How Do I Drop Medicare Part B?
- Social Security and Signing Up for Medicare. If you’ve deferred your Social Security benefits until your full retirement...
- Send Your Medicare Card Back. If you’re still working past 65 and have health insurance through your employer, you can...
- Contact Social Security and Tell Them You Wish to Waive Medicare Part B. If you get Medicare...
How do I Opt Out of Medicare Part B?
To drop Part B (or Part A if you have to pay a premium for it), you usually need to send your request in writing and include your signature. Contact Social Security. If you recently got a welcome packet saying you automatically got Medicare Part A and Part B, follow the instructions in your welcome packet, and send your Medicare card back. If you keep the card, you agree to …
What happens if I cancel Medicare Part B?
Nov 24, 2021 · You can voluntarily terminate your Medicare Part B (medical insurance). However, since this is a serious decision, you may need to have a personal interview. A Social Security representative will help you complete Form CMS 1763 .
Can I Opt Out of Medicare Part B?
Jun 05, 2020 · How to cancel Medicare Part B The Part B cancellation process begins with downloading and printing Form CMS 1763, but don’t fill it out yet. You’ll need to complete the form during an interview with a representative of the Social Security Administration (SSA) by …
How to opt out of Medicare Part B?
Apr 13, 2022 · How Do I Drop Medicare Part B? Social Security and Signing Up for Medicare. If you’ve deferred your Social Security benefits until your full retirement... Send Your Medicare Card Back. If you’re still working past 65 and have health insurance through your employer, you can... Contact Social Security ...

What happens if I don't want Medicare Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
Can I drop Medicare Part B if I have other insurance?
You are not required to have Medicare Part B coverage if you have employer coverage. You can drop Medicare Part B coverage and re-enroll in it when you need it.Dec 18, 2021
How do I get rid of Part B premium?
To request a reduction of your Medicare premium, contact your local Social Security office to schedule an appointment or fill out form SSA-44 and submit it to the office by mail or in person.Mar 30, 2022
Can I pause my Medicare Part B?
You can disenroll from Part B and stop paying premiums for it in this situation, regardless of whether it was you or your spouse who landed this new job. In other words, you're allowed to delay Part B without penalty if you have health insurance from current employment and the employer plan is primary to Medicare.Dec 22, 2021
How do I opt out of Medicare Part A?
If you want to disenroll from Medicare Part A, you can fill out CMS form 1763 and mail it to your local Social Security Administration Office. Remember, disenrolling from Part A would require you to pay back all the money you may have received from Social Security, as well as any Medicare benefits paid.Oct 27, 2014
Can you drop Medicare Part B if you go back to work?
If you're going back to work and can get employer health coverage that is considered acceptable as primary coverage, you are allowed to drop Medicare and re-enroll again without penalties. If you drop Medicare and don't have creditable employer coverage, you'll face penalties when getting Medicare back.
Are Medicare Part B premiums going up in 2021?
In November 2021, CMS announced the monthly Medicare Part B premium would rise from $148.50 in 2021 to $170.10 in 2022, a 14.5% ($21.60) increase.Jan 12, 2022
Why is my Medicare Part B premium so high?
According to CMS.gov, “The increase in the Part B premiums and deductible is largely due to rising spending on physician-administered drugs. These higher costs have a ripple effect and result in higher Part B premiums and deductible.”
Is there a cap on Medicare Part B penalty?
Is There a Cap on the Medicare Part B Penalty? As of now, there is no cap on the Part B late enrollment penalty. However, if passed, the Medicare Part B Fairness Act or H.R. 1788 would cap the penalty amount at 15% of the current premium, regardless of how many 12-month periods the beneficiary goes without coverage.
Where do I send my CMS Form 1763?
You must submit this form to the Social Security Administration or you may contact them at 1-800-772-1213 for assistance.
How do I fill out CMS 1763?
How to Complete Form CMS 1763?Write down the name of the enrollee. ... State your Medicare number;Choose the type of coverage you want to terminate. ... Indicate the date when your hospital or medical insurance coverage should end;State the reasons for the termination. ... Make sure the request is complete and sign the form.More items...
What to do if you drop Part B?
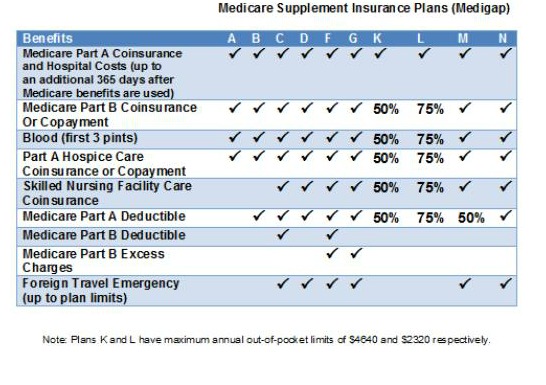
If you’re dropping Part B because you can’t afford the premiums, remember that you could save money on your health care costs in other ways. Consider adding a Medicare Advantage or Medigap plan instead of dropping Part B. Call us to learn more about these alternatives to disenrolling in Part B.
What happens if you opt out of Part B?
But beware: if you opt out of Part B without having creditable coverage—that is, employer-sponsored health insurance from your current job that’s as good or better than Medicare—you could face late-enrollment penalties (LEPs) down the line.
What happens if you don't have health insurance?
Without health insurance that’s as good or better than Medicare, you could start racking up late-enrollment penalties the longer you go without coverage. If you decide to re-enroll in Part B later, these penalties could make your premiums (what you pay for coverage) even less affordable.
How to schedule an interview with Social Security?
Call a Licensed Agent: 833-271-5571. You can schedule an in-person or over-the-phone interview by contacting the SSA. If you prefer an in-person interview, use the Social Security Office Locator to find your nearest location. During your interview, fill out Form CMS 1763 as directed by the representative.
Is it easy to cancel Medicare Part B?
Disenrolling in Medicare Part B isn’t an easy process because it requires an in-person or phone interview. But this is intentional. Canceling Part B could have negative consequences for your wallet (in the form of late-enrollment penalties) and your health (in the form of a gap in coverage).
Can Medicare tack late enrollment penalties?
If you have a gap in coverage, the Medicare program could tack late-enroll ment penalties onto your Part B premiums if you re-enroll in coverage again later. Avoid this pitfall by working with your human resources department to ensure that your company's insurance is indeed creditable (meaning that it’s as good or better than Medicare Part B). You may need to provide documentation of creditable coverage during your Part B cancellation interview.
Does Medicare Advantage offer rebates?
Consider a Medicare Advantage plan that offers a rebate on your Part B premium. Here's how that works: A Medicare Advantage plan provides the same or better coverage than Part A (hospital insurance) and Part B (medical insurance). To receive this coverage, most enrollees pay a premium for their Medicare Advantage plan in addition to the cost ...
How to cancel Medicare Part B?
To cancel your Medicare Part B coverage, download and print the online form . However, you won’t be required to fill the form yet. Before you fill the form, you will go through an interview process with a representative of the Social Security Administration in person or through the phone. You can either choose to have the interview in person ...
What to do if you are enrolled in Medicare but your coverage has not started?
If you were enrolled automatically for Medicare but the coverage has not started. Check your Medicare card and follow the instructions that came with the card to return the card and cancel your coverage.
What happens if you don't sign up for Part B?
Also, be aware that if you don’t sign up for Part B during your eight-month window, the late penalty will date from the end of your employer coverage (not from the end of the special enrollment period), said Patricia Barry, author of “Medicare for Dummies.”.
How much Medicare will be available in 2026?
For those ages 75 and older, 10.8% are expected to be at jobs in 2026, up from 8.4% in 2016 and 4.6% in 1996. The basic rules for Medicare are that unless you have qualifying insurance elsewhere, you must sign up at age 65 or face late-enrollment penalties. You get a seven-month window to enroll that starts three months before your 65th birthday ...
What happens if you don't follow Medicare guidelines?
And if you don’t follow those guidelines, you might end up paying a price for it. “You could be accruing late-enrollment penalties that last your lifetime,” said Elizabeth Gavino, founder of Lewin & Gavino in New York and an independent broker and general agent for Medicare plans.
How long does it take to enroll in Medicare if you stop working?
First, once you stop working, you get an eight-month window to enroll or re-enroll. You could face a late-enrollment penalty if you miss it. For each full year that you should have been enrolled but were not, you’ll pay 10% of the monthly Part B base premium.
Why do people sign up for Medicare at 65?
While most people sign up for Medicare at age 65 because they either no longer are working or don’t otherwise have qualifying health insurance, the ranks of the over-65 crowd in the workforce have been steadily growing for years. And in some cases, that means employer-based health insurance is an alternative ...
How long do you have to have Part D coverage?
You also must have Part D coverage — whether as a standalone plan or through an Advantage Plan — within two months of your workplace coverage ending, unless you delayed signing up for both Part A and B. If you miss that window, you could face a penalty when you do sign up.
Do you have to drop a Medicare supplement?
Additionally, if you have a Medicare supplement policy — i.e., “ Medigap ” — you’d have to drop that, as well. And those policies have their own rules for enrolling, which means you might face medical underwriting if you reapply down the road.
How to disenroll from Part B?
If you do not initially disenroll in Part B, you will have to do so by contacting your local Social Security office or calling 1-800-772-1213 (TTY 1-800-325-0778). You may not disenroll from Part B online. You will have to speak directly to a Social Security agent to complete the process.
How to cancel Medicare Part A?
But if you do pay a premium for Part A and wish to cancel it, you may do so by visiting your local Social Security office or by calling 1-800-772-1213 (TTY 1-800-325-0778).
When does Medicare Part C end?
If you wish to cancel your Medicare Part C (Medicare Advantage) plan, here is one option for cancelling your coverage: The Fall Annual Enrollment Period (AEP, sometimes called the Open Enrollment Period for Medicare Advantage and Medicare prescription drug coverage) lasts from October 15 to December 7 each year.
When is Medicare open enrollment?
Starting in 2019, you can take advantage of the Medicare Advantage Open Enrollment Period, which runs each year from January 1 through March 31. During this time, you can change from one Medicare Advantage plan to another, whether or not either plan includes prescription drug coverage. You can also disenroll from your Medicare Advantage plan ...
What is Medicare Part B?
Some people automatically get. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , and some people need to sign up for Part B. Learn how and when you can sign up for Part B. If you don't sign up for Part B when you're first eligible, ...
What happens if you don't get Part B?
Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board. Office of Personnel Management. If you don’t get these benefit payments, you’ll get a bill. Most people will pay the standard premium amount.
What is the standard Part B premium for 2021?
The standard Part B premium amount in 2021 is $148.50. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
How much do you pay for Medicare after you meet your deductible?
After you meet your deductible for the year, you typically pay 20% of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How much is Part B deductible in 2021?
Part B deductible & coinsurance. In 2021, you pay $203 for your Part B. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. . After you meet your deductible for the year, you typically pay 20% of the.
Do you pay Medicare premiums if your income is above a certain amount?
If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.
When do you get Medicare Part B?
Generally, people are first eligible for Medicare Part B when they turn 65 years old, unless they have other qualifying conditions. Part B covers medically necessary services and supplies, such as: outpatient care and emergency room visits. preventive services including tests and screenings. ambulance transport.
Who is eligible for Medicare Part A and Part B?
Medicare extends both Medicare Part A and Part B benefits to people who are: aged 65 or older. disabled and receiving Social Security Income (SSI) or Railroad Retirement Board (RRB) benefits.
What happens if you don't pay Medicare?
If a person does not pay following the 3-month grace period, they will get a termination notice stating they no longer have Medicare coverage. However, if a person pays their missed premiums within 30 days of the termination notice, they will continue to receive Part B coverage.
How much is Medicare premium 2021?
For individuals with an income below $88,000, the standard premium is $148.50 in 2021, with an annual deductible of $203. According to the Centers for Medicare and Medicaid Services, about 7% of Medicare Part B beneficiaries will pay a higher income adjusted premium.
What is a good cause policy for Medicare?
Medicare good cause policy. If a person feels they have a good reason or cause for not paying their premiums, they can ask Medicare for reinstatement under the Medicare good cause policy. The individual must be able to prove the reason for missing payments.
What are the benefits of Medicare?
Medicare extends both Medicare Part A and Part B benefits to people who are: 1 aged 65 or older 2 disabled and receiving Social Security Income (SSI) or Railroad Retirement Board (RRB) benefits 3 diagnosed with end stage renal disease (ESRD) 4 diagnosed with amyotrophic lateral sclerosis (ALS)
When is the Medicare enrollment period?
Medicare General Enrollment Period. January 1 to March 31 is the Medicare general enrollment period (GEP). People can join or reenroll in Medicare parts A and B for coverage to begin on July 1. People with an advantage plan can also switch between plans or join original Medicare.
What happens if you cancel Medicare Part B?
If you’ve disenrolled from or cancelled your Medicare Part B coverage, you may have to pay a costly late enrollment penalty to reenroll. This is especially true if you have a gap in coverage. If you’re looking to reenroll in Medicare Part B, follow these steps: Go to the Social Security Administration website. Complete the application.
How long do you have to pay back Medicare Part B?
If you were disenrolled from your Medicare part B plan for missing premium payments, you have 30 days from the official termination date to repay what’s due. If accepted, your coverage will continue. If you don’t pay back the premiums within the allotted time, you’ll have to reenroll during the next general enrollment period, ...
How long does it take to reenroll in Medicare?
Special enrollment period — 8 months following a qualifying event. If you qualify, you may be granted this 8-month window to reenroll in original Medicare or change your Medicare coverage after a significant life event, such as a divorce or move. Read on to learn more about how to reenroll in Medicare Part B and what it covers.
How long does it take to get Part B?
If you’re already covered through a workplace plan, or if you or your spouse suffer from a disability, you can sign up for Part B at any time. An 8-month special enrollment period to enroll into Part B insurance also comes into play 1 month after your employment or workplace insurance plan ends.
When is Medicare open enrollment?
Medicare open enrollment period — October 15 through December 7. During this time, you can switch from a Medicare Advantage (Part C) plan back to original Medicare. You can also change Part C plans or add, remove, or change a Medicare Part D (prescription drug) plan. Special enrollment period — 8 months following a qualifying event.
How long does it take to enroll in a new health insurance plan?
The initial enrollment period is a 7-month time frame. It includes: the 3 months before the month you turn 65 years old. your birth month. 3 months after your birth month. It’s recommended that you enroll during the first 3 months of initial enrollment so your coverage will begin earlier and you’ll avoid delays.