How to file a Medicare claim
- Fill out a Patient’s Request for Medical Payment form. You can also pick up a form at your local Social Security office. ...
- Get an itemized bill for your medical treatment. Your itemized bill is the evidence for the Medicare claim. ...
- Write a letter and add supporting documents to your claim. ...
- File your claim for Medicare reimbursement. ...
Full Answer
How to manually file a claim with Medicare?
- A copy of the bill
- Your Medicare information
- The doctor’s NPN (call the doctor who treated you and ask them for it)
How long do you have to submit a claim to Medicare?
Medicare Part A and B claims are submitted directly to Medicare by the healthcare provider (such as a doctor, hospital, or lab). Medicare then takes approximately 30 days to process and settle each claim. However, if there are queries or issues with the claim, the process can be a lot longer.
Do I need to file any claims with Medicare?
You usually don’t have to file a Medicare claim. Doctors or hospitals typically file Original Medicare claims for you. Private insurers that administer Medicare Advantage and Part D plans handle those claims. In the rare cases when you have to file a claim, Medicare provides a form to download and mail in.
What if Medicare denies my claim?
- Your bill will be sent directly to Medicare.
- The appeal must be filed within 120 days of receiving the Medicare Summary Notice (MSN) that shows that your claim was denied.
- If you disagree with a Medicare coverage decision in the MSN, you can appeal the decision.
How do I get reimbursed from Medicare?
How to Get Reimbursed From Medicare. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request.
Can I submit a claim directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Can you submit Medicare claims online?
Submit your completed Patient's Request for Medical Payment form, itemized medical bill or bills, and any supporting documents to your state's Medicare contractor. All claims must be submitted by mail; you can't file a Medicare claim online.
Does Medicare reimburse patients directly?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Where do I send Medicare claims?
You can submit your claims for Medicare online through your “MyMedicare.gov” account. Or, you can send your paper claim to the address on the Medicare Summary Notice.
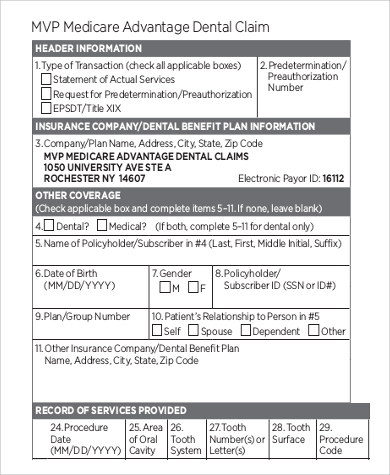
What form is used to send claims to Medicare?
Form CMS-1500Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
How long does a Medicare rebate take to process?
As long as your details and bank account is registered with Medicare we should be able to process this for you immediately after taking payment for your consultation. Your rebate will usually be back in your bank account within one to two business days.
What are Medicare reimbursement rates?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
How does Medicare Part B reimbursement work?
The Medicare Part B Reimbursement program reimburses the cost of eligible retirees' Medicare Part B premiums using funds from the retiree's Sick Leave Bank. The Medicare Part B reimbursement payments are not taxable to the retiree.
How do reimbursements work in healthcare?
Healthcare reimbursement describes the payment that your hospital, healthcare provider, diagnostic facility, or other healthcare providers receive for giving you a medical service. Often, your health insurer or a government payer covers the cost of all or part of your healthcare.
How Do I File a Medicare Reimbursement Claim?
To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor.
What To Submit With The Claim
When filling out the form, you must choose the service type then provide the following information:
Where to Send Your Medicare Claim
Each state has a different address to send your claim. There are two places where you can find the address. You can find the address on the claim form on page two, or on your quarterly Medicare Summary Notice.
What if My Healthcare Provider is Not Sending the Claims Promptly?
The first thing you should do is call the provider and ask them to send your claim. If they do not file the claim, call Medicare and find out how much time is left to file the claim. If it’s close to the end of the allowed time and your healthcare provider has not filed the claim, you should go ahead and file the claim.
FAQs
When a claim is submitted to Medicare, it should come straight from the doctor or other provider of services. If for some reason they don’t submit the claim on your behalf, then you can call Medicare and submit it yourself. You can also submit the claim online.
What is Medicare reimbursement?
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.
What does Medicare look up after a CPT?
After the treatment they may look up the CPT code for the procedure then file the necessary claim to Medicare. In return, Medicare would look up the allowable charge for that procedure and then reimburse the doctor the amount of money.
How much can a doctor bill for Medicare?
For example, if you got a service that normally costs $500 and Medicare pays $250 then the doctor cannot bill you more than $287.50 (15% more than $250).
How to file a claim for Medicare?
How to File a Medicare Claim Yourself. If you need to file your own Medicare claim, you’ll need to fill out a Patient Request for Medical Payment Form, the 1490S. Make sure it’s filed no later than 1 full calendar year after the date of service. Medicare can’t pay its share if the submission doesn’t happen within 12 months.
How long does it take for Medicare to process a claim?
How Are Medicare Claims Processed? Your doctor will submit the claims. Then, Medicare will take about 30 days to process the claim. When it comes to Part A services, Medicare will pay the hospital directly. But, with Part B claims payment depends on whether or not the doctor accepts Medicare assignment.
How long does it take to get a Medicare summary notice?
Most claims are sent in within 24 hours of processing. You can even get your Medicare Summary Notice online; sign up to receive an e-Medicare Summary Notice and get monthly emails that link you to your details. With this, you get the most up to date information and no waiting 3 months for a letter.
Can a doctor submit a claim to Medicare?
But, in some instances, like foreign travel or doctors that don’t accept assignment, you’ll file the claim. If you receive an Advance Beneficiary Notice of Noncoverage and decide to proceed, it’s best to request your doctor submit the claim to Medicare before billing you.
Is Medicare always primary?
Medicare isn’t always primary. In this instance where Medicare is secondary, you’ll bill the primary insurance company before Medicare. Then, you can submit an Explanation of Benefits from the primary payor with the claim. The primary payer must process the claim first, and if they don’t, your doctor may bill Medicare.
Can Medicare help you complete a claim?
Medicare is trying to make it simple for beneficiaries; there are many tools that can help you complete any Medicare form or document on your own. Although, if you find that you need help with your claim, don’t hesitate to contact someone.
Can Medicare pay your share?
Medicare can’t pay its share if the submission doesn’t happen within 12 months. You can log in to MyMedicare.gov and view your claims to ensure they are being filed in a timely fashion. If your claims aren’t being taken care of, contact the doctor and ask them to file the claim.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What to do if a pharmacist says a drug is not covered?
You may need to file a coverage determination request and seek reimbursement.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Before Filing a Medicare Claim
Before filing a claim on your own, Medicare.gov says that participants should first contact the healthcare provider or medical equipment supplier directly and ask them to file a claim for reimbursement. They are required by law to do this for all Original Medicare participant services.
How to File a Basic Claim for Medicare Reimbursement
If you do need to file a claim, the form you need to use is called a Patient’s Request for Medical Payment (form CMS-1490S).
Special Medicare Reimbursement Claim Instructions
There are some instances where Medicare provides different claim submission instructions other than those included with the standard Patient’s Request for Medical Payment. While they all use the same form, what changes from one type of claim to the other is where they’re sent for processing.
Checking the Status of Your Medicare Claim
Although Medicare.gov indicates that most claims are processed within 60 days, if you’d like to check the status of your claim after it has been filed, the way to go about this is dependent upon which part of Medicare the claim is for.
If Your Medicare Claim Was Denied
If a service or supply claim is denied by Medicare, the first step is to contact the billing agency (whether that is a doctor’s office or medical supply company) and verify that the information they submitted was correct. If not, ask them to resubmit the claim with the corrected information.
Helping a Loved One with a Medicare Reimbursement Claim
In some cases, Medicare participants may ask a loved one or other trusted person for help with completing and submitting a Medicare claim, or to check its status. In this instance, an Authorization to Disclose Personal Health Information form must be completed first.
How to Reduce Out-of-Pocket Healthcare Expenses
The goal of filing a claim for Medicare reimbursement is to ensure that costs covered under the Medicare program are paid according to your specific plan or policy. This reduces your out-of-pocket expenses related to mental and physical healthcare.
How long does it take for Medicare to pay your claim?
Any Medicare claims must be submitted within a year (12 months) of the date you received a service, such as a medical procedure. If a claim is not filed within this time limit, Medicare cannot pay its share. One reason to make sure that Medicare processes a claim is to ensure that deductible amounts are credited to you.
How to check if I have Medicare?
To learn about Medicare plans you may be eligible for, you can: 1 Contact the Medicare plan directly. 2 Call 1-800-MEDICARE (1-800-633-4227), TTY users 1-877-486-2048; 24 hours a day, 7 days a week. 3 Contact a licensed insurance agency such as Medicare Consumer Guide’s parent company, eHealth.#N#Call eHealth's licensed insurance agents at 888-391-2659, TTY users 711. We are available Mon - Fri, 8am - 8pm ET. You may receive a messaging service on weekends and holidays from February 15 through September 30. Please leave a message and your call will be returned the next business day.#N#Or enter your zip code where requested on this page to see quote.
What does it mean when a doctor accepts Medicare?
When your doctor accepts Medicare assignment, it also means she or he agrees not to bill you for more than the Medicare deductible and/or coinsurance. Private insurance companies contracted with Medicare may bill Medicare differently.
Why do you need to contact your doctor about Medicare?
One reason to make sure that Medicare processes a claim is to ensure that deductible amounts are credited to you. It may be worthwhile for you to contact your doctor’s office to remind them that you’re waiting for them to file a claim.
Can you appeal a Medicare Advantage plan?
If you have prescription drug coverage–whether it’s through a stand-alone Medicare Part D Prescription Drug Plan, or through a Medicare Advantage Prescription Drug plan–and your plan doesn’t cover a drug prescribed for you , you can file an appeal to get your plan to cover the prescription drug or to get it at a lower cost.
How to file a claim for Medicare Part B?
To file a claim, fill out the Patient Request for Medical Payment form and send the completed form to your state’s Medicare contractor. Instructions for submitting your claim vary depending on the type of claim you’re filing: Claims for Medicare Part B services. Claims for durable medical equipment (DME)
How to find Medicare Advantage plan?
To learn more about Medicare or to find Medicare Advantage plans in your area, speak with a licensed insurance agent by calling. 1-800-557-6059 . 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week. 1 Medicare.gov. Lower costs with assignment.
How to contact Medicare if you don't accept Medicare?
Speak with a licensed insurance agent. 1-800-557-6059 | TTY 711, 24/7. If you go to a provider that does not accept Medicare assignment, you may have to pay for the service out of pocket and then file a claim to be reimbursed by Medicare.
What are the benefits of Medicare Advantage?
Still, there are several advantages to having a Medicare Advantage plan. For instance, many Medicare Advantage plans can offer benefits that aren’t covered by Original Medicare, including: 1 Prescription drug coverage 2 Dental coverage 3 Vision coverage 4 Hearing coverage 5 Health and wellness program benefits, such as membership to SilverSneakers
What is Medicare assignment?
Providers that accept Medicare assignment are required by law to accept the Medicare-approved amount as full payment for covered services. Providers that don’t accept assignment can charge up to 15 percent more for covered services, which you are typically responsible for paying. 1
What should be included in a medical bill?
The bill should include: The date of service. A description of each service. The charge for each service. The place of service. Diagnosis. Name and address of the provider. A letter explaining your reason for the claim, including why you received the medical care from the provider.
Does Medicare have an out-of-pocket maximum?
Original Medicare does not have an out-of-pocket maximum.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
Who has the right to appeal a demand letter?
This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the right to appeal.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.

When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…