How do I get Medicare certification as a home care provider?
Mar 30, 2022 · Skilled nursing facilities (SNFs) and nursing facilities (NFs) are required to be in compliance with the requirements in 42 CFR Part 483, Subpart B, to receive payment under the Medicare or Medicaid programs. To certify a SNF or NF, a state surveyor completes at least a Life Safety Code (LSC) survey, and a Standard Survey.
How does home health care work with Medicare?
Oct 27, 2020 · When you subscribe to CMS on the Federal Register website, you’ll be notified of statuses, moratoria, and proposed rules concerning the Medicare program. Go to CMS on the Federal Register website. State Medicaid Agency (SMA) Provider Enrollment Contact List Medicaid COVID-19 Vaccine Enrollment Contact Information (PDF) Other Links
How do I get an SNF/NF certificate?
Feb 26, 2020 · The Medicare program conditions of payment require a physician certification and (when specified) recertification for SNF services. Analysis of claim denials from CERT, RA and MAC contractors has identified a trending related to the failure to comply with the certification or re-certification requirements. Providers are reminded to comply, maintain, and submit this …
How are Medicare skilled nursing facility reimbursements calculated?
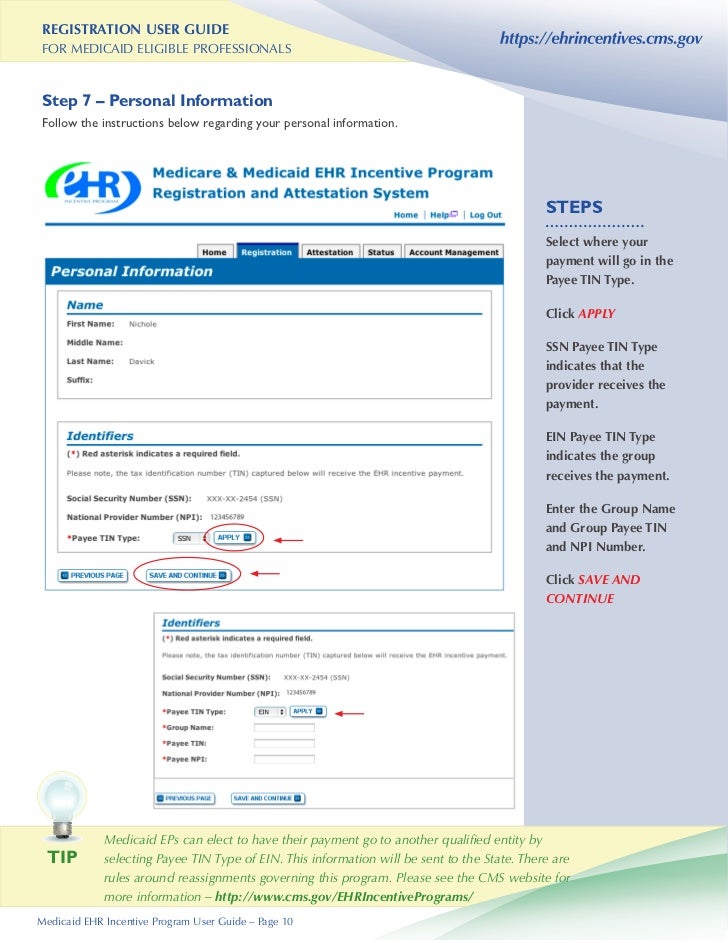
Jan 22, 2019 · Starting the Process. Home care providers seeking Medicare certification will need to complete the following forms: CMS-1572 (a and b) (PDF) CMS-1561 (PDF) Complete the Civil Rights Attestation and the Assurance of Compliance form at US Office of Civil Rights Assurance of Compliance. Email or mail these documents to:

What is a CMS certificate?
The CMS Certification number (CCN) replaces the term Medicare Provider Number, Medicare Identification Number or OSCAR Number. The CCN is used to verify Medicare/Medicaid certification for survey and certification, assessment-related activities and communications.
What is a CMS F tag?
F-Tags refer to areas of compliance assessed during a Centers for Medicare and Medicaid Services or CMS Survey. F-Tags are used by your state and CMS to identify deficiencies based on a community's performance within CMS standards and guidelines. Each tag is related to one area of the Code of Federal Regulations.
What is CMS compliance?
The CMS National Standards Group, on behalf of HHS, administers the Compliance Review Program to ensure compliance among covered entities with HIPAA Administrative Simplification rules for electronic health care transactions.Dec 1, 2021
What is the name of CMS's web based reporting system for nursing homes?
Please visit the Skilled Nursing Facility web page within Care Compare (CCXP) and Provider Data Catalog (PDC) to view the updated quality data. The Centers for Medicare & Medicaid Services (CMS) discovered an error in measure calculations for the DTC-Post Acute Care (PAC) SNF Quality Reporting Program (QRP) measure.Mar 23, 2022
What does IG mean in nursing home?
Immediate JeopardyImmediate jeopardy is a situation in which the nursing home's non-compliance with one or more requirements has caused, or is likely to cause, serious injury, harm, impairment, or death to a resident.
What happens when a nursing home gets an IJ tag?
When an IJ is identified, the Regional Office needs to take action itself or notify your State Medicaid Agency to take action. The facility will face termination of their Provider Agreement and/or the appointment of a temporary manager to remove the IJ situation.Jul 19, 2012
What are the 7 elements of compliance?
The 7 Elements of a Compliance Program Are as Follows:Implementing written policies, procedures, and standards of conduct.Designating a compliance officer and compliance committee.Conducting effective training and education.Developing effective lines of communication.Conducting internal monitoring and auditing.More items...•Nov 1, 2021
Does CMS require a compliance program?
The development and implementation of a compliance program is voluntary, but CMS believes that an effective compliance program is a cost-effective investment. It should be noted, however, that CMS is not specifically authorizing funding for any of the recommendations contained in this guidance.
Are Medicare Parts C and D required to have a compliance program?
Medicare Parts C and D plan Sponsors are not required to have a compliance program.
What is a Casper report CMS?
CASPER is the acronym for Certification and Survey Provider Enhanced Reporting system. The CASPER reports are generated from Minimum Data Set (MDS) data 3 Page 4 4 types of CASPER reports are available.
What are Casper reports?
CASPER is an acronym for Certification And Survey Provider Enhanced Reports. These are reports that are compiled using your submitted OASIS data to demonstrate your agency's performance. Current metrics are benchmarked against a prior period and the national rate.Jun 19, 2018
What is the CMS quality reporting program?
Under the Hospital Inpatient Quality Reporting Program, CMS collects quality data from hospitals paid under the Inpatient Prospective Payment System, with the goal of driving quality improvement through measurement and transparency by publicly displaying data to help consumers make more informed decisions about their ...Dec 1, 2021
How long does it take to get a recertification?
Subsequent recertifications are required at intervals not to exceed 30 days. Delayed Certification/Recertifications. Delayed certifications and recertifications are allowed for an isolated oversight or lapse.
What is a PA in nursing?
A nurse practitioner (NP), clinic al nurse specialist (CNS) or a physician assistant (PA) who does not have a direct or indirect employment relationship with the facility, but who is working in collaboration with the physician. Timing of Certification/Recertifications.
What is CDT used for?
Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT.
Starting the Process
Home care providers seeking Medicare certification will need to complete the following forms:
Onsite Medicare Survey
When above documents are complete, MDH will send a questionnaire asking to acknowledge that you are ready for an initial Medicare survey. You can choose to have MDH conduct the initial certification survey or you can choose to have a Region V Office of CMS-approved accrediting organization conduct the initial survey.
Questions?
Please contact our Health Regulation Division: [email protected] or#N#651-201-4200.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
What is Medicare Advantage?
As Medicare Advantage (MA) expands in the marketplace , healthcare payers involved in Medicare and Medicaid are increasingly challenged to optimize and modernize their core administrative processes. Manual processes and legacy administrative systems are costly and inaccurate. Payer organizations are increasingly aware that leveraging automated claims adjudication software is the single greatest step they can take to process claims with sufficient speed and accuracy to reduce or eliminate duplication errors for an accelerated ROI. The comprehensive PLEXIS platform allows you to meet evolving standards for regulatory compliance while delivering coordinated, consistent, cost-effective care for all your MA needs.
What is plexis software?
PLEXIS’ comprehensive enterprise platform is the premier claims adjudication and benefit administration software solution on the market. Serving all major healthcare payers for the past 20 years, PLEXIS simplifies and automates claims processing operations. PLEXIS’ agile, trusted technology is eminently configurable to empower you to manage all aspects of claims onboarding and integration.
When did CMS start rating nursing homes?
CMS launched its five-star rating system for Medicare and Medicaid certified nursing homes in December 2008. The system awards stars in three subcategories to determine an overall composite star rating for each nursing home. The three subcategories are onsite health inspections, staffing and quality measures.
How to improve nursing home quality?
Alexander recommended three steps nursing homes can take to conquer this key piece of the five-star rating formula: 1 Know and collect the data elements required for each quality measure. 2 Review and improve MDS coding accuracy. 3 Review and improve all clinical care and systems that affect quality and safety outcomes.
How are health inspection stars determined?
Health inspection stars are determined by onsite inspection scores, and onsite inspection scores are determined by adverse events that can harm nursing home residents. Low scores are better than high scores. For example, adverse events that affected one or two residents and caused no harm are worth zero points.