1-800-557-6059 | TTY 711, 24/7 Check your Medicare enrollment by following these three easy steps: Visit the Check Your Enrollment page on Medicare.gov, the official website for Medicare.
How do I Check my Medicare enrollment?
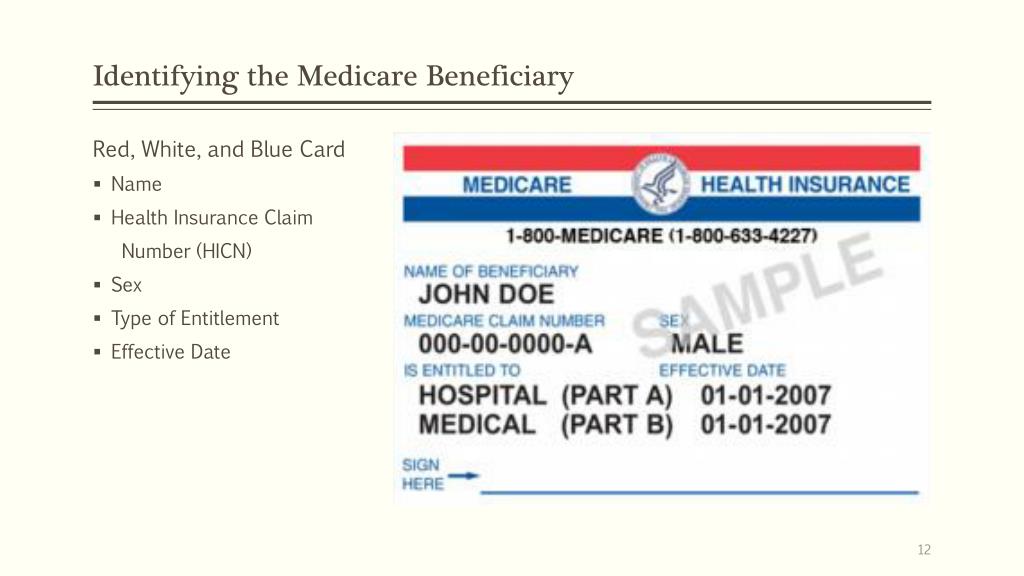
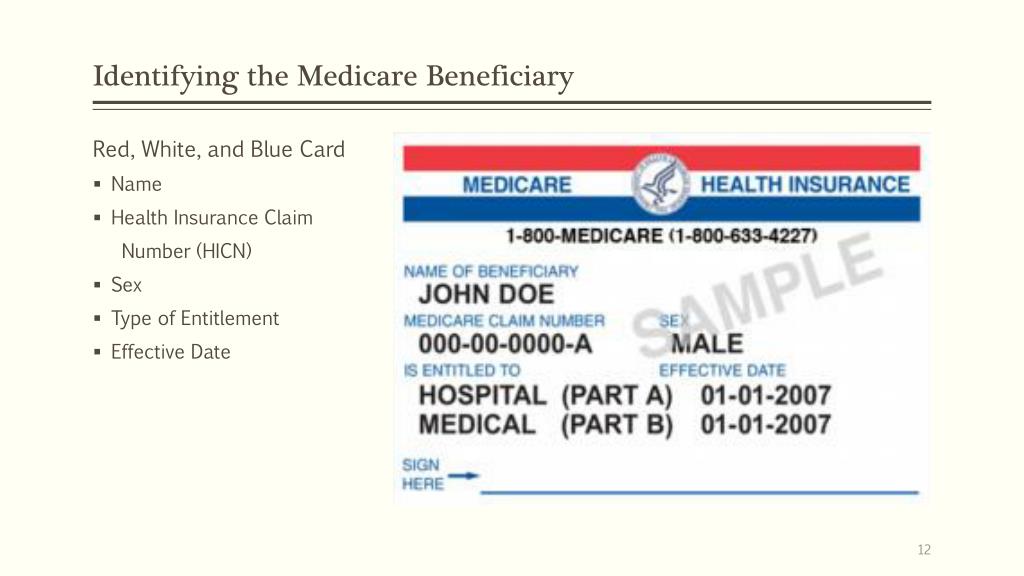
Check your Medicare enrollment by following these three easy steps: Visit the Check Your Enrollment page on Medicare.gov, the official website for Medicare. Fill out the requested information, including your zip code, Medicare number, name, date of birth and your effective date for Medicare Part A coverage or Part B coverage.
Are you automatically enrolled in Medicare Part A and B?
Most people are automatically enrolled in Medicare Part A and Part B once they’ve been collecting Social Security Disability Insurance (SSDI) payments for 24 months. But some people may be eligible for Medicare even sooner.
How do I get Medicare based on disability?
To become eligible for Medicare based on disability, you must first qualify for Social Security Disability Insurance. SSDI pays monthly benefits to people with disabilities who might be limited in their ability to work.
How do I check the status of my Medicare Part D claims?
To check the status of Medicare drug plan (Part D) claims: Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
How do I verify Medicare enrollment?
The status of your medical enrollment can be checked online through your My Social Security or MyMedicare.gov accounts. You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office.
How do I know if I am a Medicare recipient?
Your state's Medicaid office Visit Medicare.gov/contacts, or call 1-800-MEDICARE (1-800-633-4227) and say “Medicaid.” TTY: 1-877-486-2048.
How long does an SSDI recipient wait for their Medicare to start?
Everyone eligible for Social Security Disability Insurance (SSDI) benefits is also eligible for Medicare after a 24-month qualifying period. The first 24 months of disability benefit entitlement is the waiting period for Medicare coverage.
Does Medicare automatically come with disability?
If you're on SSDI benefits, you won't have to pay a Medicare Part A premium. If you are eligible for Medi-Cal and Medicare, you will automatically be enrolled in Medicare Part D.
How can I find my Medicare number?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov PIN. On your homepage, select My card. You'll see your current Medicare card.
What happens to my Medicare disability when I turn 65?
What Happens When You Turn 65? When you turn 65, you essentially lose your entitlement to Medicare based on disability and become entitled based on age. In short, you get another chance to enroll, a second Initial Enrollment Period if you will.
Why does Medicare have a two year waiting period?
The original purposes of the 24month waiting period were to limit costs to the Medicare trust funds at a time when many workers might have other health insurance coverage and to ensure that Medicare protection is extended only to persons whose disabilities are severe and long lasting.
How does disability affect Medicare?
Medicare coverage is the same for people who qualify based on disability as for those who qualify based on age. For those who are eligible, the full range of Medicare benefits are available.
Is there a waiting period after signing up for Medicare?
Initial Enrollment Period – a 7-month period when someone is first eligible for Medicare. For those eligible due to age, this period begins 3 months before they turn 65, includes the month they turn 65, and ends 3 months after they turn 65.
What happens when someone on disability turns 65?
When you reach the age of 65, your Social Security disability benefits stop and you automatically begin receiving Social Security retirement benefits instead. The specific amount of money you receive each month generally remains the same.
Do Social Security disability benefits end at 65?
To put it in the simplest terms, Social Security Disability benefits can remain in effect for as long as you are disabled or until you reach the age of 65. Once you reach the age of 65, Social Security Disability benefits stop and retirement benefits kick in.
Do I lose Medicare if I lose SSDI?
Yes. If you go off SSDI when you return to work you can continue Medicare coverage for 93 months after completing the 9 months work period. Combined with the trial work period, therefore, you can receive Medicare Part A coverage premium-free for a total of 8 and half years.
What conditions are considered to be eligible for Medicare?
Even though most people on Social Security Disability Insurance must wait for Medicare coverage to begin, two conditions might ensure immediate eligibility: end-stage renal disease (ESRD) and Lou Gehrig’s disease (ALS).
When will Medicare be available for seniors?
July 16, 2020. Medicare is the government health insurance program for older adults. However, Medicare isn’t limited to only those 65 and up—Americans of any age are eligible for Medicare if they have a qualifying disability. Most people are automatically enrolled in Medicare Part A and Part B once they’ve been collecting Social Security Disability ...
What is ESRD in Medicare?
ESRD, also known as permanent kidney failure, is a disease in which the kidneys no longer work. Typically, people with ESRD need regular dialysis or a kidney transplant (or both) to survive. Because of this immediate need, Medicare waives the waiting period. 2
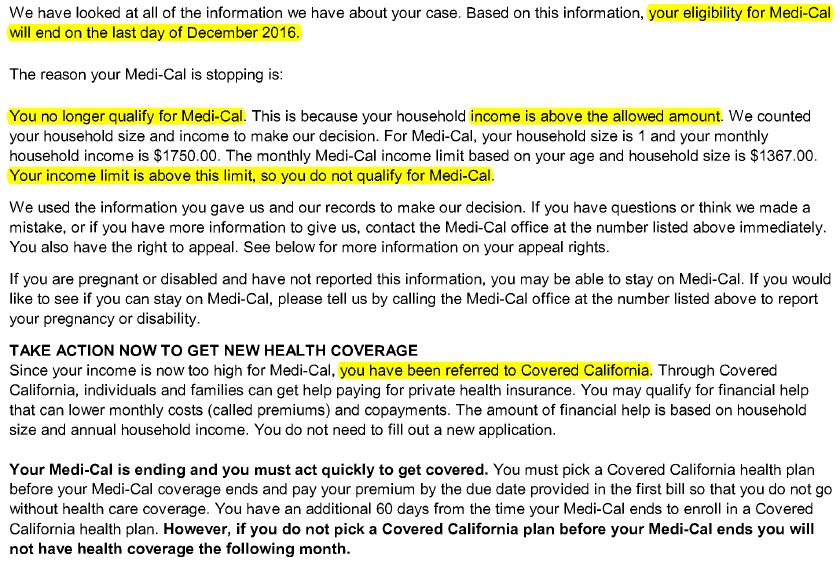
What to do if your income is too high for medicaid?
If your income is too high to qualify for Medicaid, try a Medicare Savings Program (MSP), which generally has higher limits for income. As a bonus, if you qualify for an MSP, you automatically qualify for Extra Help, which subsidizes your Part D costs. Contact your state’s Medicaid office for more information.
How long does it take to get Medicare if you appeal a decision?
The result: your wait for Medicare will be shorter than two years.
How long does a disability last?
The government has a strict definition of disability. For instance, the disability must be expected to last at least one year. Your work history will also be considered—usually, you must have worked for about 10 years but possibly less depending on your age.
Does Medicare cover ALS?
Medicare doesn’t require a waiting period for people diagnosed with ALS, but they need to qualify based on their own or their spouse’s work record. 3
How long do you have to wait to get Medicare if you have Social Security Disability?
Social Security Disability Insurance (SSDI) & Medicare coverage. If you get Social Security Disability Income (SSDI), you probably have Medicare or are in a 24-month waiting period before it starts. You have options in either case.
What is SSI disability?
Supplemental Security Income (SSI) Disability & Medicaid coverage. Waiting for a disability status decision and don’t have health insurance. No disability benefits, no health coverage. The Marketplace application and disabilities. More information about health care for people with disabilities.
Can I enroll in a Medicare Marketplace plan if I have Social Security Disability?
You’re considered covered under the health care law and don’t have to pay the penalty that people without coverage must pay. You can’t enroll in a Marketplace plan to replace or supplement your Medicare coverage.
Can I keep my Medicare Marketplace plan?
One exception: If you enrolled in a Marketplace plan before getting Medicare, you can keep your Marketplace plan as supplemental insurance when you enroll in Medicare. But if you do this, you’ll lose any premium tax credits and other savings for your Marketplace plan. Learn about other Medicare supplement options.
Can I get medicaid if I have SSDI?
You may be able to get Medicaid coverage while you wait. You can apply 2 ways: Create an account or log in to complete an application. Answer “ yes” when asked if you have a disability.
Can I get medicaid if I'm turned down?
If you’re turned down for Medicaid, you may be able to enroll in a private health plan through the Marketplace while waiting for your Medicare coverage to start.
When should I enroll in Medicare?
If you become eligible for Medicare because of a disability and have been receiving Social Security Disability Insurance (SSDI) or railroad disability annuity checks for 24 months, you should automatically be enrolled in both Medicare Parts A and B at the start of your 25th month. You should not have to contact anyone.
Where do Social Security benefits come from?
If you get Social Security retirement benefits, your package and card will come from the Social Security Administration (SSA). If you get railroad disability annuity checks, your package and card will come from the Railroad Retirement Board .
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long do you have to wait to get Medicare?
In most cases, you’ll need to wait 24 months before your Medicare coverage begins. There is a 2-year waiting period that begins the first month you receive a Social Security benefit check.
When does Medicare start covering ALS?
If you have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s Disease, you’ll be enrolled in coverage in the first month you receive SSDI. If you have end stage renal disease (ESRD), your Medicare coverage normally begins after you’ve received 3 months of dialysis treatment.
How much is Medicare Part B 2021?
The standard Part B premium for 2021 is $148.50 per month. The deductible for Medicare Part B in 2021 is $203. After you meet the deductible, some services are covered in full. You’ll pay 20 percent of the Medicare-approved amount for other services.
How much is hospitalization for Medicare Part A 2021?
In 2021, hospitalization costs with Medicare Part A include: Deductible: $1,484 for each benefit period. Days 1–60: after the deductible has been met, inpatient stays will be completely covered until the 60th day the benefit period. Days 61–90: $371 per day coinsurance.
How long does a disability last?
Generally, this means you are unable to work and that your condition is expected to last for at least a year. Medicare doesn’t determine who is eligible for disability coverage.
Can I get Medicare Part B after 24 months?
The takeaway. Medicare coverage is available for people with a disability who receive SSDI. You’ll automatically be enrolled in parts A and B after your 24th month of SSDI benefits. You can choose to decline Medicare Part B coverage if you have other options that work better for your budget.
How long do you have to sign up for Medicare Part D?
You can sign up for a drug plan: Up to three months before you qualify for Medicare. The month you qualify for Medicare.
How many people are eligible for Medicare?
As of 2019, Medicare covered more than 8 million Americans under age 65 with disabilities. You can qualify for Medicare under age 65 if you have end-stage renal disease (ESRD), amyotrophic lateral sclerosis (ALS) or if you’ve received disability benefits for at least 24 months. This guide covers Medicare eligibility requirements for people ...
How old do you have to be to get Medicare?
Depending on the type of disability you have, you may qualify for Medicare under age 65 if you receive disability benefits, though there may be a waiting period.
How long does Medicare Advantage last?
If you’re over 65, this seven-month period starts three months before you turn 65, includes the month you turn 65 and ends three months later.
How long does it take for Medicare to cover end stage renal disease?
You can receive retroactive Medicare coverage that starts up to 12 months before you enroll. You’ll need to enroll in both Medicare Part A and Part B in order to cover dialysis and kidney transplant services.
How long does it take to get Medicare if you are 65?
In some cases, individuals under 65 may qualify for Medicare if they have certain disabilities. Depending on the disability, there may be a 24-month waiting period before individuals can enroll in Parts A and B. Qualified for Social Security retirement benefits and received Social Security Disability Insurance (SSDI) for 24 months.
What does it mean when a doctor certifys you are homebound?
A doctor must certify that you are homebound, which means you’re unable to leave your home without assistance. A doctor must certify that you need part-time skilled nursing care or therapy services. The care must be provided through a Medicare-approved home health agency.