Typically, you would have to log into your account on your insurance provider’s website, and your EOB would be found in the claims-related section. To check the status of your current Medicare claims online, log into your Medicare account and download the claims information.
Full Answer
How long should you keep Medicare EOB?
You can also:
- Add your prescriptions and pharmacies to help you better compare health and drug plans in your area.
- Sign up to get your yearly “Medicare & You” handbook and claims statements, called “Medicare Summary Notices,” electronically.
- View your Original Medicare claims as soon as they’re processed.
- Print a copy of your official Medicare card.
How to get help when you have problems with Medicare?
What To Do If There Is A Medicare Billing Error, Or You Suspect One Occurred
- It could be an accident. Accidents happen—even with billion-dollar government programs. ...
- Make sure you’re not being scammed. On the other hand, an “accident” could disguise itself as fraud. ...
- Check with Social Security. ...
- Fill out the right form. ...
- Know who is billing you. ...
How to get free cell phones for seniors on Medicare?
Tips for choosing the best Lifeline provider:
- Each state has many free cell phone providers, and you have to find out who serves your area.
- One of these companies may offer more free minutes or allow additional low-cost minutes. ...
- Then you have to sign up for the lifeline program on this company website, or you can do that with mobile vendors at street fairs.
How to choose the best Medicare?
How to Choose the Best Medicare Plan in 2019
- Understanding What Medicare Is About and How It Works. Before getting into the details of how to choose an adequate plan, let’s get acquainted with Medicare.
- A Guide on How to Choose the Best Medicare Plan for You. ...
- Conclusion on Choosing the Best Medicare Plan 2019. ...
Can I view my Medicare EOB online?
EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
How do I access my Medicare claims data?
Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information. Learn more about Medicare's Blue Button. For more up-to-date Part D claims information, contact your plan.
How do I access Medicare statements?
If you have received services but have not received an MSN, call 1-800-MEDICARE or access your MSN online by creating or logging into your secure Medicare account at www,medicare.gov/account (however, you should still request a paper copy for your records).
Can I get my Medicare Summary Notice Online?
Yes, Medicare summary notices are available online — but you must sign up to receive them electronically. If you opt for electronic notices, you'll stop receiving printed copies of your MSNs in the mail. Instead, you'll get an email every month from your online My Medicare Account.
Can I download my Medicare claims?
How do I download my Medicare claims data? Log into (or create) your secure Medicare account. Select "Download my claims & personal data" from the drop-down menu under your name. Complete the short online form to pick the data you want and save the file to your computer as a PDF or TXT file.
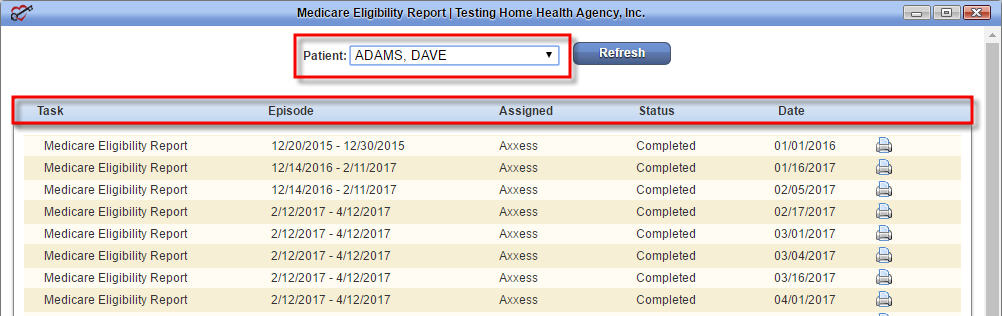
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
How do I check my Medicare payments online?
If you don't already have an account, follow these steps to make one:Visit the MyMedicare.gov account registration page. ... Complete the online account form using your personal data and your Medicare details. ... Check the boxes to show your information is accurate and that you accept the site's rules.More items...•
What is Medicare EOB?
Each month you fill a prescription, your Medicare Prescription Drug Plan mails you an "Explanation of Benefits" (EOB). This notice gives you a summary of your prescription drug claims and costs.
How often are Medicare summary notices mailed?
every 3 monthsIt's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services.
How do I claim Medicare receipts online?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov pin. On your homepage, select Make a claim. Make sure you have details of the service, cost and amount paid to continue your claim.
Claim Status Request and Response | CMS
Providers have a number of options to obtain claim status information from Medicare Administrative Contractors (MACs): • Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
Appeals Status Lookup | HHS.gov
The first thing to know about an Explanation of Benefits is that it’s not a bill. Instead, it’s a summary of the claims and charges applied to your...
Lookup tools | CMS
Anyone enrolled in Medicare Advantage and Medicare Prescription Drug Plan (Part D) will receive an EOB when they use their policy. You don’t need t...
How do I view my EOB online? | Medicare | bcbsm.com
You can expect to see a few standard terms, no matter who sends your Explanation of Benefits. They are:
Checking Claim Status - CGS Medicare
If you misplaced your most recent EOB or didn’t receive it in the mail, contact your insurance company. A representative should be able to provide...
What is an Explanation of Benefits?
No, but you’ll receive a Medicare Summary Notice (MSN), the Medicare explanation of benefits. Like the EOB, the MSN is not a bill — it’s a monthly...
Who Receives an EOB?
If you have a Medicare Prescription Drug EOB, it can show which medicines you’re taking, how much they cost, and how much your insurance covers. [i]
How Do I Read My EOB?
Your insurance company is only required to send you an EOB when you make a claim. This happens any time you see a healthcare provider through your...
Can I Get Another Copy of my EOB?
I’m on Original Medicare (Parts A and B) -- Do I get an EOB?
Does my EOB show specific prescription info?
Will I get an EOB each month if I don't see a doctor?
What Is A Medicare Explanation Of Benefits
First, it is important to understand what a Medicare Explanation of Benefits is. Essentially, it summarizes what items or services you received that were paid for by your Medicare plan. Even if your plan only paid for a part of these items or services, it will show up on your Explanation of Benefits, also known as an EoB.
What Is An Explanation Of Benefits
The first thing to know about an Explanation of Benefits is that its not a bill. Instead, its a summary of the claims and charges applied to your policy from the previous month.
How Long To Keep An Eob
An article from the New York Times recommended keeping your EOB on file for at least one year to track payments, detect discrepancies and verify that bills have been paid in full.
Electronic Medicare & You Handbook
The eHandbook is an electronic version of your trusted “Medicare & You” handbook. You can help save tax dollars by switching to the eHandbook. You’ll get an email with a link to the online PDF of “Medicare & You” instead of getting a paper copy each fall. If you want to get your next fall handbook electronically, sign up by May 31st.
What To Do With The Notice
If you have other insurance, check to see if it covers anything that Medicare didnt.
Checking Your Medicare Eob Online
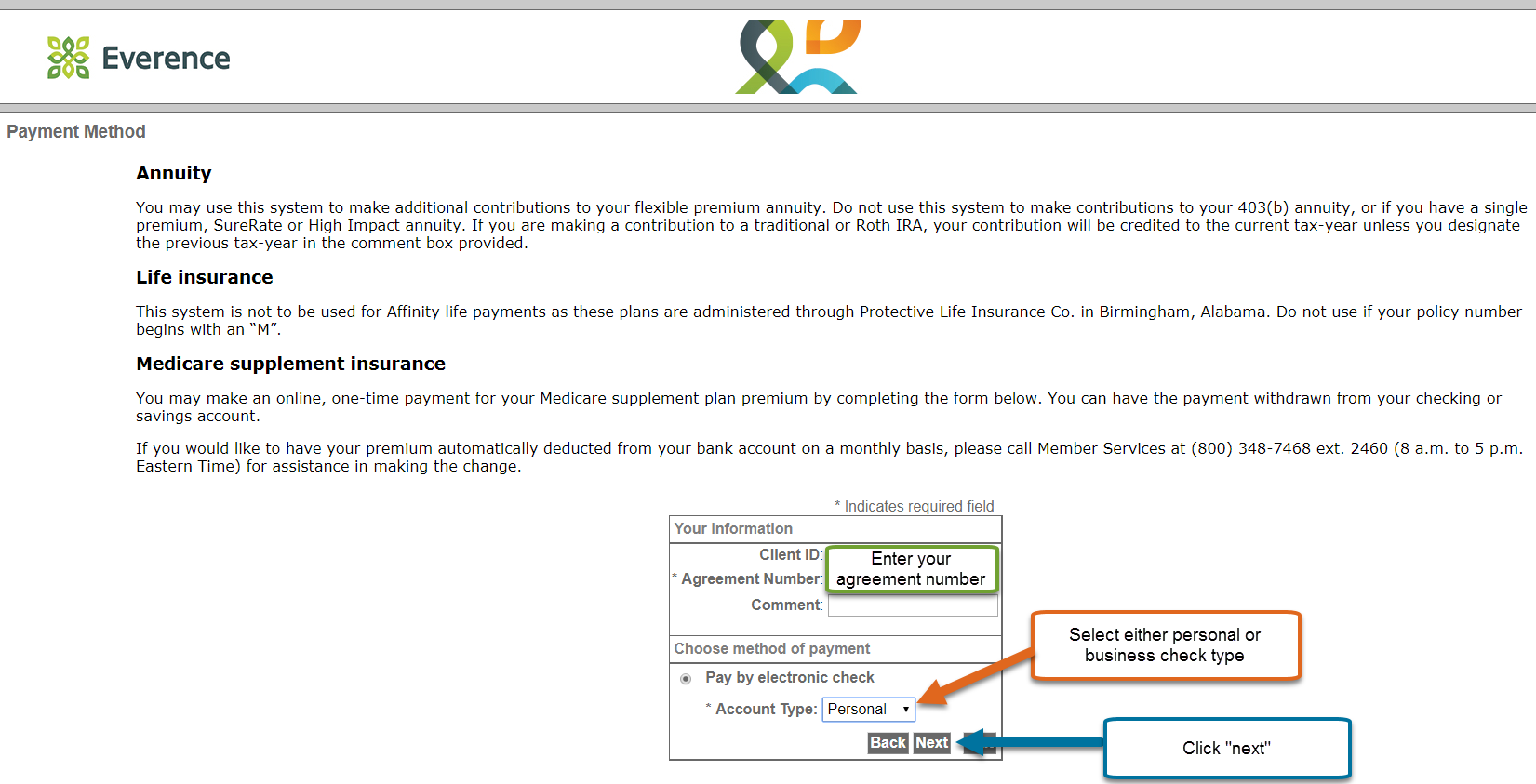
Your plan provider may offer the option to check your EOB online instead of getting them via mail. Your plan provider should have instructions on its website for accessing your EOBs online.
When Do I Need To File Medicare Claim
Original Medicare has both participating and non-participating providers. Participating providers accept Medicares reimbursement plus your coinsurance as full payment, and have agreed to always bill Medicare for your care.
What is EOB in Medicare?
An explanation of benefits (EOB) is a notice from your Medicare provider that you receive monthly or after accessing health care services. It includes a description of your plan, the costs of services, how much your insurer covered and out-of-pocket costs you may have to pay.
How often do you get EOB from Medicare Advantage?
If you enroll in Medicare Advantage plans, you’ll either receive an EOB monthly or on a per-claim basis, along with quarterly summary statements.
What is an EOB?
An EOB summarizes the items and services you accessed, the amount charged to Medicare, how much was covered by Medicare and how much you owe.
How to check Medicare claims?
To check the status of your current Medicare claims online, log into your Medicare account and download the claims information.
When do you get an EOB for Medicare Part D?
Enrollees who have a Medicare Part D plan will get an EOB at the end of every month detailing the covered prescriptions you filled during the previous month. The EOB also includes information on the current payment stage for your plan, which determines how much you’ll pay for drugs covered by the plan.
What to do before filing an appeal with Medicare?
Before filing an appeal, you can also call Medicare customer service to inquire about your denied claims or appoint a representative to file an appeal on your behalf.
How long do you keep EOB?
If you plan to file for medical expense deductions, it’s recommended that you keep your EOB along with other tax documentation for six to seven years.
What is EOB in Medicare?
Explanation of Benefits (EOB) go to enrollees in Medicare Advantage. Medicare Advantage ( Medicare Part C) is health insurance for Americans aged 65 and older that blends Medicare benefits with private health insurance. This typically includes a bundle of Original Medicare (Parts A and B) and Medicare Prescription Drug Plan (Part D).
What is an EOB bill?
For example: If your deductible is $1,000, your insurance company will not cover any costs until you pay the first $1,000 yourself. An EOB is NOT a bill.
What does EOB mean in July?
The EOB you receive in July will reflect the claims and charges from those visits. Your EOB will show what your insurance company has agreed to pay for the services you received. With your EOB, you can check that you’re being charged correctly by your doctors and specialists when you get your bills.
What to do if you misplaced your EOB?
If you misplaced your most recent EOB or didn’t receive it in the mail, contact your insurance company. A representative should be able to provide the information you need and verify your mailing address. Many companies also offer paperless options; if you have an internet connection, you may be able to view your EOB online at any time.
What is an explanation of benefits?
The first thing to know about an Explanation of Benefits is that it’s not a bill. Instead, it’s a summary of the claims and charges applied to your policy from the previous month.
What happens if you don't see your doctor?
This happens any time you see a healthcare provider through your insurance. If you didn’t see your doctor, you probably won’t get an EOB. If you do receive one but haven’t seen a doctor (or filled a prescription) lately, make sure to check it for errors — this can be a helpful tool in spotting fraud on your account.
Do you get an explanation of Medicare benefits each month?
If you have a Medicare Advantage or Medicare Prescription Drug Plan (Part D), you probably receive an explanation of benefits each month. Unfortunately, many people don’t understand how to use this info. With the right knowledge, however, your Explanation of Benefits can be a handy tool.
What is EOB in Medicare?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. You only receive an EOB if you have Medicare Advantage or Part D. An EOB is not the same as a Medicare Summary Notice.
Is EOB the same as Medicare?
An EOB is not the same as a Medicare Summary Notice. It is also important to remember that an EOB is not a bill. EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
Does BCRC process claims?
The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Who does BCRC service?
The BCRC provides customer service to all callers from any source, including, but not limited to, beneficiaries, attorneys/other beneficiary representatives, employers, insurers, providers, and suppliers.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
