Resolving Rejected Home Health Claims Caused by Billing Errors
- Tips for Avoiding Claims from Rejecting. Always check a beneficiary's eligibility using the ELGH or ELGA eligibility systems prior to admission and billing Medicare.
- Resubmitting a New Claim. ...
- Electronically Adjusting a Rejected Claim. ...
- Submitting a Paper Claim Adjustment. ...
How to fight a Medicare claim rejection?
Nov 07, 2020 · How do I correct a rejected Medicare claim? Claims rejected as unprocessable cannot be appealed and instead must be resubmitted with the corrected information. The rejected claim will appeal on the remittance advice with a remittance advice code of MA130, along with an additional remark code identifying what must be corrected before resubmitting …
What to do if Medicare denies your medical claim?
Mar 30, 2016 · They also do not qualify for a Clerical Error Reopening (CER). You can only correct a rejected or unprocessable claim by submitting a new claim with the correct information. Identifying an Unprocessable Claim. You can identify an unprocessable claim by the reason and remark codes that appear on the remittance advice.
What if Medicare denies my claim?
Jan 21, 2020 · To access this screen: Log on to FISS At the Main Menu screen, enter "01" and press
How to prevent your insurance claim from being rejected?
• Submit only reports relevant to the denial on claim • Do not submit patient’s entire hospital stay Critical care • Submit notes for NP or specialty denied on claim • Total time spent by provider performing service Anesthesia • Submit only those reports and records that apply to case What documents are needed? 17

What happens when Medicare rejects a claim?
If Medicare refuses to pay for something, they send you a “denial” letter. The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
What is required on a Medicare corrected claim?
Claim adjustments must include: TOB XX7. The Document Control Number (DCN) of the original claim. A claim change condition code and adjustment reason code.Jul 24, 2019
How do you correct a claim?
Make Changes, Add Reference/Resubmission Numbers, and Then Resubmit: To resolve a claim problem, typically you will edit the charges or the patient record, add the payer claim control number, and then resubmit or “rebatch” the claim.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.Jan 6, 2022
Tips For Avoiding Claims from Rejecting
1. Always check a beneficiary's eligibility using the ELGH or ELGA eligibility systems prior to admission and billing Medicare. Access Chapter 2 -...
Electronically Adjusting A Rejected Claim
If the original claim information has posted to the CWF (TPE-TO-TPE field is blank), you will need to adjust the original claim. Resubmitting a new...
Submitting A Paper Claim Adjustment
In the rare circumstance that an electronic adjustment is not possible, the alternative option is to submit a paper adjustment (UB-04). Because the...
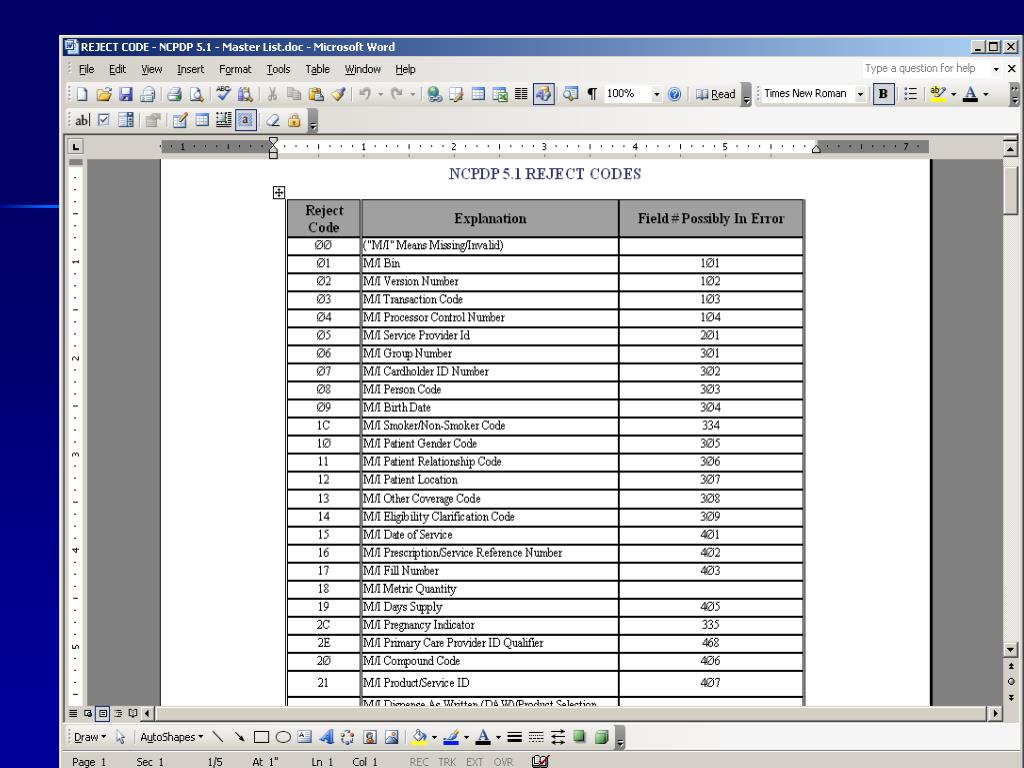
What does "missing" mean in insurance?
Definition: Missing/incomplete/invalid health insurance claim number . The patient's health insurance claim number (Medicare Number) on the claim is not correct. Please contact the patient to verify that the number has not changed and that, and the suffix has not changed.
What is the M77 code?
Remarks Code: M77. Definition: Missing/incomplete/invalid place of service. Medicare requires a two-digit place of service (POS) code on all claims submitted. The POS code represents where the services actually took place (i.e. the physical location of the service).
What is the reason for CO16?
Reason Code: CO16#N#Definition: Claim/service lacks information which is needed for adjudication.# N#Remarks Code: MA04#N#Definition: Secondary payment cannot be considered without the identity of or payment information from the primary payer. The information was either not reported or was illegible.
Is CPT a warranty?
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT.
Is CPT copyrighted?
End User Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association (AMA).
Tips for Avoiding Claims from Rejecting
Always check a beneficiary's eligibility using the ELGH or ELGA eligibility systems prior to admission and billing Medicare. Access Chapter 2 - Checking Beneficiary Eligibility of the Fiscal Intermediary Standard System (FISS) Guide for more information about verifying eligibility information for Medicare beneficiaries.
Resubmitting a New Claim
If the claim information did not post to the CWF, submit a new claim with corrected information. Typically, home health claims that overlap a beneficiary's hospice election or a Medicare Advantage (MA) Plan enrollment period do not post information to CWF when they reject.
Electronically Adjusting a Rejected Claim
If the original claim information has posted to the CWF (TPE-TO-TPE field is blank), you will need to adjust the original claim. Resubmitting a new claim may cause the claim to reject as a duplicate.
Submitting a Paper Claim Adjustment
In the rare circumstance that an electronic adjustment is not possible, the alternative option is to submit a paper adjustment (UB-04). Because the rejected claim posted the episode information out on CWF, HHAs should not submit a new Request for Anticipated Payment (RAP) for the episode prior to submitting the adjustment.
What is a CER in insurance?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
How many levels of appeals are there?
All appeals must be made in writing, and there are five appeal levels a provider can pursue: Level 1 – Redetermination by a Medicare Administrative Contractor (MAC) Level 2 – Reconsideration by a Qualified Independent Contractor (QIC) Level 3 – Decision by Office of Medicare Hearings and Appeals (OMHA)
Is "rejection" a synonym for "denial"?
Let’s face it: rejections and denials don’t sound all that different. In fact, if you look up “denial” in a thesaurus, “rejection” is listed among the acceptable synonyms. But in Medicare parlance, the two words mean different things.
Who is Charity Singleton?
Charity Singleton Craig is a freelance writer and editor who provides communications and marketing services for CIPROMS. She is responsible for creating, editing, and managing all content, design, and interaction on the company website and social media channels in order to promote CIPROMS as a thought leader in healthcare billing and management.
Can a rejected claim be appealed?
Claims rejected as unprocessable cannot be appealed and instead must be resubmitted with the corrected information. The rejected claim will appeal on the remittance advice with a remittance advice code of MA130, along with an additional remark code identifying what must be corrected before resubmitting the claim.
Do Medicare claims have to be processed correctly?
Ideally, claims submitted to Medicare are always entered and processed correctly and then paid on time according to the Medicare fee schedule. But since we live in the real world, where mistakes can and do happen at any point in the billing process, here are four tips to help you identify and correct billing errors on Medicare claims.