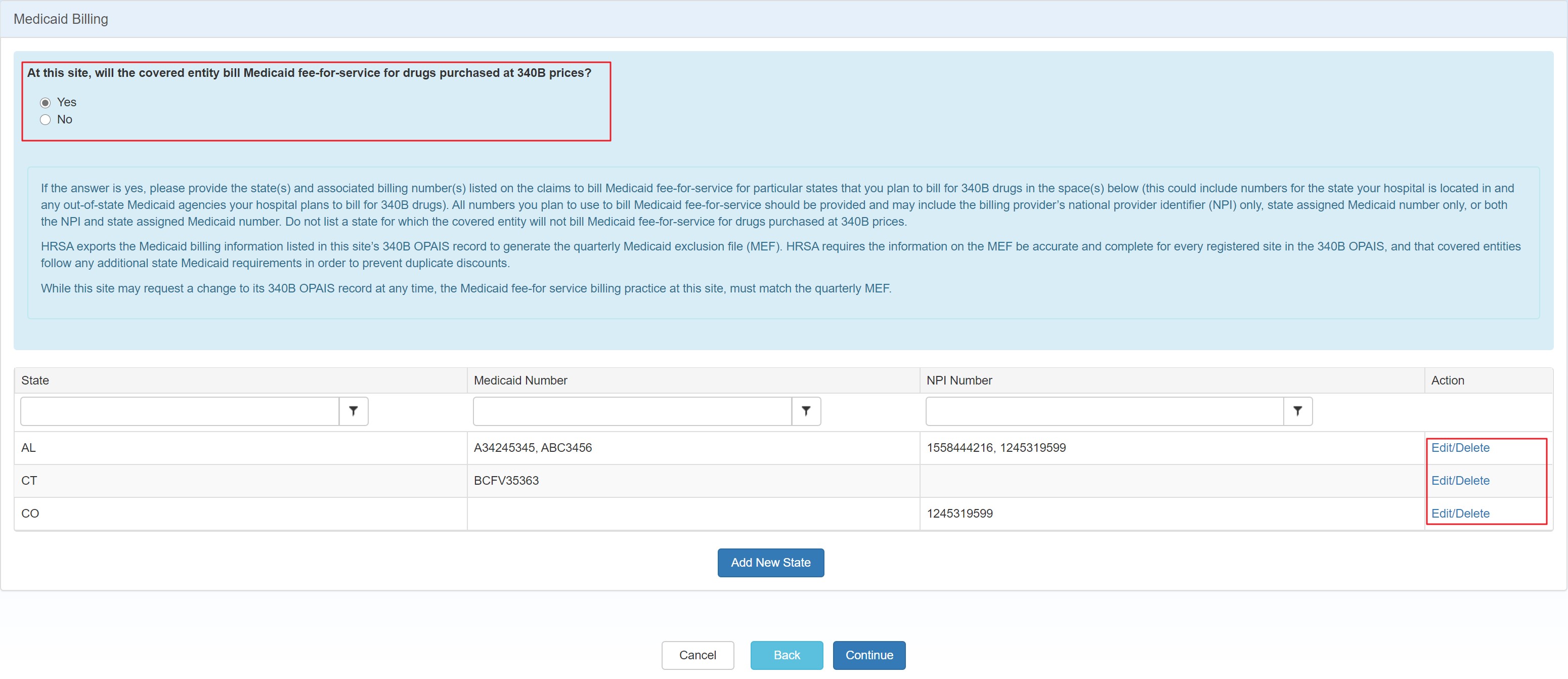
What is Medicare 8-minute rule?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized.
How many units can you bill for Medicare?
The rule allows practitioners to bill Medicare for one unit of service if its length is at least eight (but fewer than 22) minutes. A billable “unit” of service refers to the time interval for the service.
Who follows the 8-minute rule?
The 8-minute rule is used by pediatric therapists, including occupational therapists, physical therapists, and speech therapists. In order to fully understand the 8-Minute Rule, you must first understand what constitutes billable time, specifically the difference between service-based and time-based CPT codes.
What codes can a physical therapist Bill?
Common Physical Therapy CPT Codes29240, 29530, 29540: Strapping.97110: Therapeutic Exercise.97112: Neuromuscular Re-education.97116: Gait Training.97140: Manual Therapy.97150: Group Therapy.97530: Therapeutic Activities.97535: Self-Care/Home Management Training.More items...•
What CPT codes can a physical therapist Bill?
Physical Therapy CPT Codes97161: Physical therapy evaluation, low complexity.97162: Physical therapy evaluation, moderate complexity.97163: Physical therapy evaluation, high complexity.
How does billing work in physical therapy?
How Does Therapy Billing Work?A bill is submitted to the patient, third-party payer directly, or a 'claims clearinghouse' that prepares the bill.The claims clearinghouse will submit the bill to the payer. ... Copayments are collected at the time of service.
How long is a 15 minute code?
No. Medicare has established specific minimum and maximum times for 15-minute codes and most payers have adopted this policy. The minimum time for one 15-minute code is 8 minutes. Two units would be a minimum of 15 + 8 minutes = 23 minutes. This rule is extended to multiple units in the following CMS table:
What would happen if the treatment code (92507) was revised?
If the treatment code (92507) is revised, the development of additional treatment codes that could address complexity of services would be considered at that time . ASHA would have to present evidence that the services are different in terms of the time it takes to perform the service, the level of technical skill, the physical effort, ...
What is a CPT modifier?
One of the CPT modifiers is -22, added at the end of the CPT code. This modifier denotes a session or procedure that is unusually long. Many payers will increase reimbursement by 25 to 50 percent when this modifier is included, but the claim will be stopped for manual review and you will need to submit additional documentation with your claim to justify the increased services. Be warned that if you submit claims with the -22 modifier too often, the payer may conclude that the long sessions are not "unusual," and cease to honor the modifier.
Can speech language pathology codes be billed by time units?
Can procedure codes be billed by units of time? Most speech-language pathology codes do not have time units assigned to them, such as 92507 (speech-language treatment). If no time is noted in the descriptor, each code counts as one session.
Is there a minimum time for untimed codes?
However, there are no hard and fast rules regarding time "minimums" for untimed codes. Ultimately, the decision to bill a code depends on the clinician’s judgement and documentation to support that the time spent with the patient was medically necessary and clinically appropriate for that patient on that day.
Do untimed codes have a typical time?
However, untimed codes do have any underlying "typical" time associated with each code. These times are derived from surveys of speech-language pathologists that ASHA conducts in conjunction with the American Medical Association.
Why are untimed codes important?
Untimed codes, therefore, allow a certain amount of flexibility—within reason—to spend more time with some patients and less with others. Underlying times may also help clinicians determine if they should bill a CPT code when a session is substantially shorter than the underlying time.
How long is CPT code 92557?
For example, CPT code 92507 has a total underlying time of 60 minutes, and CPT code 92557 has a total time of 28 minutes.
How long is a 5 unit CPT?
5 units: 68 minutes to less than 83 minutes. 6 units: 83 minutes to less than 98 minutes. Medicare has a list of Medically Unlikely Edits (MUEs), which determines the maximum number of billable units for each CPT code. Many other payers may follow Medicare MUEs or have their own similar list.
How long is a 15 minute unit?
Medicare publishes the following guide for reporting 15-minute units: 1 unit: 8 minutes to less than 23 minutes. 2 units: 23 minutes to less than 38 minutes. 3 units: 38 minutes to less than 53 minutes. 4 units: 53 minutes to less than 68 minutes. 5 units: 68 minutes to less than 83 minutes.
Is there a rule for billed sessions?
No. There are no rules regarding the length of billed session-based codes. However, these underlying times can serve as a guide or advocacy tool when a clinician is feeling pressure to shorten session lengths to maximize time and payment.
Is CPT code 92507 untimed?
Yes, most audiology and speech-language pathology codes are untimed—that is, they don’t have a time unit in their descriptors and are considered “session-based.”. Untimed codes may be reported once per day, regardless of the length of the session. Examples include CPT codes 92507 (Treatment of speech, language, voice, communication, ...
Negotiating an Equitable Payment Rate - You Can Do It!
Here is a scenario to consider: a health plan sends you a notice saying it will no longer accept time units for untimed CPT codes, such as 92507 or 92610. The health plan offers a revised reimbursement rate that is significantly lower than the previous payment when time units were allowed.
An Adapted Mertz Negotiation Approach
Step 1 Generate a report on your CPT codes and their frequency, using billing software if possible, and covering a three month period.
Develop an Action Plan
Negotiate Individual Fees Target specific codes for increases based on your gathered data. Your first contact in the negotiation process might be the health plan provider relations representative. If your argument is compelling, the discussion will move up to the contracting manager.
Timed codes
Several CPT codes used for therapy modalities, procedures, and tests and measurements specify that direct (one-on-one) time spent with the patient is 15 minutes. Report procedure codes for services delivered on any single calendar day using CPT codes and the appropriate number of 15 minute units of service.
Examples
The following examples illustrate how to count the appropriate number of units for the total therapy minutes provided.
Untimed codes
The units for untimed codes are reported based on the number of times the procedure is performed, as described in the HCPCS code definition (often once per day). When reporting service units for codes where the procedure is not defined by a specific timeframe (untimed codes), a 1 is entered in the unit's field.
Reference
CMS, Internet Only Manual, Publication 100-04, Claims Processing Manual, Chapter 5, Section 20.2
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Language quoted from Centers for Medicare and Medicaid Services (CMS), National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
Article Guidance
This article gives guidance for billing, coding, and other guidelines in relation to local coverage policy Outpatient Physical and Occupational Therapy Services L34049.
ICD-10-CM Codes that DO NOT Support Medical Necessity
The following ICD-10-CM Codes do not support the medical necessity for the CPT/HCPCS code 97035.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How often is 97150 billed?
In private practice settings for physical and occupational therapists and in physician offices where therapy services are provided incident to the physician, Medicare expects the group therapy code (97150) to be billed only once each day per patient. In the facility/institutional therapy settings, the group therapy code could be applied more than once. However, the occasional situation where group therapy is billed more than once each day would require sufficient documentation to support its medical necessity and clinical appropriateness of providing more than one separate session of group therapy.
How long can a therapist bill for a supervised modality?
In the same 15-minute time period, one therapist may bill for more than one therapy service occurring in the same 15-minute time period where "supervised modalities" are defined by CPT as untimed and unattended -- not requiring the presence of the therapist (CPT codes 97010 - 97028). One or more supervised modalities may be billed in the same 15-minute time period with any other CPT code, timed or untimed, requiring constant attendance or direct one-on-one patient contact. However, any actual time the therapist uses to attend one-on-one to a patient receiving a supervised modality cannot be counted for any other service provided by the therapist.
Can a therapist bill a patient separately?
Therapists, or therapy assistants, working together as a "team" to treat one or more patients cannot each bill separately for the same or different service provided at the same time to the same patient.
How many minutes can you bill for untimed codes?
For example, it you spent 38 minutes on timed codes and 30 minutes on untimed codes, the maximum number of units you can bill for is 3 units (38 to 52 minutes) based on the table. Remember, you only count the timed code minutes and you must ignore the untimed code minutes.
How long is a 15 minute timed code?
For the individual codes, you need to code based on the following rules: If a service represented by a 15 minute timed code is performed in a single day for at least 15 minutes, that service shall be billed for at least one unit.
How long is a 97712 treatment?
Example 1: 24 minutes of neuromuscular reeducation, code 97712. 23 minutes of therapeutic exercise, code 97110. Total timed code treatment time is 47 minutes. If you look up 47 minutes on the chart, you can bill for a maximum of 3 units (38 to 52 minutes).
What is the time period for 97545?
The code 97545 is for the time period included in the first 2 hours and the code 97546 includes the time period for each additional hour (after the first 2 hours). Normally these codes are used to report services to a patient's Workers Compensation program and are only rarely used for Medicare.