On the top menu bar, click Settings > Codes > Find Procedures. The Find Procedure window opens. Enter all or part of a keyword of the procedure in the Look For search box.
Full Answer
How do you enter a procedure code on a bill?
PROCEDURE CODES AND DATES Enter the full ICD-9-CM, including all four-digit codes where applicable for the principal procedure (first code). Enter the date in MMDDYY format that the procedure was performed during the billing period (within the ‘from’ and ‘through’ dates of services in form locator 6).
How do I process HCPCS codes for medical services?
FISS performs pre-payment processing of HCPCS codes for laboratory services; but radiology, ambulatory surgery center (ASC), durable medical equipment (DME), and medical diagnostics HCPC service codes are processed post-payment. To start the inquiry process, enter the HCPCS code and the locality code, then press [ENTER].
What is the multiple Procedure Rule for Medicare?
Under the so-called “multiple procedure rule,” Medicare pays less for the second and subsequent procedures performed during the same patient encounter. There are several ways in which reductions may be taken, as indicated for each CPT® code in column “S” of the Physician Fee Schedule Relative Value file.
How do I enter the ICD-9-CM code for a procedure?
Enter the date in MMDDYY format that the procedure was performed during the billing period (within the ‘from’ and ‘through’ dates of services in form locator 6). PRV ESRD HOURS This field identifies the ICD-9-CM or ICD-10-CM code describing the patient’s stated reason for seeking care at the time of outpatient registration.
What is a procedure code in Medicare?
Providers that bill Medicare use codes for patient diagnoses and codes for care, equipment, and medications provided. “Procedure” code is a catch-all term for codes used to identify what was done to or given to a patient (surgeries, durable medical equipment, medications, etc.).
What does KX modifier mean for Medicare?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
What CPT codes are not accepted by Medicare?
Certain services are never considered for payment by Medicare. These include preventive examinations represented by CPT codes 99381-99397. Medicare only covers three immunizations (influenza, pneumonia, and hepatitis B) as prophylactic physician services.
How do I bill add on CPT codes?
In the CPT Manual an add-on code is designated by the symbol "+". The code descriptor of an add-on code generally includes phrases such as "each additional" or "(List separately in addition to primary procedure)."
How do you use the KX modifier?
Apply the KX modifier when you provide medically necessary services above the soft cap. Therapists should continue to affix the KX modifier to all medically necessary services above the designated limit ($2,010 in 2018), thus signaling Medicare to pay the claim.
When can you use a KX modifier?
The KX modifier should only be used when the therapist (not the biller or the billing company) has made a determination that skilled therapy is medically necessary over the $1920 therapy caps.
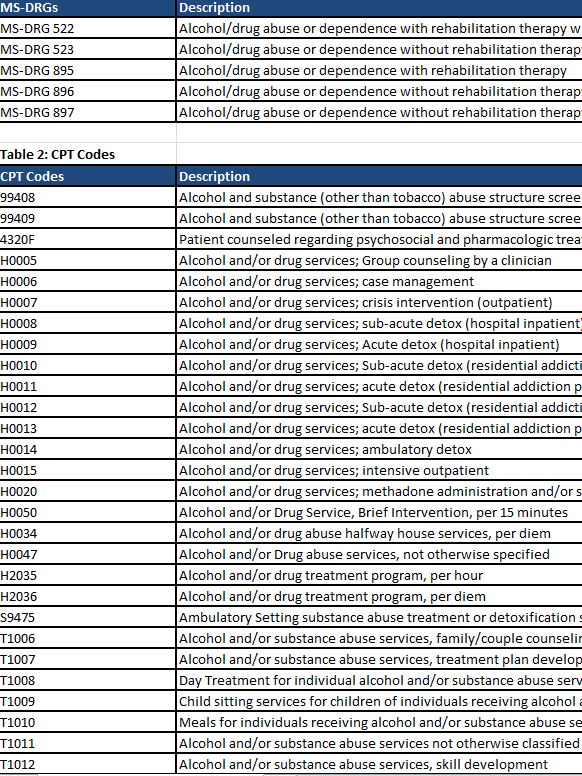
Does Medicare accept CPT codes?
When a health care provider bills Medicare to seek reimbursement, they will use CPT codes to list the various treatments they delivered. The CPT codes used to bill for medical services and items are part of a larger coding system called the Healthcare Common Procedure Coding System (HCPCS).
Is my procedure covered by Medicare?
Generally, Medicare covers services (like lab tests, surgeries, and doctor visits) and supplies (like wheelchairs and walkers) that Medicare considers “medically necessary” to treat a disease or condition.
Does Medicare cover CPT code?
The Level II HCPCS codes, which are established by CMS's Alpha-Numeric Editorial Panel, primarily represent items and supplies and non-physician services not covered by the American Medical Association's Current Procedural Terminology-4 (CPT-4) codes; Medicare, Medicaid, and private health insurers use HCPCS procedure ...
Do you use modifier 59 with an add on code?
Yes you may append modifier 59 to an add on code.
What is the modifier for add on codes?
modifier 51 exemptThese codes can't be billed without a primary code, and the fee is already discounted as it is a secondary procedure. This is why add-on codes are “modifier 51 exempt” and, most of the time, you won't need to use any modifiers with CPT add-on codes.
Do add on codes need modifier 25?
No modifier is required in order for these codes to be separately reimbursed. New patient CPT codes require CPT modifier 25 when a separately identifiable E/M service is performed the same day as chemotherapy or nonchemotherapy infusions or injections as these are not considered surgery.
What is a type 1 add-on code?
A Type I add-on code, with one exception, is eligible for payment if one of the listed primary procedure codes is also eligible for payment to the same practitioner for the same patient on the same date of service.
What is an AOC code?
An AOC is a HCPCS/CPT code that describes a service that, with rare exception, is performed in conjunction with another primary service by the same practitioner. An AOC is rarely eligible for payment if it is the only procedure reported by a practitioner. Add-on codes may be identified in three ways:
Does CMS have effective dates?
CMS has added effective dates and deletion dates, where appropriate, for each of the Medicare Add-on Code Edits to aid in determining the active period of an add-on code edit for Medicare Services.
Why are CPT codes not included in CPT codes?
They are used to identify various items and services that are not included in the CPT code set because they are medical items or services that are regularly billed by suppliers other than physicians. For example, ambulance services, hearing and vision services, drugs, and durable medical equipment.
What are some examples of Medicare coverage documents?
Examples include guidance documents, compendia, and solicitations of public comments. Close.
What is MEDCAC in medical?
The MEDCAC reviews and evaluates medical literature, reviews technology assessments, public testimony and examines data and information on the benefits, harms, and appropriateness of medical items and services that are covered under Medicare or that may be eligible for coverage under Medicare.
What is a local coverage determination?
A Local Coverage Determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific jurisdiction that the MAC oversees. MACs are Medicare contractors that develop LCDs and process Medicare claims.
What is a LCD in Medicare?
LCDs are specific to an item or service (procedure) and they define the specific diagnosis (illness or injury) for which the item or service is covered. LCDs outline how the contractor will review claims to ensure that the services provided meet Medicare coverage requirements.
What percentage of Medicare beneficiaries are excluded from coverage?
For purpose of this exclusion, "the term 'usually' means more than 50 percent of the time for all Medicare beneficiaries who use the drug. Therefore, if a drug is self-administered by more than 50 percent of Medicare beneficiaries, the drug is excluded from coverage" and the MAC will make no payment for the drug.
Can an NCD exclude or limit an indication or circumstance?
If an NCD does not specifically exclude/limit an indication or circumstance, or if the item or service is not mentioned at all in an NCD or in a Medicare manual, an item or service may be covered at the discretion of the MAC based on a Local Coverage Determination (LCD).
What is the overlap between surgical and pre-procedure?
Most medical and surgical procedures include pre-procedure, intra-procedure, and post-procedure work. When multiple procedures are performed at the same patient encounter, there is often overlap of the pre-procedure and post-procedure work. Payment methodologies for surgical procedures account for the overlap of the pre-procedure ...
What is the modifier indicator in CCI?
Each CCI code pair edit includes a correct coding modifier indicator of “0” or “1,” as indicated by a superscript placed to the right of the column 2 code.
Can you use modifiers for separate procedures?
If, however, the two procedures are separate and distinct, you may be able to use a modifier to override the edit and be paid for both procedures. Separate, distinct procedures may include: different session. different procedure or surgery. different site or organ system.
Does CPT have multiple procedures?
Multiple procedure rule does not apply to all CPT® codes.
Can NCCI codes be bundled?
In some cases, the National Correct Coding Initiative (NCCI) may impose edits that “bundle” codes to one another. If the NCCI lists any two codes as “mutually exclusive,” or pairs them as “column 1” and “column 2” codes, the procedures are bundled and normally are not reported together.