File an application to enroll by contacting the Social Security Administration; Enroll during a valid enrollment period; and Also enroll in or already have Part B. To keep premium Part A, the person must continue to pay all monthly premiums and stay enrolled in Part B.
How do I apply for Medicare Part B during a special enrollment?
Go to “ Apply Online for Medicare Part B During a Special Enrollment Period ” and complete CMS-40B and CMS-L564. Then upload your evidence of Group Health Plan or Large Group Health Plan. Fax or mail your CMS-40B, CMS-L564, and secondary evidence to your local Social Security office (see list of secondary evidence below).
Who is eligible for Medicare special enrollment period?
Disabled TRICARE beneficiaries TRICARE beneficiaries who are under 65 and qualify for Medicare because of a disability, ALS (Lou Gehrig’s Disease) or End-Stage Renal Disease (ESRD) may be eligible for a Special Enrollment Period if they didn’t sign up for Medicare Part B when they first became eligible. When does a Special Enrollment Period start?
When do I sign up for Medicare Part A or Part B?
Beginning the month that follows the end of your employer coverage (whether you retired or your coverage was terminated), you will be given a Special Enrollment Period of eight months to sign up for Part A and/or Part B. One thing to note: Medicare does not consider COBRA coverage or retiree health plans to be active employer coverage.
Who is eligible to enroll in Part B?
Individuals who are eligible for premium-free Part A are also eligible for enroll in Part B once they are entitled to Part A. Enrollment in Part B can only happen at certain times. Individuals who must pay a premium for Part A must meet the following requirements to enroll in Part B: Be age 65 or older;
Are you automatically enrolled in Medicare Part A and B?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
How do I add Medicare Part A?
Apply online (at Social Security) – This is the easiest and fastest way to sign up and get any financial help you may need. You'll need to create your secure my Social Security account to sign up for Medicare or apply for Social Security benefits online. Call 1-800-772-1213. TTY users can call 1-800-325-0778.
What is a special enrollment period for Medicare Part B?
What is the Medicare Part B special enrollment period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse's current job. You usually have 8 months from when employment ends to enroll in Part B.
Can Medicare Part B be added at any time?
Special Enrollment Period If you are eligible for the Part B SEP, you can enroll in Medicare without penalty at any time while you have job-based insurance and for eight months after you lose your job-based insurance or you (or your spouse) stop working, whichever comes first.
Do you have to enroll in Medicare Part B every year?
Do You Need to Renew Medicare Part B every year? As long as you pay the Medicare Part B medical insurance premiums, you'll continue to have the coverage. The premium is subtracted monthly from most people's Social Security payments. If you don't get Social Security, you'll get a bill.
How much is Medicare Part A?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
What is a Medicare special enrollment?
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What does special enrollment period mean?
A time outside the yearly Open Enrollment Period when you can sign up for health insurance. You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
Can I submit form CMS-L564 online?
You can complete form CMS-40B (Application for Enrollment in Medicare – Part B [Medical Insurance]) and CMS-L564 (Request for Employment Information) online. You can also fax the CMS-40B and CMS-L564 to 1-833-914-2016; or return forms by mail to your local Social Security office.
Can I delay Medicare Part A?
However, if you have to pay a premium for Part A, you can delay Part A until you (or your spouse) stop working or lose that employer coverage. You will NOT pay a penalty for delaying Part A, as long as you enroll within 8 months of losing your coverage or stopping work (whichever happens first).
What is the Part B late enrollment penalty?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
Can I delay Medicare Part B if I am still working?
If you qualify and decide you want to delay enrolling in Medicare Part B, you should not face any late enrollment penalties for Part B. When you lose your employer coverage, you will get an 8-month Special Enrollment Period during which to enroll in Medicare Part B, and Part A if you haven't done so already.
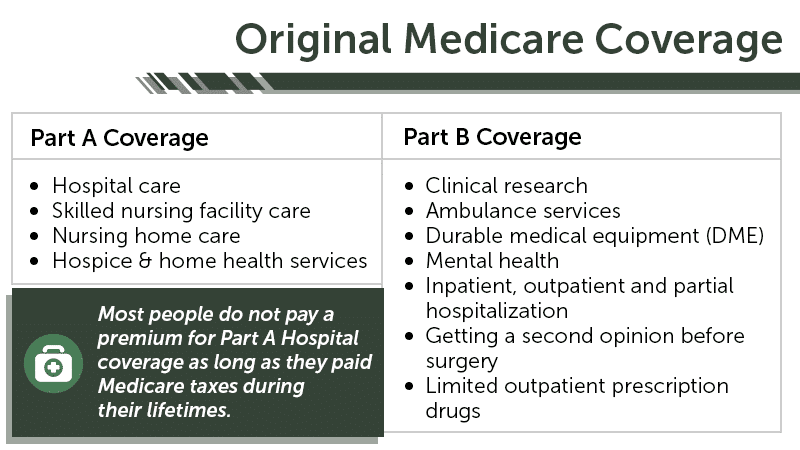
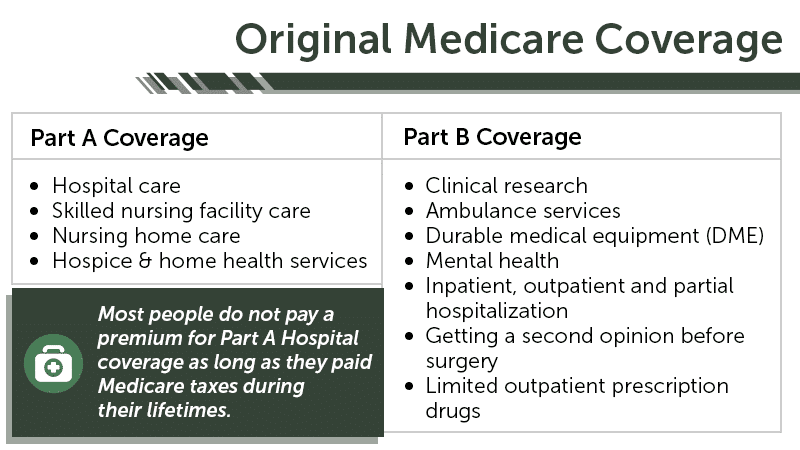
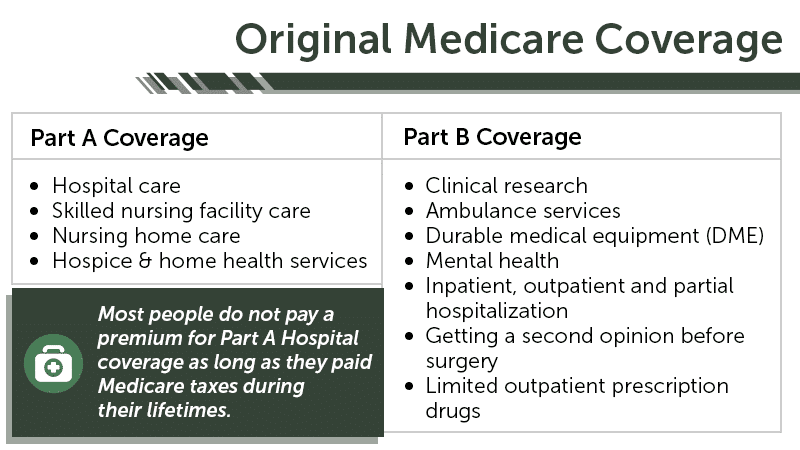
What does Part B cover?
Part B helps cover medically necessary services like doctors’ services, outpatient care, and other medical services that Part A doesn’t cover. Part B also covers many preventive services. Part B coverage is your choice. However, you need to have Part B if you want to buy Part A.
What is Part A insurance?
Part A helps cover your inpatient care in hospitals. Part A also includes coverage in critical access hospitals and skilled nursing facilities (not custodial or long-term care). It also covers hospice care and home health care. You must meet certain conditions to get these benefits.
Does Medicare cover prescription drugs?
Medicare prescription drug coverage is available to everyone with Medicare. Private companies provide this coverage. You choose the Medicare drug plan and pay a monthly premium. Each plan can vary in cost and specific drugs covered. If you decide not to join a Medicare drug plan when you’re first eligible, and you don’t have other creditable prescription drug coverage, or you don’t get Extra Help, you’ll likely pay a late enrollment penalty. You may have to pay this penalty for as long as you have Medicare drug coverage.
Can I get medicare if I have SSI?
Getting SSI doesn’t make you eligible for Medicare. SSI provides a monthly cash benefit and health coverage under Medicaid. Your spouse may qualify for Medicare when he/she turns 65 or has received disability benefits for 24 months.
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
How long do you have to disenroll from Medicare Advantage?
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How long does Medicare Advantage coverage last?
If you had a Medicare Advantage plan with prescription drug coverage which met Medicare’s standards of “creditable” coverage and you were to lose that coverage through no fault of your own, you may enroll in a new Medicare Advantage plan with creditable drug coverage beginning the month you received notice of your coverage change and lasting for two months after the loss of coverage (or two months after receiving the notice, whichever is later).
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
What to do if you don't fit into Medicare?
If your circumstances do not fit into any of the Special Enrollment Periods described above, you may ask the Centers for Medicare and Medicaid Services (CMS) for your own Special Enrollment Period based on your situation.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
When will I be enrolled in Medicare?
If you are younger than age 65 and receive disability benefits under Social Security Disability Insurance (SSDI) or Railroad Retirement, you will automatically be enrolled in Medicare Parts A and B in the 25th month of your disability payments , or sooner if you have either end-stage renal disease ...
What is a SEP for Part B?
When your employer coverage or employment ends (whichever is earlier), you will have a Special Enrollment Period (SEP) for Part B and a Special Election Period for Part D, and will not be penalized for late enrollment if you sign up for: Note: If you have ESRD, you do not have the same SEP for Part B.
How much is the late enrollment penalty for Part B?
You may also be required to pay a late enrollment penalty of 10% of the current Part B premium for each 12-month period you could have had Part B coverage, but did not take it. For beneficiaries age 65 and older, this penalty is for life, and you will always pay more for your Part B coverage than other people.
When does Part B coverage end?
If you turn down Part B and don’t have other coverage due to active employment, but later decide you want Part B coverage, you can only enroll during the annual General Enrollment Period (GEP), which is January 1 through March 31. Your Part B benefits will not be effective until July 1 of that year.
When do you get Medicare if you are 65?
1. If You Are Approaching or at Age 65. If you are approaching age 65 and you already receive Social Security or Railroad Retirement benefits through early retirement, you will be automatically enrolled in Medicare Parts A (hospital insurance) and B (medical insurance) when you turn 65. Approximately 3 months prior to your 65th birthday, ...
Who is a dependent child on Social Security?
You are the spouse or dependent child of a person who has worked the required amount of time under Social Security, the Railroad Retirement Board or as a Medicare-qualified government employee, or who is receiving Social Security, Railroad Retirement or federal retirement benefits.
Can I get Medicare if I don't have SSDI?
You can also get Medicare if you are not receiving SSDI benefits if you meet one of the following conditions: You have worked long enough under Social Security (40 quarters), the Railroad Retirement Board or as a Medicare-qualified government employee.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
What to do if your Social Security enrollment is denied?
If your enrollment request is denied, you’ll have the chance to appeal.
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
When does Medicare Part B start?
If you don’t enroll in Medicare Part B during your initial enrollment period, you have another chance each year to sign up during a “general enrollment period” from January 1 through March 31. Your coverage begins on July 1 of the year you enroll. Read our Medicare publication for more information.
When do you have to apply for Medicare Part B?
Special Enrollment Period (SEP) If you have medical insurance coverage under a group health plan based on your or your spouse's current employment, you may not need to apply for Medicare Part B at age 65 . You may qualify for a " Special Enrollment Period " (SEP) that will let you sign up for Part B during: Any month you remain covered ...
What happens if you don't receive your Medicare card?
If you did not receive your red, white, and blue Medicare card, there may be something that needs to be corrected, like your mailing address.
What is Medicare Advantage Plan?
Medicare Advantage Plan (previously known as Part C) includes all benefits and services covered under Part A and Part B — prescription drugs and additional benefits such as vision, hearing, and dental — bundled together in one plan. Medicare Part D (Medicare prescription drug coverage) helps cover the cost of prescription drugs.
What is Medicare Part A?
Medicare Part A (hospital insurance) helps pay for inpatient care in a hospital or limited time at a skilled nursing facility (following a hospital stay). Part A also pays for some home health care and hospice care. Medicare Part B (medical insurance) helps pay for services from doctors and other health care providers, outpatient care, ...
How long does a spouse have to be covered by a group health plan?
Any month you remain covered under the group health plan and you or your spouse's employment continues. The 8-month period that begins with the month after your group health plan coverage or the employment it is based on ends, whichever comes first.
Who manages Medicare?
The Centers for Medicare & Medicaid Services (CMS) manages Medicare. After you are enrolled, they will send you a Welcome to Medicare packet in the mail with your Medicare card. You will also receive the Medicare & You handbook, with important information about your Medicare coverage choices.