Also, to keep your costs lower, we suggest making sure your doctor accepts Medicare assignment. There are several other examples of coverage for plastic surgery that will be approved due to medical necessity. In some cases, your doctor needs to write a letter to explain the procedure’s medical necessity.
Full Answer
What does it mean when doctors accept Medicare?
Doctors who accept Medicare are either a participating doctor, non-participating doctor, or they opt-out. When it comes to Medicare’s network, it’s defined in one of three ways. Participating Provider: Providers that accept Medicare Assignment agree to accept what Medicare establishes per procedure, or visit, as payment in full.
How do I find a doctor that accepts Medicare assignment?
To find doctors approved by Medicare you can visit the Medicare website tool to search for a doctor. Here you can find all the doctors who accept assignment near your area. You can narrow down your search to find a doctor who offers all the services you need near you and accepts Medicare assignment.
What types of doctors accept Medicare?
Doctors who accept Medicare are either a participating doctor, non-participating doctor, or they opt-out. When it comes to Medicare’s network, it’s defined in one of three ways.
How hard is it to find a doctor that accepts Medicare?
The good news is that it shouldn’t be too hard to find a participating doctor. Only about 4% of American doctors don’t accept Medicare. And if you’re a Medicare beneficiary, as you can see, provider enrollment can make a huge difference, primarily for your pocketbook.
Why do some doctors refuse Medicare?
Can Doctors Refuse Medicare? The short answer is "yes." Thanks to the federal program's low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare's payment for services. Medicare typically pays doctors only 80% of what private health insurance pays.
Does Medicare have to approve surgery?
Understanding Medicare Surgery Coverage A procedure must be considered medically necessary to qualify for coverage. This means the surgery must diagnose or treat an illness, injury, condition or disease or treat its symptoms.
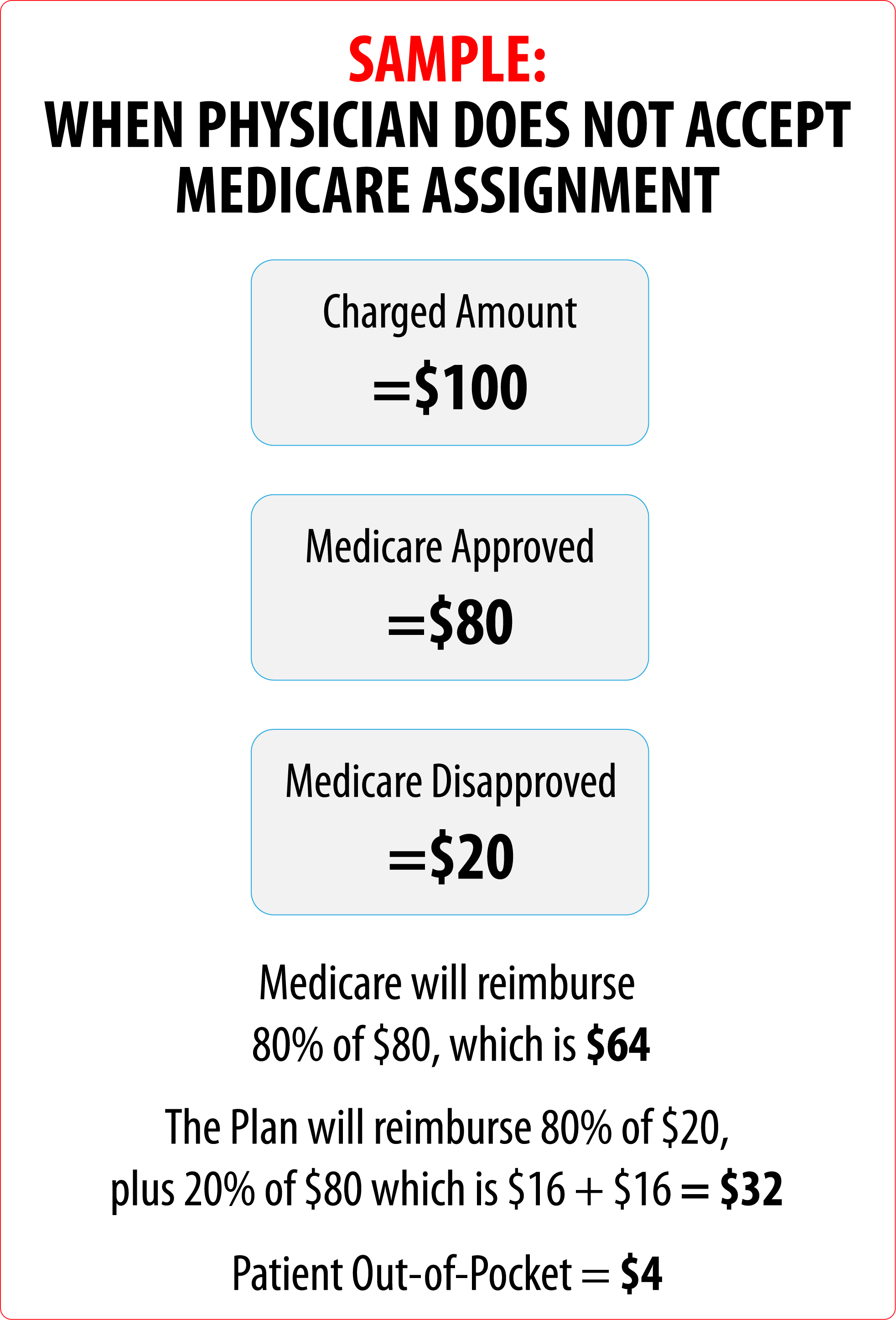
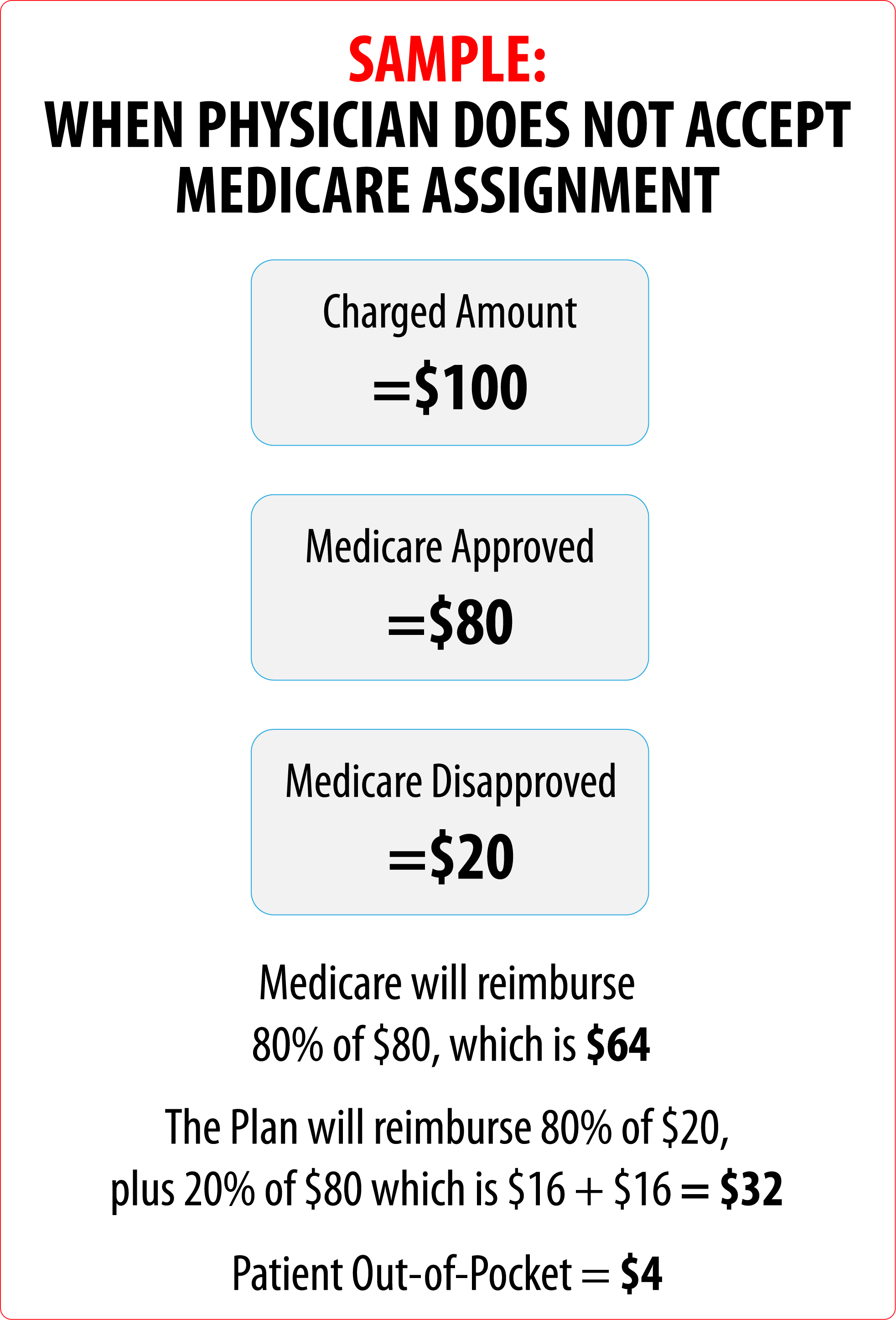
What does it mean if a doctor does not accept Medicare assignment?
A: If your doctor doesn't “accept assignment,” (ie, is a non-participating provider) it means he or she might see Medicare patients and accept Medicare reimbursement as partial payment, but wants to be paid more than the amount that Medicare is willing to pay.
How does Medicare decide what is medically necessary?
According to Medicare.gov, health-care services or supplies are “medically necessary” if they: Are needed to diagnose or treat an illness or injury, condition, disease (or its symptoms). Meet accepted medical standards.
How long does Medicare take to approve a surgery?
Usually, your medical group or health plan must give or deny approval within 3-5 days. If you need an urgent appointment for a service that requires prior approval, you should be able to schedule the appointment within 96 hours. Be sure you understand exactly what services are covered by a referral and prior approval.
Does Medicare require preauthorization for surgery?
Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Can a provider refuse to bill Medicare?
In summary, a provider, whether participating or nonparticipating in Medicare, is required to bill Medicare for all covered services provided. If the provider has reason to believe that a covered service may be excluded because it may be found not to be reasonable and necessary the patient should be provided an ABN.
How do you justify medical necessity?
Well, as we explain in this post, to be considered medically necessary, a service must:“Be safe and effective;Have a duration and frequency that are appropriate based on standard practices for the diagnosis or treatment;Meet the medical needs of the patient; and.Require a therapist's skill.”
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
What are the criteria used to determine medical necessity?
The determination of medical necessity is made on the basis of the individual case and takes into account: Type, frequency, extent, body site and duration of treatment with scientifically based guidelines of national medical or health care coverage organizations or governmental agencies.
How to know how much to pay for surgery?
For surgeries or procedures, it's hard to know the exact costs in advance. This is because you won’t know what services you need until you meet with your provider. If you need surgery or a procedure, you may be able to estimate how much you'll have to pay. You can: 1 Ask the doctor, hospital, or facility how much you'll have to pay for the surgery and any care afterward. 2 If you're an outpatient, you may have a choice between an ambulatory surgical center and a hospital outpatient department. 3 Find out if you're an inpatient or outpatient because what you pay may be different. 4 Check with any other insurance you may have to see what it will pay. If you belong to a Medicare health plan, contact your plan for more information. Other insurance might include:#N#Coverage from your or your spouse's employer#N#Medicaid#N#Medicare Supplement Insurance (Medigap) policy 5 Log into (or create) your secure Medicare account, or look at your last "Medicare Summary Notice" (MSN)" to see if you've met your deductibles.#N#Check your Part A#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#if you expect to be admitted to the hospital.#N#Check your Part B deductible for a doctor's visit and other outpatient care.#N#You'll need to pay the deductible amounts before Medicare will start to pay. After Medicare starts to pay, you may have copayments for the care you get.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. if you expect to be admitted to the hospital. Check your Part B deductible for a doctor's visit and other outpatient care.
Can you know what you need in advance with Medicare?
Your costs in Original Medicare. For surgeries or procedures, it's hard to know the exact costs in advance. This is because you won’t know what services you need until you meet with your provider. If you need surgery or a procedure, you may be able to estimate how much you'll have to pay. You can:
What Happens if a Doctor Doesn’t Accept Medicare Assignment?
Not all doctors accept assignment, this means you pay for services out of pocket. You could pay 100% out of pocket, then wait for Medicare reimbursement. Please keep in mind, there’s no reimbursement guarantee. Then there are doctors who opt out of Medicare charges. This means you pay 100%. Unlike doctors that accept assignment, these doctors don’t set their fees to Medicare standards. This is why you should always confirm first whether your doctor accepts the assignment or not.
What happens if a provider refuses to accept Medicare?
However, if a provider is not participating, you could be responsible for an excess charge of 15% Some providers refuse to accept Medicare payment altogether; if this is the situation, you’re responsible for 100% of the costs.
What is Medicare Assignment of Benefits?
The assignment of benefits is when the insured authorizes Medicare to reimburse the provider directly. In return, the provider agrees to accept the Medicare charge as the full charge for services. Non-participating providers can accept assignments on an individual claims basis. On item 27 of the CMS-1500 claim form non participating doctors need to check “yes” when they agree to accept Medicare assignment for the full charge on the claim.
What is a Medicare Opt-Out Private Contract?
This usually happens with doctors who do not have an agreement with Medicare. A Medicare private contract is for doctors that opt-out of Medicare payment terms. Once you sign a contract, it means that you accept the full amount on your own, and Medicare can’t reimburse you. Signing such a contract is giving up your right to use Medicare for your health purposes.
How to avoid excess charges on Medicare?
You can avoid excess charges by visiting a provider who accepts Medicare & participates in Medicare assignment. If your provider does not accept Medicare assignment, you can get a Medigap plan that will cover any excess charges. Not all Medigap plans will cover excess charges, but some do.
What does it mean to accept Medicare assignment?
Accepting assignment means your doctor agrees to the payment terms of Medicare. Doctors who accept Medicare are either a participating doctor, non-participating doctor, or they opt-out. When it comes to Medicare’s network, it’s defined in one of three ways. Participating Provider: Providers that accept Medicare Assignment agree to accept ...
What does it mean when you sign a contract with Medicare?
Once you sign a contract, it means that you accept the full amount on your own, and Medicare can’t reimburse you. Signing such a contract is giving up your right to use Medicare for your health purposes.
How to confirm Medicare coverage before an appointment?
You can do this by calling the doctor’s office and providing your Medicare information.
What happens if a doctor doesn't accept Medicare?
If your doctors hasn’t signed an agreement to accept assignment for all Medicare-covered services, they are considered a non-participating provider. This means that they are enrolled in a Medicare program but can choose whether or not to accept the assignment, which is the approved amount Medicare will pay for a service.
What is the maximum amount of Medicare coinsurance?
This is the maximum amount that can be charged to Medicare patients after the 20 percent coinsurance. Some doctors may require some or all of these payments at the time of your appointment, while others may send a bill afterward.
How much more do you have to pay for a Medicare prescription?
This may mean you have to pay up to 15 percent more than the Medicare-approved rate for a service.
Do non-pediatrics take Medicare?
The simple answer to this question is yes. Ninety-three percent of non-pediatric primary care physicians say they accept Medicare, comparable to the 94 percent that accept private insurance. But it also depends on what type of Medicare coverage you have, and whether you’re already a current patient.
What is Medicare Advantage Plan Referral?
Medicare Advantage Plan Referral Requirements. Medicare works with private insurers to offer Medicare recipients more choices for coverage. These Medicare Advantage plans must provide the same benefits as Original Medicare, but they often include additional benefits and have their own specific provider network.
What is the primary care physician?
The function of a primary care physician is to help you establish health needs and then help you maintain common health goals and preventive care. An appointment with your primary care doctor is typically your first step in addressing any chronic or acute symptoms.
How many specialty and subspecialty branches of medical practice are there?
In those situations, your primary care doctor will refer you to a specialist. According to the Association of American Medical Colleges (AAMC), there are over 120 specialty and subspecialty branches of medical practice.
Do you need to consult a representative for insurance?
Each insurer can have policies that differ from these general guidelines, so it may be necessary to consult with a representative for your specific plan to verify their policy with regard to specialist referrals.
Do you need a referral for a special needs plan?
Special Needs Plans (SNPs). Some common yearly screenings and exams performed by specialists may not require a referral, but most do. As with other plans, non-emergency specialists must be in-network providers in order to qualify for coverage.
How to find a doctor who accepts Medicare?
You can search by entering a health care professional’s last name or group practice name, a medical specialty, a medical condition, a body part, or an organ system. This tool will provide you with a list of professionals or group practices in the specialty and geographic area you specify, along with detailed profiles, maps and driving directions.
Does Physician Compare accept Medicare?
Please note that Physician Compare only lists professionals that accept Medicare. Although some may also accept Medicaid, it does not have information about which professionals do accept Medicaid.
What are the benefits of choosing a doctor who accepts Medicare?
Benefits of Choosing a Doctor Who Accepts Medicare. When you use a doctor who accepts Medicare, you’ll know exactly what to expect when you pay the bill. An enrolled provider won’t charge more than the Medicare-approved amount for covered services.
How many doctors don't accept Medicare?
Only about 4% of American doctors don’t accept Medicare. And if you’re a Medicare beneficiary, as you can see, provider enrollment can make a huge difference, primarily for your pocketbook.
What is an opt out provider?
Opt-Out Providers will bill you out of pocket in any amount for services in full; the charge limit does not apply. They require a private contract between patient and provider agreeing that neither will receive reimbursement from Medicare for services provided.
What happens if you opt out of Medicare Supplement?
If you use a Medicare Supplement plan, your benefits won’t cover any services when your provider has opted out of Medicare. When you see a non-participating provider, you may have to pay the “limiting charge” in addition to your copay. The limiting charge can add up to 15% of the Medicare-approved amount to your bill.
How much does a limiting charge add to Medicare?
The limiting charge can add up to 15% of the Medicare-approved amount to your bill. If your provider has opted out of Medicare, the limiting charge does not apply, and your provider can bill any amount he or she chooses. Of course, Medicare provider enrollment is just one of the things you’ll need to consider when you choose a doctor.
Do you have to wait for Medicare to pay you?
Most of the time, providers who accept Medicare will wait for Medicare to make payment on a claim before collecting your portion of the bill.
Do Medicare enrollees have to accept Medicare?
Medicare-Enrolled Providers will only charge the Medicare-approved amount for covered services and often cost less out of pocket than services from doctors who don’t accept Medicare. Non-Participating Providers have no obligation to accept the Medicare-approved amount. However, they can choose to do so for any service.
What to ask before setting an appointment for a medical visit?
Before you set the appointment for your medical visit, ask the doctor’s office, if they are accepting new Medicare patients?
How to get a 1490s form?
Call 1/800-MEDICARE (633-4227) and ask for Form CMS-1490S or go to medicare.gov/medicareonlineforms.
Do doctors accept Medicare?
Look for a doctor or specialist that does take Medicare assignment and will bill Medicare. There are plenty of doctors and healthcare professionals that still accept and bill Medicare and are accepting new Medicare patients. Even top in their specific medical field specialists still take Medicare.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.