
Completing the revalidation process
- Determine which provider is being requested to revalidate. Use the revalidation tab within the application status tool -- confirm if you have been sent a request to revalidate and ...
- View the checklist for required information for revalidation
- Revalidate using internet-based PECOS or CMS-855 paper applications. ...
- Support resources. ...
Full Answer
How to revalidate Medicare?
Revalidation
- Due Dates
- Look-up Tool
- Notification
- Failure to Revalidate
- Application Submission
- Resources
How do I re-enroll in Medicare?
If you're looking to reenroll in Medicare Part B, follow these steps:
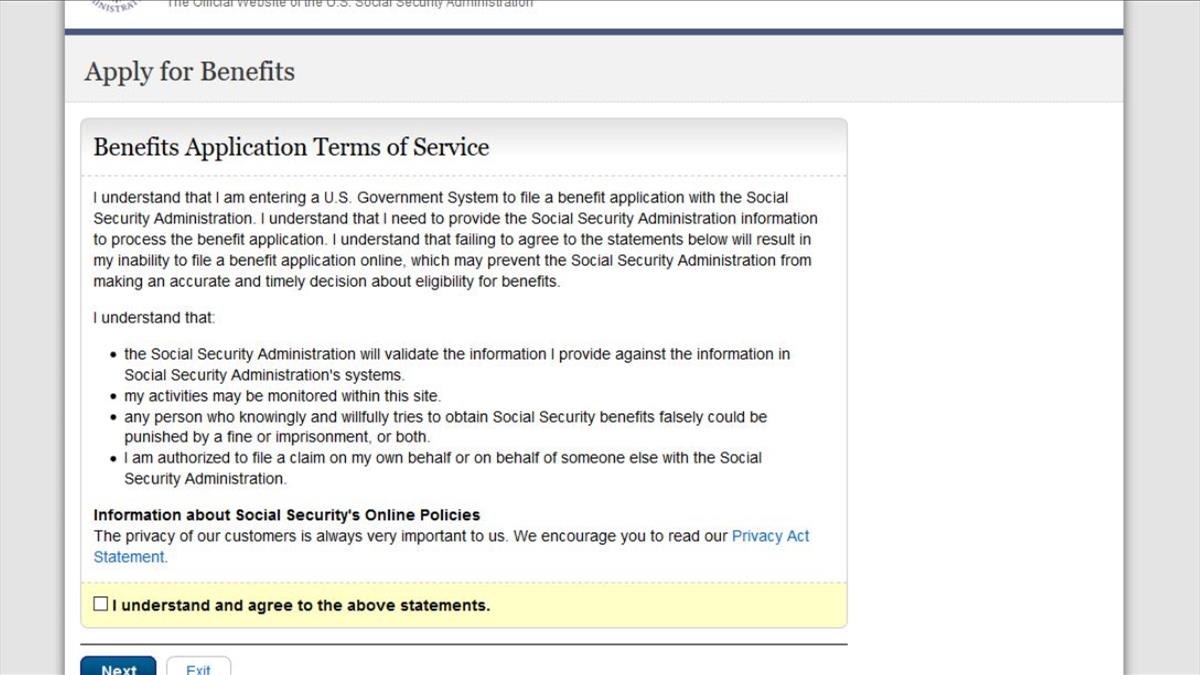
- Go to the Social Security Administration website.
- Complete the application.
- Mail all required documents to the Social Security office. Include all required official or certified documents to allow for a seamless process.
Do I need to re-enroll in Medicaid?
Medicaid can require re-enrollment to prove you are still eligible. Contact your state Medicaid department. While you won't have to re-enroll in Medicaid during open enrollment. You can re-apply or re-enroll at any time of the year. Usually you'll be prompted to "re-prove" your eligibility.
How to get Medicare certified?
- Ambulatory surgery centers
- Community mental health centers
- Comprehensive outpatient rehabilitation facilities
- Critical access hospitals
- End-stage renal disease facilities
- Home health agencies
- Home infusion therapy suppliers
- Hospices
- Hospitals
- Intermediate care facilities for individuals with intellectual disabilities
What forms are needed for Medicare revalidation?
How do I revalidate my Medicare file? You will need to submit a complete CMS-20134, CMS-855A, CMS-855B, or CMS-855I application, depending on your provider / supplier type. If you enrolled in more than one state in our jurisdiction, you are required to submit a separate application for each state.
How do I reactivate my Medicare enrollment?
If your Medicare billing privileges are deactivated, you'll need to re-submit a complete Medicare enrollment application to reactivate your billing privileges....It allows you to:Review information currently on file.Upload your supporting documents.Electronically sign and submit your revalidation online.
How often is Medicare revalidation required?
every 5 yearsAll providers and suppliers are required to revalidate their enrollment information every 5 years and every 3 years for DMEPOS suppliers. CMS also reserves the right to request off-cycle revalidations. 24.
What is Medicare revalidation?
The Patient Protection and Affordable Care Act established a requirement for all enrolled providers/suppliers to revalidate their Medicare enrollment information roughly every five years. Revalidation is the process of reviewing all information that is on file with Medicare is correct.
How do I revalidate on Pecos?
1:057:06So to do this just submit an initial enrollment. You'll need to click on the new application buttonMoreSo to do this just submit an initial enrollment. You'll need to click on the new application button shown on the previous screen. And then this submission is what will count towards your revalidation.
Why would my Medicare be inactive?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
What is the revalidation process?
Revalidation is an evaluation of your fitness to practise. This process: supports doctors in regularly reflecting on how they can develop or improve their practice. gives patients confidence doctors are up to date with their practice. promotes improved quality of care by driving improvements in clinical governance.
How do I know when my revalidation is due?
Your revalidation application is due on the first day of the month in which your registration expires. For example, if your renewal date is 30 April, your revalidation application date will be 1 April. You can find out your renewal date by checking your NMC Online account.
What is meant by revalidation?
Definition of revalidate transitive verb. : to validate again or anew: such as. a : to make (something) legal or valid again Her mother had revalidated her Cuban teaching credentials and begun teaching school.— Linda Marx also : to grant official sanction to (something) again had to get his visa revalidated.
Does Medicare expire?
As long as you continue paying the required premiums, your Medicare coverage (and your Medicare card) should automatically renew every year. But there are some exceptions, so it's always a good idea to review your coverage every year to make sure it still meets your needs.
Does Ptan expire?
Inactive PTAN s are Deactivated A is given an end-date when it is deactivated, meaning claims can get submitted prior to the end-date within a year of the service date.
How do I call Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
What is Medicare revalidation?
Revalidation is a complete and thorough re-verification of the information contained in your Medicare enrollment record to ensure it is still accurate and compliant with Medicare regulations. Simply put, revalidation is re-enrollment. All providers and suppliers are required to revalidate their enrollment information every five years.
How to revalidate a provider?
1. Determine which provider is being requested to revalidate. Use the revalidation tab within the application status tool -- confirm if you have been sent a request to revalidate and to which provider the request applies. 2. View the checklist for required information for revalidation. Take advantage of this helpful checklist to ensure ...
How to revalidate a CMS 855?
Revalidate in a few simple steps. 1. Determine which provider is being requested to revalidate. 2. View the information checklist. 3. Revalidate using internet-based PECOS or by completing the appropriate CMS-855 application. 4. Support resources.
How often do you have to revalidate First Coast?
First Coast Service Options must receive your enrollment application within 60 days of the revalidation request.
How often do Medicare providers revalidate?
Generally, physicians and NPPs revalidate enrollment every 5 years or when CMS requests it. What is being Revalidated.
What does TBD mean in revalidation?
Provider/suppliers not due for revalidation will display a "TBD" (To Be Determined) in the due date field. This means that you do not yet have a due date for revalidation. Please do not submit a revalidation application if there is NOT a listed due date. Where is Revalidation sent to.
How often does Medicare require revalidation?
Medicare requires all enrolled providers and suppliers to revalidate enrollment information every five years. To ensure compliance with these requirements, existing regulations at 42 CFR §424.515 (d) provide that (CMS is permitted to conduct off-cycle revalidations for certain program integrity purposes). 2.
Do I need to submit a CMS-855A?
You will need to submit a complete CMS-20134, CMS-855A, CM S-855B or CMS-855I application, depending on your provider / supplier type. If you enrolled in more than one state in our jurisdiction, you are required to submit a separate application for each state.
Does revalidation change enrollment?
No, the revalidation effort does not change other aspects of the enrollment process. Continue to submit changes (i.e., change of ownership, change in practice location or reassignment, final adverse action, etc.) as you always have. If you also receive a request for revalidation, respond separately to that request.
Do you need separate revalidation applications for each state?
If this occurs, separate revalidation applications are required for each state in which you must revalidate. If someone is completing the application on behalf of an individual provider, that person is strongly encouraged to coordinate with all groups / entities to ensure all reassignments remain intact. 10.
Can you use PECOS for revalidation?
If you wish to use internet-based PECOS to submit your revalidation application, you will have to select ‘ New Enrollment’ and complete the application under this scenario. You can also complete the paper application, which does allow you to select ‘Revalidation’ as a submission reason.
How long does it take for Medicare to be revalidated?
If an application is submitted before seven months, it will be returned as unsolicited. If application changes any of Medicare information, changes will occur but will not revalidate the enrollment. Another application must be submitted within seven months of due date.
How often do you have to revalidate Medicare?
The Patient Protection and Affordable Care Act established a requirement for all enrolled providers/suppliers to revalidate their Medicare enrollment information roughly every five years. Revalidation is the process of reviewing all information that is on file with Medicare is correct. All information can be found in CMS Internet Only ...
What happens if there is no space at the end of NPI?
If there is no space at end of NPI, and no due date populates, enrollment is not requested to revalidate at this time. If enrollment has revalidated successfully, or application is still in processing, due date will still populate on website.
How long before Noridian due date?
Reminder Emails. Noridian will also send out a reminder email roughly four months before due date. If correspondence email address is valid, another email will be sent a month and a half before due date again. This will be a generic email stating that your enrollment is due for revalidation.
Does Noridian require documentation for Medicare?
Noridian will process the application as if it were a new enrollment. If supporting documentation currently exists in supplier's file, supplier is not required to submit that documentation again during enrollment process. Application must be fully completed for enrollment to be active in Medicare.
