How to check Medicare EOB?
Explanation of Benefits (EOB) go to enrollees in Medicare Advantage and Medicare Prescription Drug Plan (Part D) EOBs show the claims and charges applied to your policy the previous month. EOBs offer detailed breakdowns of the costs, including the full price of services, amounts covered by your policy, and what you owe.
Does Medicare send EOB?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. It tells you how much your provider billed Medicare, the Medicare-approved amount your plan will pay, and how much you have to pay the provider. An EOB is not a bill.
Where to find Medicare EOB?
- Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
- Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
- Some providers can enter claim status queries via direct data entry screens.
What does EOB stand for?
Six weeks after his last visit, Frank received an EOB with the following information: 2
- Patient: Frank F.
- Insured ID Number: 82921-804042125-00 – Frank’s Medicare Advantage Plan Identification Number
- Claim Number: 64611989 – the number assigned to this claim by Frank’s Medicare Advantage Plan
- Provider: David T. ...
- Type of Service: Follow-Up Office Visit
- Date of Service: 1/21/20 – the day that Frank had on an office visit with Dr. ...
How do I get an explanation of benefits from Medicare?
claims:Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. ... Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information. ... For more up-to-date Part D claims information, contact your plan.
How do you explain Explanation of Benefits?
How to read an EOBYour patient details.The medical services you received and from who.Amount billed: Cost of those services.Discounts: Any money you saved by accessing care or medical products from within your plan's network of providers.Amount paid by your health insurance plan.More items...
Does Medicare send EOBs to providers?
(If you are enrolled in a Medicare Advantage plan, you will receive an Explanation of Benefits (EOB) if you get care covered by your plan.) The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the three-month period.
Is a Medicare Summary Notice the same as an EOB?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. You only receive an EOB if you have Medicare Advantage or Part D. An EOB is not the same as a Medicare Summary Notice.
How do you interpret EOB benefits?
How to read your EOBProvider—The name of the doctor or specialist who provided the service.Service/Procedure—The type of service you received.Total Cost—The amount we pay for the service. ... Not Covered—The amount of the service not covered (this usually only occurs if the service is denied).More items...•
Should you keep explanation of benefits?
When you or someone you are caring for is seriously ill, it is recommended that you keep EOBs for five years after the illness or condition is alleviated. If you or the patient is claiming or has claimed a medical deduction, keep the explanation of benefits for seven years.
What is a Medicare Summary Notice?
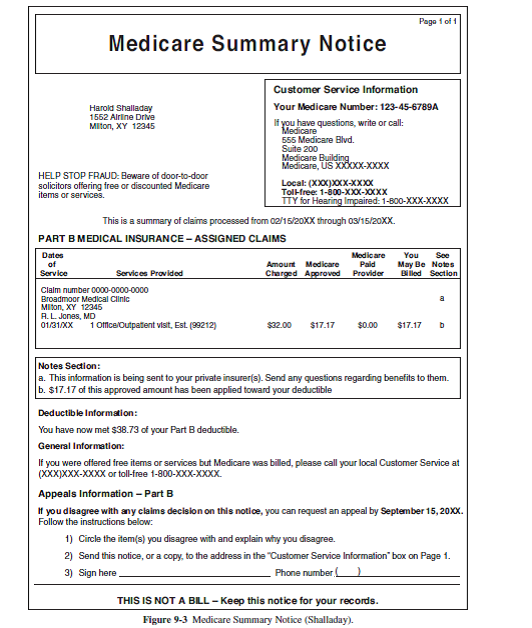
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period. What Medicare paid. The maximum amount you may owe the provider.
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
Can providers call Medicare?
CMS also relies on providers and suppliers to ask their Medicare patients about the presence of other primary health care coverage, and to report this information when filing claims with the Medicare program.
Do I need to keep Medicare summary notices?
How Long Should You Keep Medicare Summary Notices? Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance.
How do I get a Medicare Summary Notice?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
How long should Medicare EOBs be kept?
1. Keep medical EOBs in a file for one year. As the bills and EOBs for a medical service come in, match related items together, and address any discrepancies you detect. Examples might include double billing or your health insurance company overlooking the fact that you have met your deductible.
What is an Explanation of Benefits?
The first thing to know about an Explanation of Benefits is that it’s not a bill. Instead, it’s a summary of the claims and charges applied to your...
Who Receives an EOB?
Anyone enrolled in Medicare Advantage and Medicare Prescription Drug Plan (Part D) will receive an EOB when they use their policy. You don’t need t...
How Do I Read My EOB?
You can expect to see a few standard terms, no matter who sends your Explanation of Benefits. They are:
Can I Get Another Copy of my EOB?
If you misplaced your most recent EOB or didn’t receive it in the mail, contact your insurance company. A representative should be able to provide...
I’m on Original Medicare (Parts A and B) -- Do I get an EOB?
No, but you’ll receive a Medicare Summary Notice (MSN), the Medicare explanation of benefits. Like the EOB, the MSN is not a bill — it’s a monthly...
Does my EOB show specific prescription info?
If you have a Medicare Prescription Drug EOB, it can show which medicines you’re taking, how much they cost, and how much your insurance covers. [i]
Will I get an EOB each month if I don't see a doctor?
Your insurance company is only required to send you an EOB when you make a claim. This happens any time you see a healthcare provider through your...
What is EOB in Medicare?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. You only receive an EOB if you have Medicare Advantage or Part D. An EOB is not the same as a Medicare Summary Notice.
Is EOB the same as Medicare?
An EOB is not the same as a Medicare Summary Notice. It is also important to remember that an EOB is not a bill. EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
What does EOB mean for prescription drug?
When you receive an EOB from your prescription drug plan provider, they are providing you with a tool that shows you the value of your coverage with them. You can use it to keep an account of your annual deductible amount, to see whether you have reached it, or how much is left to go.
What to do if you find errors in Medicare?
If you find errors, or have questions, call your plan provider right away. If you believe that Medicare fraud is involved, call the Medicare Drug Integrity Contractor. The EOBs you receive provide monthly and annual summaries of your prescription drug plan costs.
Is EOB a bill?
Because of this type of information, the EOB may look like a bill, and many find this confusing. It is not a bill. Here is the information you should see on your EOB in more detail:
Does Medicare have an EOB?
An Explanation of Benefits (EOB) is not a bill ...
What is EOB in medical billing?
Your EOB is a window into your medical billing history. Review it carefully to make sure you actually received the service being billed, that the amount your doctor received and your share are correct, and that your diagnosis and procedure are correctly listed and coded.
What is EOB in healthcare?
Updated on July 19, 2020. An explanation of benefits (EOB) is a form or document provided to you by your insurance company after you had a healthcare service for which a claim was submitted to your insurance plan. Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) ...
Why Is Your Explanation of Benefits Important?
Healthcare providers’ offices, hospitals, and medical billing companies sometimes make billing errors . Such mistakes can have annoying and potentially serious, long-term financial consequences.
What does EOB mean for medical?
Your EOB will generally also indicate how much of your annual deductible and out-of-pocket maximum have been met. If you're receiving ongoing medical treatment, this can help you plan ahead and determine when you're likely to hit your out-of-pocket maximum. At that point, your health plan will pay for any covered in-network services you need for the remainder of the plan year.
What is EOB information?
Your EOB has a lot of useful information that may help you track your healthcare expenditures and serve as a reminder of the medical services you received during the past several years.
What is an EOB?
Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) was paid on your behalf—if applicable—and how much you're responsible for paying yourself.
What does "not covered" mean on an EOB?
Not Covered Amount: The amount of money that your insurance company did not pay your provider. Next to this amount you may see a code that gives the reason the healthcare provider was not paid a certain amount. A description of these codes is usually found at the bottom of the EOB, on the back of your EOB, or in a note attached to your EOB. Insurers generally negotiate payment rates with healthcare provider, so the amount that ends up being paid (including the portions paid by the insurer and the patient) is typically less than the amount the provider bills. The difference is indicated in some way on the EOB, with either an amount not covered, or a total covered amount that's lower than the billed charge.
What does EOB stand for in Medicare?
EOB stands for explanation of benefits. MSN stands for Medicare summary notice. Both of these documents help you understand how your Medicare benefits are being used and how much you may owe out-of-pocket.
What is an EOB code?
EOBs also usually have codes, known as reason codes. These codes help tell the provider why Medicare didn't pay for something so the provider's billing office can follow up. Usually, you don't need to worry that much about these codes. However, the codes may be explained on the bottom of the EOB if you're interested. You can also call your Medicare customer service line to ask about the codes or why certain claims weren't paid.
What to do if you suspect Medicare billing?
If you suspect that providers are billing Medicare for services that weren't provided to you, you can call your Medicare customer service line to report it. You can also talk to your provider if the patient responsibility on your Medicare EOB is less than what you were billed, as that might indicate a mistake in billing.
Why is it important to compare your MSN to your EOBs?
This helps you ensure all your claims are being billed accurately and what you're being asked to pay by providers is correct.
How often do you get a summary notice from Medicare?
You receive a Medicare Summary Notice every quarter that you receive Medicare-covered health care services. The notice summarizes how much Medicare paid for services during that period and how much you may owe out-of-pocket.
How often do beneficiaries get their MSN?
Beneficiaries will get their MSN every 3 months if they get any services or medical supplies during that 3-month period. If they didn’t get any services or medical supplies during that 3-month period, they won’t get an MSN for that particular 3-month period.
What is an appeal in Medicare?
An appeal is the action a client takes if they disagree with a coverage or payment decision made by Original Medicare, a Medicare Advantage plan or a Medicare prescription drug plan.