
You can change from Medicare Advantage to Medigap
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
How to switch from Medicare Advantage to Original Medicare?
Jun 09, 2020 · Guaranteed Approval options: 1.) If you are trying to switch from Medicare Advantage to Medigap during either your first year of enrollment into Medicare Advantage (and 65 years old) or the special enrollment period, then you are guaranteed approved. 2.) Special enrollment periods cover a few circumstances.
Can I disenroll from Medicare Advantage plan?
If changing from an Advantage plan to Medigap is your goal, you need to apply as early as possible. You want to be sure the Medigap plan accepts your …
Why choose a Medicare Advantage plan?
Nov 08, 2019 · If you have a Medigap plan, you can switch to another Medigap plan at any time. However, if you already have Medicare Advantage and want a new Medicare Advantage plan, or if you have Medigap but want to switch to Medicare Advantage, you’ll have to wait for one of three* Medicare Advantage enrollment periods: Annual Enrollment Period: October ...
What is Medicare Advantage vs Medicare?
How to switch from Medicare Advantage to Medigap A person can take the following steps to switch from Medicare Advantage to original Medicare plus Medigap during an …
Can you switch from Advantage plan to Medigap?
Can you switch from Medicare Advantage to Medigap with pre existing conditions?
Can I switch from a Medicare Advantage plan back to Original Medicare?
Is it better to have Medicare Advantage or Medigap?
How do I disenroll from a Medicare Advantage plan?
Why do doctors not like Medicare Advantage plans?
Can a person have a Medicare Advantage plan and a Medicare Supplement plan?
Can Medigap insurance be denied for pre existing conditions?
Does getting a Medicare Advantage plan make you lose original Medicare?
What is the downside to Medigap plans?
Why is Medigap so expensive?
Who pays for Medigap?
Is Medigap better than Medicare?
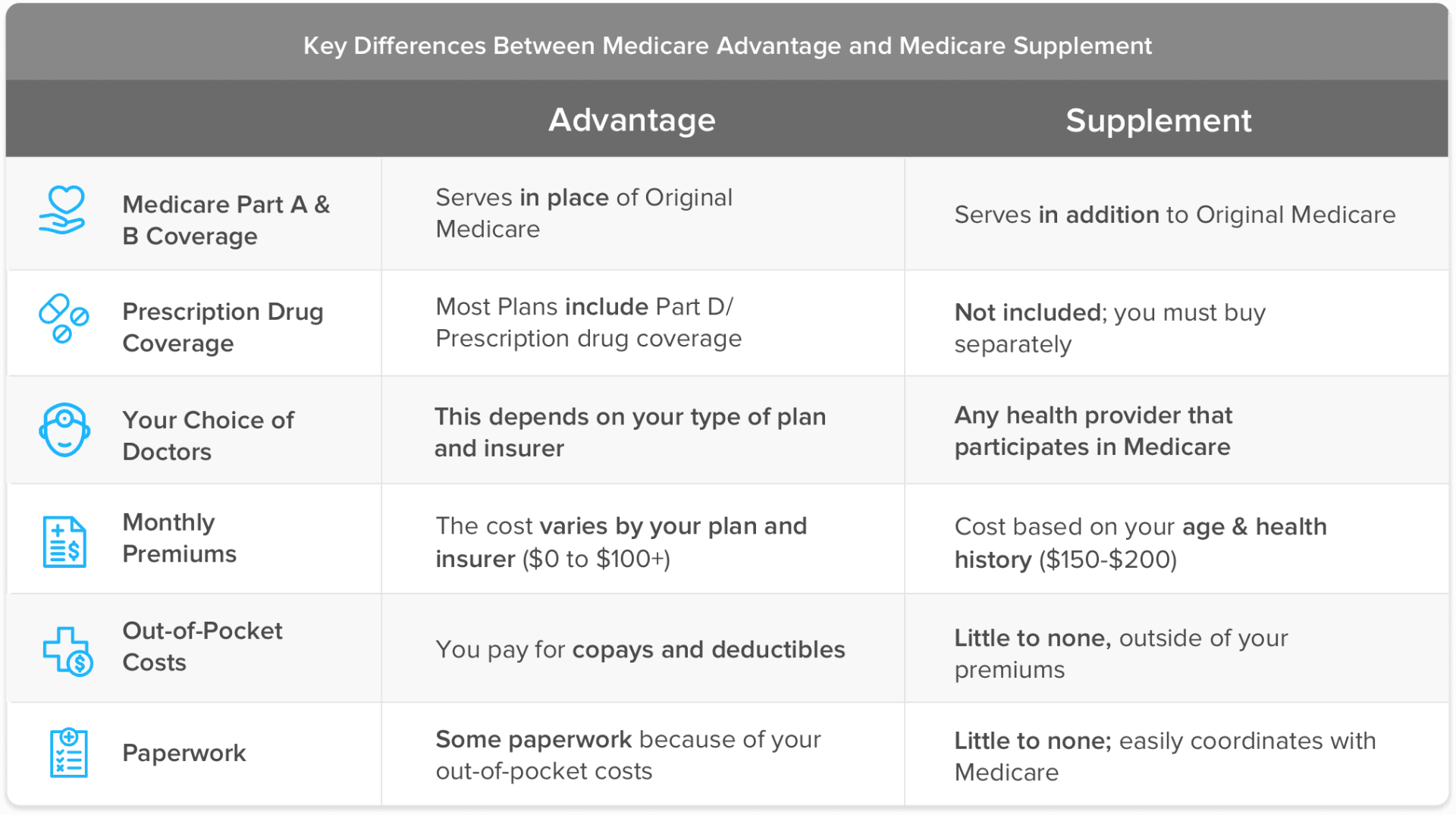
Medigap has some advantages over a Medicare Advantage plan. Medigap plans are mandated to pay their share of the cost when Medicare covers its portion. They also allow you to see any doctor in the United States that accepts Medicare. Further, you don’t need referrals for specialist visits. On the other hand, people under 65 or those on Medicaid ...
When can I disenroll from Medicare Advantage?
Annual enrollment takes place in the fall from October 15 through December 7.
When is Medicare open enrollment?
The Medicare Advantage open enrollment period is one last chance to change your policy for the year. It takes place from January 1 through March 31 each year.
When is the open enrollment period for Medicare?
The Medicare Advantage open enrollment period is one last chance to change your policy for the year. It takes place from January 1 through March 31 each year. There are other enrollment periods available, such as the initial enrollment period for those newly eligible for Medicare.
Can you see a doctor on Medicare?
They also allow you to see any doctor in the United States that accepts Medicare. Further, you don’t need referrals for specialist visits. On the other hand, people under 65 or those on Medicaid could benefit from an Advantage plan.
What is the importance of choosing a Medicare plan?
Choosing a Medicare plan is a very personal process. Your Medicare coverage goes beyond copayments and deductibles. It can determine how prepared you are for emergencies, it can affect the quality of care you receive, and it can alter your lifestyle based on the benefits included.
Do you have to worry about medical underwriting for Medicare?
If you have preexisting conditions and want to switch into a new Medicare Advantage plan, you do not have to worry about medical underwriting . Medicare Supplement (Medigap) plans are the only type of Medicare plan that may require medical underwriting. Original Medicare (parts A and B), Prescription Drug Plans (Part D), and Medicare Advantage plans (Part C) all cannot deny you coverage based on your health history.
How long does it take to switch to Medicare Advantage?
If a person enrolls in Medicare Advantage when they first become eligible for Medicare, they can switch to original Medicare and Medigap within the first 3 months of their plan.
How to disenroll from Medicare Advantage?
It is possible to disenroll from a Medicare Advantage plan by contacting the insurance company directly and requesting a disenrollment form. People can also call Medicare at 800-633-4227 and ask for disenrollment from their plan, or they can visit their local Social Security office.
How to find a Medigap policy?
If a person has never enrolled in a Medigap plan, they can find available Medigap policies by searching on Medicare.gov, contacting a State Health Insurance Assistance Program, or contacting an insurance agent or company to obtain a Medigap quote.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, is a bundled plan that private companies administer. The plans vary based on which medical services are available in a certain area, and people often need to receive treatment from an approved network of healthcare professionals. Learn more here.
Does Medicare cover out of pocket costs?
However, out-of-pocket costs usually include deductibles and coinsurance. Medigap plans, or Medicare supplement plans, are available to help people fund these extra costs. People can enroll in them alongside traditional ...
Does Medicare cover overseas?
Medicare Advantage plans do not usually cover overseas treatment. Medical underwriting: If a person did not enroll in Medigap during their 6-month enrollment period, they may have to complete medical underwriting for an insurance company to cover them. People with preexisting medical conditions may not qualify.
What happens if you leave Medicare Advantage?
Leaving a Medicare Advantage plan simply moves you back to Original Medicare. Having only Original Medicare puts you at considerable risk for catastrophic medical spending if you have a serious illness. Medicare has no cap on your out of pocket expenses.
How long does Medicare Advantage last?
Medicare Advantage plan membership is generally for an entire calendar year. Leaving the plan requires that you have an approved election period to do so. The easiest election period to use is the Annual Election Period which runs from October 15th – December 7th. During this period, members of Advantage plans can move from their current plan ...
Why do people choose Medicare Advantage?
Many people try out Medicare Advantage plans because they offer lower premiums than Medigap. Medicare beneficiaries are also lured by promised of minor extra benefits like vision exams and eyeglasses or gym memberships.
What is an OEP in Medicare?
The Medicare OEP is for beneficiaries to: Switch from one Medicare Advantage plan to another Medicare Advantage plan OR. Disenroll from a Medicare Advantage plan and return to Original Medicare, with or without a Part D drug plan. Outside of these two election periods, there are various special election periods which can qualify a person ...
Does Medicare have a cap on out of pocket expenses?
Medicare has no cap on your out of pocket expenses. For example, someone with cancer will pay 20% for their chemotherapy with no cap to that spending. For this reason, most people returning to Medicare want to also apply for a Medigap plan to supplement their Medicare.
Why do doctors come and go?
Doctors can come and go from the networks as their contracts come up for renewal. If a trusted doctor leaves the network, that beneficiary may want to return to Original Medicare so that he can continue to see that doctor. Other reasons might include frustration with having to get referrals to see a specialist.
How to change to Medicare Advantage?
Changing from Medicare Advantage to Original Medicare is a very simple process once you’re ready and eligible to switch. There are three ways you can make the change: 1 Visit your local Social Security Office and ask to be disenrolled from Medicare Advantage; 2 Call 1-800-MEDICARE (1-800-633-4227) and process your disenrollment over the phone; or 3 Contact your Medicare Advantage insurer directly and request a disenrollment form.
How long does it take to switch from Medicare Advantage to Original Medicare?
If you’re covered by both Medicare and Medicaid and then you lose eligibility for Medicaid, you can switch from Medicare Advantage to Original Medicare up to three months from the date you lose Medicaid eligibility, or the date you’re notified, whichever is later.
When does Medicare open enrollment end?
Medicare Advantage Open Enrollment Period. This special opportunity to leave Medicare Advantage lasts from January 1 through March 31 each year. If you disenroll during January, your changes will be effective on February 1. If you disenroll during February, your changes will be effective on March 1. If you disenroll during March, your changes will ...
When does Medicare Advantage end?
This special opportunity to leave Medicare Advantage lasts from January 1 through March 31 each year. If you disenroll during January, your changes will be effective on February 1. If you disenroll during February, your changes will be effective on March 1. If you disenroll during March, your changes will be effective on April 1.
What is Medicare Supplement Plan?
This kind of plan, also known as a Medigap policy, pays for gaps in Medicare’s coverage. For instance, Medicare Part B pays 80% of covered costs after you pay your annual deductible. A Medigap policy would pay the remaining 20% ...
Can you leave Medicare Advantage if you have TRICARE?
If you enroll in TRICARE, VA coverage, or another plan that offers comprehensive prescription drug benefits – and you have a Medicare Advantage plan that includes prescription drug coverage ( also called MAPD) – then you can leave your Medicare Advantage plan and return to Original Medicare.
Do you have to take extra steps to disenroll in Medicare?
You shouldn’t have to take any extra steps once you disenroll in Medicare Advantage. If you were enrolled in Medicare Advantage, you would have already continued paying your Original Medicare premiums anyway. You may encounter issues, though, when leaving Medicare Advantage.
How long do you have to pay for Medigap?
You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period." The 30-day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
How long do you have to wait to get a Medigap policy?
The Medigap insurance company may be able to make you wait up to 6 months for coverage of pre-existing conditions. The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
What happens if you switch to Medicare Advantage?
If you make the switch to a Medicare Advantage plan, review your Annual Notice of Change every year. Common changes include: Your plan may even go away next year, or stop covering services not included in Medicare Part B.
Does Medicare Advantage work differently?
It works a little differently when you have a Medicare Advantage plan . These more closely resemble traditional health plans, such as those provided by an employer or union, in that you have a network of approved providers. This includes physicians, hospitals, labs, and any other professionals who provide your healthcare.
Do you have to have a primary provider for Medicare Advantage?
Most Medicare Advantage plans require you to choose a primary care physician, particularly HMOs. Of course, you likely have a primary provider now. The difference with an HMO – and some PPOs – is that your primary care physician must provide referrals to a specialist.
Why is Original Medicare so popular?
One of the reasons Original Medicare has such high approval ratings among enrollees is the enormous network of providers that accept Medicare. If you have Original Medicare, you can see any doctor that accepts assignment, even when traveling in another state. It works a little differently when you have a Medicare Advantage plan.
