Fill out CMS 855S, also known as the Medicare Enrollment Application for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Suppliers, if you sell medical equipment or supplies. Prepare to Submit Electronic Data Medicare payments and claims are all processed electronically.
Are orthotics covered by Medicare?
Your healthcare and the orthotic supplier must participate in the Medicare program for your orthotics to be covered. You will have to pay 20% of the cost of the orthotics after you’ve met your annual Medicare Part B deductible.
How do I enroll my provider in the Medicare program?
MDPP suppliers must use Form CMS-20134 to enroll in the Medicare Program. If you don’t see your provider type listed, contact your MAC’s provider enrollment center before submitting a Medicare enrollment application.
How do I become a Medicare participating provider or supplier?
To participate as a Medicare Program provider or supplier, submit the Medicare Participating Physician or Supplier Agreement (Form CMS-460) upon initial enrollment. You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
Do you want to order and certify for Medicare?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify. You wish to provide services to beneficiaries but do not want to bill Medicare for your services.

Which of the following are steps to becoming a Medicare provider?
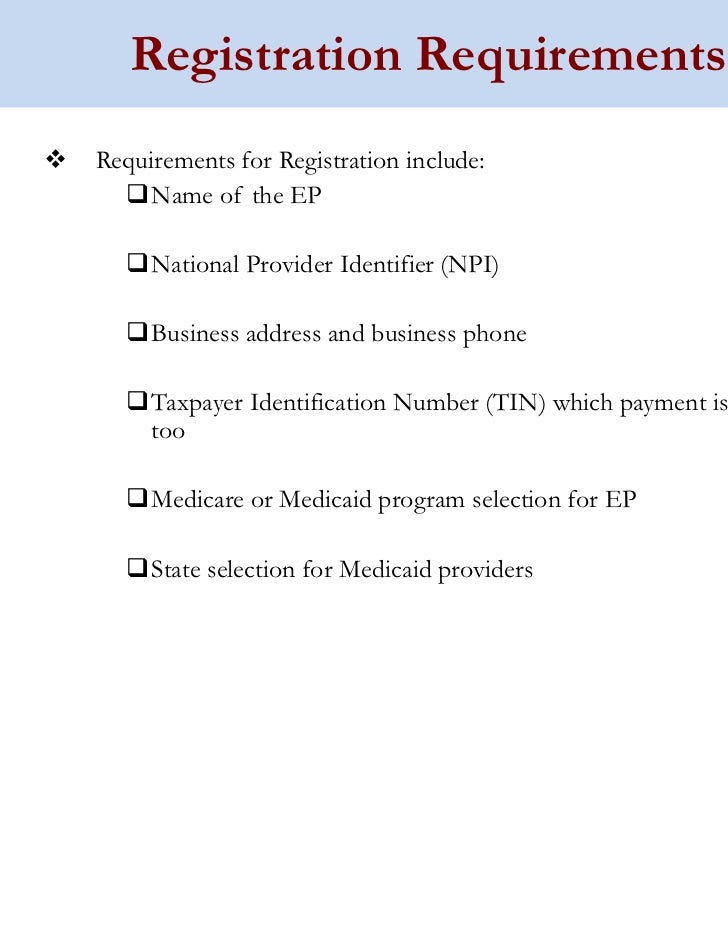
Applying to become a Medicare providerStep 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ... Step 2: Complete the Medicare Enrollment Application. ... Step 3: Select a Specialty Designation.
How do you get a Medicare product approved?
How to buy equipmentGo to an in-person doctor visit, where your doctor will write an order for the DME.Take the order to a Medicare-approved DME supplier.Depending on the product, ask the supplier if they will deliver it to your home.Find out if Medicare requires prior authorization for your DME.
How do I register as a Pecos provider?
0:146:13Medicare Provider Enrollment Through PECOS - YouTubeYouTubeStart of suggested clipEnd of suggested clipNumber if you do not already have an active NPI number you can register for one through the nationalMoreNumber if you do not already have an active NPI number you can register for one through the national plan and provider enumeration system or n Pez.
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
How long does it take to get a Medicare provider number?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.
What is DME accreditation?
Medical suppliers who wish to distribute durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) must apply for and receive accreditation that verifies the supplier meets the quality standards set forth by the Centers for Medicare & Medicaid Services.
What is Pecos Medicare requirement?
It is a database where physicians register with the Centers for Medicare and Medicare Services (CMS). CMS developed PECOS as a result of the Patient Protection and Affordable Care Act. The regulation requires all physicians who order or refer home healthcare services or supplies to be enrolled in Medicare.
How do I become a Pecos resident?
How to Complete Enrollment. Complete your enrollment online at https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/index. Select “Internet-based PECOS” located in the left navigation menu to access instructions and a link to the online enrollment form.
What is a Pecos provider?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.
What is the process of credentialing?
Credentialing is a formal process that utilizes an established series of guidelines to ensure that patients receive the highest level of care from healthcare professionals who have undergone the most stringent scrutiny regarding their ability to practice medicine.
Who performs the credentialing?
Many health care institutions and provider networks conduct their own credentialing, generally through a credentialing specialist or electronic service, with review by a credentialing committee. It may include granting and reviewing specific clinical privileges, and allied health staff membership.
What is Caqh and credentialing?
CAQH is an online data repository of credentialing data. Practitioners self report demographic, education and training, work history, malpractice history, and other relevant credentialing information for insurance companies to access.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What are the two types of NPIs?
There are 2 types of NPIs: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs for solely ordering items or certifying services. Apply for an NPI in 1 of 3 ways:
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
What is NPI in DMEPOS?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. DMEPOS suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
What is the Medicare enrollment form for DMEPOS?
DMEPOS suppliers must enroll in the Medicare program using the Medicare enrollment application (Form CMS-855S) in order to be eligible to receive Medicare payment for covered services provided to Medicarebeneficiaries.
Why do people use orthotics?
For people experiencing orthopedic problems like foot pain, osteoarthritis, spinal injury, back pain, or other orthopedic conditions, orthotic devices may provide support and pain relief. Many physicians prescribe orthotics to aid the healing process after surgeries like hip or knee replacement, or injuries like whiplash.
What are the orthotics for DME?
Medicare lists the following devices as orthotics under the heading of DME: Bracing for ankle, foot, knee, back, neck, spine, hand, wrist, elbow. Orthopedic shoes as a necessary part of a leg brace. Prosthetic devices like artificial limbs. Medicare recipients must meet all the following prerequisites for eligibility:
What is the Medicare Part B deductible?
In 2019, the yearly Part B deductible is $185.00.
What is the purpose of orthotics?
Orthotics can help support the entire leg and foot for proper alignment, and to avoid foot pronation. In the case of a slight difference in leg length that causes a loss of balance or awkwardness while walking, a custom foot orthotic may correct this. Spinal orthotic devices include back and neck braces. They stabilize and support areas of the body ...
What is the life expectancy of an orthotic?
Medicare considers durable medical equipment to be equipment used for medical reasons in the home, to have a life expectancy of more than 3 years, and not to be useful to anyone not sick or injured.
Does Medicare cover orthotics?
Medicare Coverage for Orthotic Devices. Medicare Part B pays for 80 percent of the approved cost of either custom-made or pre-made orthotic devices. Of course, this is only possible if your health care provider feels it is medically necessary.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Can a doctor be enrolled in Medicare?
Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers if they participate in Medicare before you get these items.
Does Medicare cover prescriptions?
applies. Medicare will only cover these items if your doctors and suppliers are enrolled in Medicare.
How to Get Your NPI
To begin, you must receive a one-of-a-kind National Provider Identifier, or NPI. This 10-digit NPI number is necessary in all administrative and billing activities to identify the provider anonymously without looking at other information, such as their medical specialty. The numbering system was created in accordance with HIPAA standards.
Determine Your Eligibility to Serve as a Medicare Provider
The next stage is to determine your eligibility as a Medicare provider. You may need to be certified with the Conditions of Participation in order to be eligible. Most providers’ eligibility is determined by state bodies, not by the Centers for Medicare and Medicaid Services.
Fill out the Enrollment Application
The next step toward becoming a provider is to fill out an enrollment application. CMS 855A, commonly known as the Medicare Enrollment Application for Institutional Providers, is required for institutional providers such as home health organisations, hospices, and outpatient physical therapy programmes.
Prepare to Submit Electronic Data
Medicare payments and claims are all processed electronically. To submit claims, you must complete the CMS EDI Registration Form and the EDI Enrollment Form. Enroll in Electronic Funds Transfer to get the amounts owed to you by Medicare. The forms are available online at the CMS website or through your Medicare FFS Contractor.
Pursue Annual Renewal
When you are approved to become a Medicare provider, you are automatically enrolled in Medicare Part A unless you opt-out. According to the American Medical Association, you must choose whether to participate in Medicare Part B or Part D on an annual basis.
Employ Your MAC
Your Medicare Administrative Contractor (MAC) is specific to the region in where you practice and may have extra information demands when processing your application. You can also inquire with your MAC about your enrollment status.
Keep Your Information Up to Date
It is critical to keep your enrollment information current. If you want to keep your Medicare billing credentials, you must disclose the following changes within 30 days:
